Abstract
Purpose
This prospective study with 10-year follow-up aimed to analyze potential impact of body mass index (BMI) and gamma gap on heart failure and mortality rate in older patients with coronary artery disease (CAD).
Methods
There were 987 consecutive older patients with CAD included and divided into four groups according to BMI and gamma gap levels.
Results
Median age was 86 years. The highest proportion of heart failure (46.2%) and the highest mortality rate (84.4%) was observed in patients with low BMI and high gamma gap, whereas the lowest proportion of heart failure (18.9%) and the lowest mortality rate (62.9%) was observed in those with high BMI and low gamma gap. After full adjustment in multivariate Logistic regression analysis, heart failure was most common in patients with low BMI and high gamma gap compared with those with high BMI and low gamma gap (hazard ratio [HR]: 2.82, 95% confidence interval [CI]: 1.79–4.48, P < 0.05). Meanwhile, multivariate Cox regression analysis showed that mortality rate was the highest in those with low BMI and high gamma gap compared with patients with high BMI and low gamma gap (HR: 1.65, 95% CI: 1.32–2.07, P < 0.05).
Conclusion
The combination of low BMI and high gamma gap could further promote heart failure and increase mortality rate in older patients with CAD. Future studies should explore the underlying mechanisms linking low BMI, high gamma gap, and mortality rate, as well as the potential benefits of nutritional and immunological interventions to improve health prognosis in older patients with CAD.
Similar content being viewed by others
Introduction
High body mass index (BMI) is considered a high-risk factor for the occurrence of cardiovascular disease (CAD) [1]. Previous research has reported that high BMI leads to a 13.5% mortality rate among patients with CAD [2]. However, other scholars have suggested that the overall mortality rate of patients with obesity with CAD is lower than that of normal-weight individuals, which is known as the obesity paradox [3], but its underlying reasons are unclear [4].
Gamma gap, also known as globulin fraction, defined as the difference between the serum total protein levels and the serum albumin levels, has been reported to be associated with all-cause mortality rate in several studies [5, 6]. However, there is no information regarding the association between gamma gap and mortality rate in different BMI categories. Mortality rate may vary according to different gamma gap and BMI categories. Therefore, in this prospective study with 10-year follow-up, we aimed to analyze potential impact of BMI and gamma gap on heart failure and mortality rate in older patients with CAD.
Method
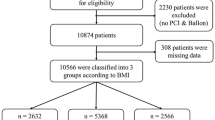
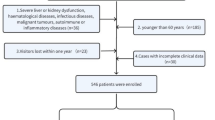
Study population
This prospective study included 987 consecutive patients with CAD aged 60 years or older in Department of Geriatric Cardiology, Chinese People’s Liberation Army (PLA) General Hospital. Chinese PLA General Hospital is their designated hospital with comprehensive medical treatment and final death records, which makes it easier for us to track them effectively and judge endpoint accurately. The diagnosis of CAD was made by the chief physician based on medical history, angina symptoms, cardiac biomarkers, and specific tests, such as electrocardiogram (rest/exercise), echocardiography, nuclear imaging, computed tomography, and coronary angiography, based on the guidelines of the American College of Cardiology (ACC)/American Heart Association (AHA)/European Society of Cardiology (ESC) [7, 8]. Exclusion criteria: severe aortic stenosis, expected heart transplantation, and ventricular assist device. This study was approved by the Ethics Committee of Chinese PLA General Hospital in Beijing, China. Informed consent was obtained from participants at the time of admission, and the study followed the principles of the Helsinki Declaration of 1975.
Baseline characteristics
The available baseline characteristics analyzed included demographics (age and gender), physical examination (height, weight, heart rate, systolic blood pressure, and diastolic blood pressure [SBP and DBP]), laboratory measurements (hemoglobin, albumin, total cholesterol, high-density lipoprotein cholesterol [HDL-C], low-density lipoprotein cholesterol [LDL-C], fasting plasma glucose [FPG], creatinine, C-reactive protein [CRP], and N-terminal pro-B-type natriuretic peptide [NT-proBNP]). BMI was calculated as body weight (kg) divided by the square of height (m). Gamma gap, also known as globulin fraction, was defined as the serum total protein levels minus the serum albumin levels [5, 6]. BMI ≥ 25 kg/m2 was defined as high BMI, and gamma gap ≥30 g/L was defined as high gamma gap. Data management involved experienced and trained doctors who recorded the data in a database. Other doctors performed logical checks to ensure the accuracy of the database.
