Abstract
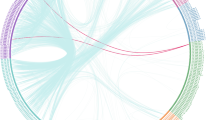
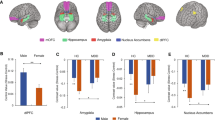
Sex-specific neurobiological changes have been implicated in Major Depressive Disorder (MDD). Dysfunctions of the default mode network (DMN), salience network (SN) and frontoparietal network (FPN) are critical neural characteristics of MDD, however, the potential moderating role of sex on resting-state network dynamics in MDD has not been sufficiently evaluated. Thus, resting-state functional magnetic resonance imaging (fMRI) data were collected from 138 unmedicated patients with first-episode MDD (55 males) and 243 healthy controls (HCs; 106 males). Recurring functional network co-activation patterns (CAPs) were extracted, and time spent in each CAP (the total amount of volumes associated to a CAP), persistence (the average number of consecutive volumes linked to a CAP), and transitions across CAPs involving the SN, DMN and FPN were quantified. Relative to HCs, MDD patients exhibited greater persistence in a CAP involving activation of the DMN and deactivation of the FPN (DMN + FPN-). In addition, relative to the sex-matched HCs, the male MDD group spent more time in two CAPs involving the SN and DMN (i.e., DMN + SN- and DMN-SN + ) and transitioned more frequently from the DMN + FPN- CAP to the DMN + SN- CAP relative to the male HC group. Conversely, the female MDD group showed less persistence in the DMN + SN- CAP relative to the female HC group. Our findings highlight that the imbalance between SN and DMN could be a neurobiological marker supporting sex differences in MDD. Moreover, the dominance of the DMN accompanied by the deactivation of the FPN could be a sex-independent neurobiological correlate related to depression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. 2017;143:783–822.
Eid RS, Gobinath AR, Galea LAM. Sex differences in depression: Insights from clinical and preclinical studies. Prog Neurobiol. 2019;176:86–102.
Labonté B, Engmann O, Purushothaman I, Menard C, Wang J, Tan C, et al. Sex-specific transcriptional signatures in human depression. Nat Med .2017;23:1102–11.
Bangasser DA, Cuarenta A. Sex differences in anxiety and depression: circuits and mechanisms. Nat Rev Neurosci. 2021;22:674–84.
Kong L, Chen K, Womer F, Jiang W, Luo X, Driesen N, et al. Sex differences of gray matter morphology in cortico-limbic-striatal neural system in major depressive disorder. J Psychiatr Res. 2013;47:733–9.
Hu X, Zhang L, Liang K, Cao L, Liu J, Li H, et al. Sex-specific alterations of cortical morphometry in treatment-naïve patients with major depressive disorder. Neuropsychopharmacology. 2022;47:2002–9.
Briceño EM, Rapport LJ, Kassel MT, Bieliauskas LA, Zubieta J-K, Weisenbach SL, et al. Age and gender modulate the neural circuitry supporting facial emotion processing in adults with major depressive disorder. Am J Geriatr Psychiatry 2015;23:304–13.
Young KD, Bodurka J, Drevets WC. Functional neuroimaging of sex differences in autobiographical memory recall in depression. Psychol Med. 2017;47:2640–52.
Dong D, Ironside M, Belleau EL, Sun X, Cheng C, Xiong G, et al. Sex-specific neural responses to acute psychosocial stress in depression. Transl Psychiatry 2022;12:1–8.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Dong D, Ming Q, Zhong X, Pu W, Zhang X, Jiang Y, et al. State-independent alterations of intrinsic brain network in current and remitted depression. Prog Neuro-Psychopharmacol Biol Psychiatry 2019;89:475–80.
Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry 2015;72:603–11.
Scalabrini A, Vai B, Poletti S, Damiani S, Mucci C, Colombo C, et al. All roads lead to the default-mode network—global source of DMN abnormalities in major depressive disorder. Neuropsychopharmacology 2020;45:2058–69.
Yan C-G, Chen X, Li L, Castellanos FX, Bai T-J, Bo Q-J, et al. Reduced default mode network functional connectivity in patients with recurrent major depressive disorder. Proc Natl Acad Sci. 2019;116:9078–83.
Allen EA, Erhardt EB, Damaraju E, Gruner W, Segall JM, Silva RF, et al. A baseline for the multivariate comparison of resting-state networks. Front Syst Neurosci. 2011;5:2.
Satterthwaite TD, Wolf DH, Roalf DR, Ruparel K, Erus G, Vandekar S, et al. Linked sex differences in cognition and functional connectivity in youth. Cereb Cortex 2015;25:2383–94.
Padgaonkar NT, Lawrence KE, Hernandez LM, Green SA, Galván A, Dapretto M. Sex differences in internalizing symptoms and amygdala functional connectivity in neurotypical youth. Dev Cogn Neurosci. 2020;44:100797.
Talishinsky A, Downar J, Vértes PE, Seidlitz J, Dunlop K, Lynch CJ, et al. Regional gene expression signatures are associated with sex-specific functional connectivity changes in depression. Nat Commun. 2022;13:1–20.
Bolton TAW, Morgenroth E, Preti MG, Van De Ville D. Tapping into multi-faceted human behavior and psychopathology using fMRI brain dynamics. Trends Neurosci. 2020;43:667–80.
Liu X, Duyn JH. Time-varying functional network information extracted from brief instances of spontaneous brain activity. Proc Natl Acad Sci. 2013;110:4392–7.
Lurie DJ, Kessler D, Bassett DS, Betzel RF, Breakspear M, Kheilholz S, et al. Questions and controversies in the study of time-varying functional connectivity in resting fMRI. Netw Neurosci. 2020;4:30–69.