Follow-up and study endpoints
The endpoint of this study was all-cause mortality. Considering the higher incidence of multi-organ failure in older patients and the priority of all-cause mortality in prognostic studies, all-cause mortality was the predetermined endpoint of this study. Follow-up continued for almost 10 years, and no patient lost to the follow-up. Follow-up results were directly obtained from medical records and telephone interviews. Deaths were determined by legal documents of death time and place.
Statistical analysis
Continuous variables with skewed distribution were presented as medians and interquartile ranges (IQR), while categorical variables were presented as frequencies and percentages. Kruskal-Wallis test was used to analyze potential difference of continuous variables with skewed distribution. Chi-square test was used to test potential difference of categorical variables. Kaplan-Meier curve was used to describe cumulative survival of patients with different BMI or gamma gap levels. Multivariate Logistic regression analysis was used to examine potential impact of BMI and gamma gap on heart failure. Multivariate Cox regression analysis was used to examine potential impact of BMI and gamma gap on mortality rate. All analyses were performed using IBM SPSS 22.0 software. A P value of <0.05 was considered significant.
Result
Characteristic description of patients with different BMI or gamma gap levels
Median age of 987 patients was 86 years (IQR: 82–90 years). Patients with high BMI accounted for 41.9% (414 patients), and those with high gamma gap accounted for 31.8% (314 patients). The average follow-up period of this study was 1836 days (median: 1871 days [IQR: 384–3225 days]). Age, gender, BMI, heart rate, DBP, hemoglobin, albumin, HDL-C, FPG, creatinine, CRP, NT-proBNP, and gamma gap had significant distinction in patients with different BMI or gamma gap levels (all P < 0.05, Table 1). The highest proportion of heart failure (46.2%) and the highest mortality rate (84.4%) was observed in patients with low BMI and high gamma gap, whereas the lowest proportion of heart failure (18.9%) and the lowest mortality rate (62.9%) was observed in those with high BMI and low gamma gap.
A synergistic impact of BMI and gamma gap on heart failure
High BMI was negatively correlated with heart failure (r: -0.13, P < 0.001). Proportion of heart failure was significantly higher in patients with low BMI than that in those with high BMI (34.9% vs 22.9%, P < 0.001). High gamma gap was positively correlated with heart failure (r: 0.16, P < 0.001). Proportion of heart failure was significantly higher in patients with high gamma gap than that in those with low gamma gap (40.4% vs 25.0%, P < 0.001). Multivariate Logistic regression analysis showed that compared with patients with low BMI, those with high BMI had a significantly lower proportion of heart failure (hazard ratio [HR]: 0.56, 95% confidence interval [CI]: 0.42–0.74, P < 0.001). Compared with patients with low gamma gap, those with high gamma gap had a significantly higher proportion of heart failure (HR: 2.04, 95% CI: 1.54–2.72, P < 0.001).
Compared with patients with high BMI and low gamma gap, those with low BMI and low gamma gap (HR: 1.79, 95% Cl: 1.24–2.59) or those with high BMI and high gamma gap had significantly higher proportions of heart failure (HR: 2.03, 95% CI: 1.26–3.26), and those with low BMI and high gamma gap had the highest proportion of heart failure (HR: 3.70, 95% CI: 2.44–5.59, all P < 0.05, Table 2). After adjusting for age and gender, the results showed that compared with patients with high BMI and low gamma gap, heart failure was significantly more common in those with low BMI and low gamma gap (HR: 1.76, 95% CI: 1.20–2.56) or in those with high BMI and high gamma gap (HR: 1.82, 95% CI: 1.11–2.99), and most common in those with low BMI and high gamma gap (HR: 3.76, 95% CI: 2.45–5.77, all P < 0.05). After adjusting for all factors with significant distinction shown in Table 1, compared with patients with high BMI and low gamma gap, heart failure was more common in those with low BMI and low gamma gap (HR: 1.62, 95% CI: 1.08–2.42), and most common in those with low BMI and high gamma gap (HR: 2.82, 95% CI: 1.79–4.48, all P < 0.05).
A synergistic impact of BMI and gamma gap on mortality rate
High BMI was negatively correlated with mortality rate (r: -0.07, P < 0.05). Mortality rate was significantly higher in patients with low BMI than in those with high BMI (75.2% vs 69.1%, P < 0.05). High gamma gap was positively correlated with mortality rate (r: 0.17, P < 0.001). Mortality rate was significantly higher in patients with high gamma gap than in those with low gamma gap (83.8% vs 67.5%, P < 0.001). Kaplan-Meier analysis showed significant difference in survival rate between different groups (P < 0.001, Fig. 1). Multivariate Cox regression analysis showed that compared with patients with low BMI, those with high BMI had a significantly lower mortality rate (HR: 0.80, 95% CI: 0.69–0.93, P < 0.05). Compared with patients with low gamma gap, those with high gamma gap had a significantly higher mortality rate (HR: 1.81, 95% CI: 1.55–2.10, P < 0.001).
Compared with patients with high BMI and low gamma gap, those with low gamma gap and low BMI (HR:1.25, 95% CI: 1.04–1.51) or those with high BMI and high gamma gap (HR: 1.78, 95% CI: 1.40–2.27) had higher mortality rates, and those with low BMI and high gamma gap had the highest mortality rate (HR: 2.30, 95% CI: 1.85–2.85, all P < 0.05, Table 3). After adjusting for age and gender, the results showed that compared with patients with high BMI and low gamma gap, mortality rate was significantly higher in those with high BMI and high gamma gap (HR: 1.68, 95% CI: 1.32–2.14), and the highest in those with low BMI and high gamma gap (HR: 2.20, 95% CI: 1.78–2.74, all P < 0.001). After adjusting for all factors with significant distinction shown in Table 1, compared with patients with high BMI and low gamma gap, mortality rate was significantly higher in those with high BMI and high gamma gap (HR: 1.51, 95% CI: 1.19–1.93), and the highest in those with low BMI and high gamma gap (HR: 1.65, 95% CI: 1.32–2.07, all P < 0.05).
Discussion
In this prospective study with 10-year follow-up, both low BMI and high gamma gap contribute to heart failure and mortality rate in older patients with CAD, suggesting that low BMI and high gamma gap play a synergistic impact on heart failure and mortality rate.
In this study, we found that low BMI and high gamma gap were associated with an increased risk of mortality rate, even after adjusting for age, gender, and other potential confounding factors. The association between BMI and mortality rate is inconsistent, which is considered as obesity paradox [9, 10]. Some studies have suggested that overweight was an important risk factor for the development of heart failure and mortality rate [11, 12], but other researches realized that high BMI had a protective impact on the actual long-term prognosis in patients with CAD [13,14,15,16]. Our findings suggested that high BMI is negatively associated with the development of heart failure and mortality rate in older patients with CAD.
The association between gamma gap and mortality rate in older patients with CAD has not been widely studied, not to say the underlying mechanisms. In this study, we found that high gamma gap resulted in increased heart failure and mortality rate in older patients with CAD. Elevated gamma gap has been realized to increase mortality rate in populations of nonagenarians and centenarians [17, 18]. High gamma gap suggests the presence of systemic inflammation and immune dysfunction [19, 20], which are important factors contributing to the development of atherosclerosis [21, 22]. An elevated gamma gap may result from increased globulin levels or decreased albumin levels. Decreased albumin levels have been shown to be a risk factor for all-cause mortality. Studies have indicated that decreased albumin levels are associated with higher mortality rate in octogenarians [23] and can predict long-term mortality rate in patients with dual-chamber permanent pacemakers [24]. Immune activation and pro-inflammatory cytokines play important roles in the progression of heart failure [25, 26], and elevated circulating globulin levels are a predictor of heart failure and mortality rate [27, 28].
Our finding of a synergistic impact of low BMI and high gamma gap on heart failure and mortality risk is still novel and warrants further investigation. One possible explanation is that low BMI and high gamma gap may reflect a state of chronic malnutrition and inflammation, which could lead to a higher risk of adverse prognosis. There is another potential mechanism may explain the relationship between BMI and gamma gap. The large number of activated macrophages in the adipose tissue increases the catabolism of globulin [29]. The half-life of globulin in individuals with obesity is shorter compared with lean individuals [30].