Yan B, Xu X, Liu M, Zheng K, Liu J, Li J, et al. Quantitative identification of major depression based on resting-state dynamic functional connectivity: a machine learning approach. Front Neurosci. 2020;14:191.
Belleau EL, Bolton TAW, Kaiser RH, Clegg R, Cárdenas E, Goer F, et al. Resting state brain dynamics: Associations with childhood sexual abuse and major depressive disorder. NeuroImage Clin. 2022;36:103164.
Kaiser RH, Kang MS, Lew Y, Van Der Feen J, Aguirre B, Clegg R, et al. Abnormal frontoinsular-default network dynamics in adolescent depression and rumination: a preliminary resting-state co-activation pattern analysis. Neuropsychopharmacology 2019;44:1604–12.
Liu X, Zhang N, Chang C, Duyn JH. Co-activation patterns in resting-state fMRI signals. Neuroimage 2018;180:485–94.
Bolton TAW, Tuleasca C, Wotruba D, Rey G, Dhanis H, Gauthier B, et al. TbCAPs: a toolbox for co-activation pattern analysis. Neuroimage 2020;211:116621.
Esteban O, Markiewicz CJ, Blair RW, Moodie CA, Isik AI, Erramuzpe A, et al. fMRIPrep: a robust preprocessing pipeline for functional MRI. Nat Methods 2019;16:111–6.
Gorgolewski K, Burns CD, Madison C, Clark D, Halchenko YO, Waskom ML, et al. Nipype: a flexible, lightweight and extensible neuroimaging data processing framework in python. Front Neuroinform. 2011;5:13.
Pruim RHR, Mennes M, van Rooij D, Llera A, Buitelaar JK, Beckmann CF. ICA-AROMA: A robust ICA-based strategy for removing motion artifacts from fMRI data. Neuroimage 2015;112:267–77.
Tian Y, Margulies DS, Breakspear M, Zalesky A. Topographic organization of the human subcortex unveiled with functional connectivity gradients. Nat Neurosci. 2020;23:1421–32.
Hamilton JP, Furman DJ, Chang C, Thomason ME, Dennis E, Gotlib IH. Default-mode and task-positive network activity in major depressive disorder: implications for adaptive and maladaptive rumination. Biol Psychiatry 2011;70:327–33.
Goodman ZT, Bainter SA, Kornfeld S, Chang C, Nomi JS, Uddin LQ. Whole-brain functional dynamics track depressive symptom severity. Cereb Cortex 2021;31:4867–76.
Sridharan D, Levitin DJ, Menon V. A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci. 2008;105:12569–74.
de Lacy N, McCauley E, Kutz JN, Calhoun VD. Sex-related differences in intrinsic brain dynamism and their neurocognitive correlates. Neuroimage 2019;202:116116.
Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319.
Maney DL. Perils and pitfalls of reporting sex differences. Philos Trans R Soc B Biol Sci. 2016;371:20150119.
Matsui T, Pham TQ, Jimura K, Chikazoe J. On co-activation pattern analysis and non-stationarity of resting brain activity. Neuroimage 2022;249:118904.
Allen EA, Damaraju E, Plis SM, Erhardt EB, Eichele T, Calhoun VD. Tracking whole-brain connectivity dynamics in the resting state. Cereb Cortex 2014;24:663–76.
Vidaurre D, Smith SM, Woolrich MW. Brain network dynamics are hierarchically organized in time. Proc Natl Acad Sci. 2017;114:12827–32.
Karahanoğlu FI, Van De Ville D. Transient brain activity disentangles fMRI resting-state dynamics in terms of spatially and temporally overlapping networks. Nat Commun. 2015;6:7751.
Kaiser RH, Chase HW, Phillips ML, Deckersbach T, Parsey RV, Fava M, et al. Dynamic Resting-State Network Biomarkers of Antidepressant Treatment Response. Biol Psychiatry 2022;92:533–42.
Funding
This project was supported by the National Natural Science Foundation of China (82071532 to SY). Dr. Dong was funded by the Scientific Research Launch Project for new employees of the Second Xiangya Hospital of Central South University. Dr. Ironside has additional funding from the National Institute of Mental Health (NIMH; R01MH132565). Dr. Belleau is supported by funding from the National Institute of Mental Health (K23MH122668) and the Klingenstein Third Generation Foundation. The content is solely the responsibility of the authors. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
SY, ELB, DAP, and XW conceptualized the study; SY, XW, DD, XZ, CL, XS, GX, and CC collected the data; DD, ELB, TAWB, DAP, and MI analyzed the data and interpreted the data. DD drafted the manuscript with critical revisions from ELB, DAP, TAWB, and MI. All authors approved the final manuscript and are accounted for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Competing interests
Over the past three years, Dr. Pizzagalli has received consulting fees from Albright Stonebridge Group, Boehringer Ingelheim, Compass Pathways, Engrail Therapeutics, Neumora Therapeutics (formerly BlackThorn Therapeutics), Neurocrine Biosciences, Neuroscience Software, Otsuka, Sunovion, and Takeda; he has received honoraria from the Psychonomic Society and American Psychological Association (for editorial work) and from Alkermes; he has received research funding from the Brain and Behavior Research Foundation, Dana Foundation, Millennium Pharmaceuticals, and Wellcome Leap; he has received stock options from Compass Pathways, Engrail Therapeutics, Neumora Therapeutics, and Neuroscience Software. There are no conflicts of interest with the work conducted in this study. No funding from these entities was used to support the current work, and all views expressed are solely those of the authors. The other authors report no financial relationships with commercial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, D., Pizzagalli, D.A., Bolton, T.A.W. et al. Sex-specific resting state brain network dynamics in patients with major depressive disorder. Neuropsychopharmacol. 49, 806–813 (2024). https://doi.org/10.1038/s41386-024-01799-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-024-01799-1