Conclusion
This prospective study with 10-year follow-up provided new evidence that the combination of low BMI and high gamma gap could further promote heart failure and increase mortality rate in older patients with CAD. Future studies should explore the underlying mechanisms linking low BMI, high gamma gap, and mortality rate, as well as the potential benefits of nutritional and immunological interventions to improve health prognosis in older patients with CAD.
Data availability
All data and material are available under the requirement to the corresponding authors.
References
Fu S, Luo L, Ye P, Liu Y, Zhu B, Bai Y, et al. The abilities of new anthropometric indices in identifying cardiometabolic abnormalities, and influence of residence area and lifestyle on these anthropometric indices in a Chinese community-dwelling population. Clin Interv Aging. 2014;9:179–89.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145–58.
Şaylık F, Çınar T, Hayıroğlu Mİ. Effect of the obesity paradox on mortality in patients with acute coronary syndrome: a comprehensive meta-analysis of the literature. Balkan Med J. 2023;40:93–103.
Qu Y, Yang J, Zhang F, Li C, Dai Y, Yang H, et al. Relationship between body mass index and outcomes of coronary artery disease in Asian population: Insight from the FOCUS registry. Int J Cardiol. 2020;300:262–7.
Edwards MK, Loprinzi PD. The Association of Estimated Cardiorespiratory Fitness on mortality risk among those with an elevated gamma gap. Int J Cardiol. 2017;227:508–10.
Juraschek SP, Moliterno AR, Checkley W, Miller ER. The Gamma Gap and All-Cause Mortality. PLoS One. 2015;10:e0143494.
Skalidis EI, Vardas PE. Guidelines on the management of stable angina pectoris. Eur Heart J. 2006;27:2606.
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50:e1–157.
Lavie CJ, Milani RV. Obesity and cardiovascular disease: the hippocrates paradox? J Am Coll Cardiol. 2003;42:677–9.
Hwang I-C, Choi H-M, Yoon YE, Park JJ, Park J-B, Park J-H, et al. Body Mass Index, Muscle Mass, and All-Cause Mortality in Patients With Acute Heart Failure: The Obesity Paradox Revisited. Int J Heart Fail. 2022;4:95–109.
Kenchaiah S, Evans JC, Levy D, Wilson PWF, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13.
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–73.
Kenchaiah S, Pocock SJ, Wang D, Finn PV, Zornoff LAM, Skali H, et al. Body mass index and prognosis in patients with chronic heart failure: insights from the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation. 2007;116:627–36.
Fonarow GC, Srikanthan P, Costanzo MR, Cintron GB, Lopatin M. ADHERE Scientific Advisory Committee and Investigators. An obesity paradox in acute heart failure: analysis of body mass index and inhospital mortality for 108,927 patients in the Acute Decompensated Heart Failure National Registry. Am Heart J. 2007;153:74–81.
Stienen S, Ferreira JP, Girerd N, Duarte K, Lamiral Z, McMurray JJV, et al. Mean BMI, visit-to-visit BMI variability and BMI changes during follow-up in patients with acute myocardial infarction with systolic dysfunction and/or heart failure: insights from the High-Risk Myocardial Infarction Initiative. Clin Res Cardiol. 2019;108:1215–25.
Yui H, Ebisawa S, Miura T, Nakamura C, Maruyama S, Kashiwagi D, et al. Impact of changes in body mass index after percutaneous coronary intervention on long-term outcomes in patients with coronary artery disease. Heart Vessels. 2020;35:1657–63.
Yang M, Xie L, Liu X, Hao Q, Jiang J, Dong B. The gamma gap predicts 4-year all-cause mortality among nonagenarians and centenarians. Sci Rep. 2018;8:1046.
Dalle S, Rossmeislova L, Koppo K. The Role of Inflammation in Age-Related Sarcopenia. Front Physiol. 2017;8:1045.
Guo X, Ma L. Inflammation in coronary artery disease-clinical implications of novel HDL-cholesterol-related inflammatory parameters as predictors. Coron Artery Dis. 2023;34:66–77.
Pai AY, Sy J, Kim J, Kleine C-E, Edward J, Hsiung J-T, et al. Association of serum globulin with all-cause mortality in incident hemodialysis patients. Nephrol Dial Transplant. 2021;37:1993–2003.
Meng Q, Liu H, Liu J, Pang Y, Liu Q. Advances in immunotherapy modalities for atherosclerosis. Front Pharmacol. 2022;13:1079185.
Pattarabanjird T, Li C, McNamara C. B Cells in Atherosclerosis: Mechanisms and Potential Clinical Applications. JACC Basic Transl Sci. 2021;6:546–63.
Hayıroğlu Mİ, Çınar T, Çinier G, Yüksel G, Pay L, Keskin K, et al. Cardiac variables associated with atrial fibrillation occurrence and mortality in octogenarians implanted with dual chamber permanent pacemakers. Aging Clin Exp Res. 2022;34:2533–9.
Hayıroğlu Mİ, Çınar T, Çinier G, Yüksel G, Pay L, Keskin K, et al. Prognostic value of serum albumin for long-term mortality in patients with dual-chamber permanent pacemakers. Biomark Med. 2022;16:341–8.
Anker SD, von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004;90:464–70.
Çinier G, Hayıroğlu Mİ, Kolak Z, Tezen O, Yumurtaş AÇ, Pay L, et al. The value of C-reactive protein-to-albumin ratio in predicting long-term mortality among HFrEF patients with implantable cardiac defibrillators. Eur J Clin Invest. 2021;51:e13550.
Niedziela JT, Hudzik B, Szygula-Jurkiewicz B, Nowak JU, Polonski L, Gasior M, et al. Albumin-to-globulin ratio as an independent predictor of mortality in chronic heart failure. Biomark Med. 2018;12:749–57.
van den Hoogen P, de Jager SCA, Huibers MMH, Schoneveld AH, Puspitasari YM, Valstar GB, et al. Increased circulating IgG levels, myocardial immune cells and IgG deposits support a role for an immune response in pre- and end-stage heart failure. J Cell Mol Med. 2019;23:7505–16.
Fu S, Luo L, Ye P, Liu Y, Zhu B, Zheng J, et al. Overall and abdominal obesity indicators had different association with central arterial stiffness and hemodynamics independent of age, sex, blood pressure, glucose, and lipids in Chinese community-dwelling adults. Clin Interv Aging. 2013;8:1579–84.
Brunetti L, Chapy H, Nahass RG, Moore R, Wassef A, Adler D, et al. Relationship between Body Composition and Serum Immunoglobulin Concentrations after Administration of Intravenous Immune Globulin–Preclinical and Clinical Evidence. Pharmaceutics. 2023;15:510.
Acknowledgements
We appreciate all those who participated in the present study for their continued cooperation.
Funding
This work was supported by grants from the Natural Science Foundation of Hainan Province (821QN389, 821MS112, 822MS193, 822MS198, 820MS126, 820QN383), the Excellent Youth Incubation Program of Chinese People’s Liberation Army General Hospital (2020-YQPY-007), the Military Medical Science and Technology Youth Incubation Program (20QNPY110, 19QNP060), the National Key R&D Program of China (2018YFC2000400), the National S&T Resource Sharing Service Platform Project of China (YCZYPT[2018]07), the Scientific Research Project of Health Industry in Hainan Province (22A200352), the Specific Research Fund of Innovation Platform for Academicians of Hainan Province (YSPTZX202216), the Medical Big Data R&D Project of Chinese People’s Liberation Army General Hospital (MBD2018030), the Traditional Chinese Medicine Service Capacity Cultivating Program (2021ZY053), the Heatstroke Treatment and Research Center of PLA (413EGZ1D10), the Simulation Training for Treatment of Heat Stroke, and the Major Science and Technology Programme of Hainan Province (ZDKJ2019012). The sponsors had no role in the design, conduct, interpretation, review, approval or control of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design, conducted the data collection and analyses, and drafted the paper. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The current study received the approval from Ethics Committee of Chinese People’s Liberation Army General Hospital (Beijing, China). Prior to the current study, written informed consents were required from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, X., Zheng, Y., Li, D. et al. A synergistic impact of body mass index and gamma gap on heart failure and mortality rate among older patients with coronary artery disease: a prospective study with 10-year follow-up. Nutr. Diabetes 13, 25 (2023). https://doi.org/10.1038/s41387-023-00255-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41387-023-00255-1