Abstract
Identifying genetic contributors to cognitive impairments in psychosis-spectrum disorders can advance understanding of disease pathophysiology. Although CNS medications are known to affect cognitive performance, they are often not accounted for in genetic association studies. In this study, we performed a genome-wide association study (GWAS) of global cognitive performance, measured as composite z-scores from the Brief Assessment of Cognition in Schizophrenia (BACS), in persons with psychotic disorders and controls (N = 817; 682 cases and 135 controls) from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. Analyses accounting for anticholinergic exposures from both psychiatric and non-psychiatric medications revealed five significantly associated variants located at the chromosome 3p21.1 locus, with the top SNP rs1076425 in the inter-alpha-trypsin inhibitor heavy chain 1 (ITIH1) gene (P = 3.25×E−9). The inclusion of anticholinergic burden improved association models (P < 0.001) and the number of significant SNPs identified. The effect sizes and direction of effect of the top variants remained consistent when investigating findings within individuals receiving specific antipsychotic drugs and after accounting for antipsychotic dose. These associations were replicated in a separate study sample of untreated first-episode psychosis. The chromosome 3p21.1 locus was previously reported to have association with the risk for psychotic disorders and cognitive performance in healthy individuals. Our findings suggest that this region may be a psychosis risk locus that is associated with cognitive mechanisms. Our data highlight the general point that the inclusion of medication exposure information may improve the detection of gene-cognition associations in psychiatric genetic research.
Similar content being viewed by others
Introduction
Cognitive deficit is an enduring core feature across psychotic disorders [1, 2]. Persons with schizophrenia exhibit impairments in numerous cognitive domains, including memory, learning, attention, processing speed, and executive function [3,4,5,6,7]. While the severity of cognitive dysfunction varies across persons with psychosis, on average, generalized deficits are one to two standard deviations below the performance of healthy comparison groups [2, 6, 8]. These deficits are a major cause of functional disability [9] and elucidating their underpinning mechanisms is important for understanding disease pathophysiology, and for developing treatment strategies to reduce functional deficits and related illness burden.
Cognitive impairments in psychotic disorders are typically present before the onset or diagnosis of illness and remain relatively stable over time [6, 10,11,12]. Given the stability, reliability, and heritability of this clinically important feature of psychosis [2, 10, 13], this quantitative phenotype is a promising target for genetic association studies. Overlap in genetic associations with risk for bipolar disorder, schizophrenia, and intellectual ability have been recently reported [14,15,16,17,–18], and a recent meta-analysis identified that across multiple studies, genetic risk for psychosis is associated with cognitive traits and relevant brain function measures in healthy persons [19, 20].
Identifying genetic relationships with cognitive phenotypes in patients with psychotic disorders has been challenging [21, 22]. One confounding factor may be medications with anticholinergic and/or antidopaminergic activity, which may impact cognition [23,24,25,26,27,28,29,30,31,–32], induce phenotypic variability in patient populations, and thereby weaken genotype/phenotype associations. While studies of the influence of antipsychotic drugs on cognition in persons with psychosis reported mixed findings [23,24,25,–26, 31, 33], studies of anticholinergic medications have consistently demonstrated adverse effects on cognitive function in several patient populations, including psychosis-spectrum disorders [24, 27,28,29,30]. Persons with psychotic disorders are often treated with psychotropic medications, which possess antidopaminergic and/or anticholinergic activities [34] as well as non-psychotropic medications for medical comorbidities, which may also have anticholinergic properties [35, 36]. Thus, there is considerable potential impact of CNS-active drug treatment to impact genotype–phenotype associations in these patient populations.
The Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) was established to characterize similarities and differences in cognitive, neurophysiological, and brain imaging phenotypes across the psychosis spectrum with the collection of extensive neurobiological phenotype, clinical, and genetic information [37]. We previously reported a continuum of neurocognitive impairments in individuals with clinically stable psychotic illness, which were gradually worse from bipolar disorder to schizoaffective disorder to schizophrenia [2], consistent with other reports [1, 2, 38,39,40,41]. Familiality estimates, however, did not differ across diagnoses, suggesting a similar degree of genetic contribution to cognitive function across the psychosis spectrum [2].
While previous associations of antipsychotic dose and cognition and functional brain connectivity were not robust [2, 42], we observed a significant negative impact of anticholinergic burden on cognition within B-SNIP participants [43]. These findings suggest that cumulative anticholinergic burden may be robust enough to be a potential confounder in gene association studies of cognitive impairments. In the present study, we conducted what is to our knowledge the first GWAS of global cognitive performance in individuals with psychotic disorders and controls accounting for anticholinergic exposures from both psychiatric and non-psychiatric medications. Participants included individuals from the B-SNIP study [37] with replication in a separate untreated first episode psychosis study sample [44]. We hypothesized that accounting for potential medication confounders would facilitate the identification of novel genetic contributors to cognition in persons with psychosis.
Materials and methods
Participants
We examined eight hundred and seventeen participants (schizophrenia N = 287, schizoaffective disorder N = 173, psychotic bipolar disorder N = 222, and healthy controls N = 135) from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. Details of the overall B-SNIP study design and clinical measurements have been previously reported [37]. Inclusion criteria included: (1) age 15–65; (2) Wide Range Achievement Test (WRAT) Reading Score ≥ 65; (3) English proficiency; (4) no history of seizures or head injury with loss of consciousness >10 min; (5) no diagnosis of substance abuse during the past 30 days or substance dependence during the previous 6 months; (6) negative urine toxicology on the day of testing; (7) no history of neurologic or systemic medical disorder; and (8) detailed medication information to quantify anticholinergic burden for both psychiatric and non-psychiatric medications. Additional inclusion criteria for healthy controls included no personal or immediate family history of a psychotic disorder or recurrent depression. All cases were clinically stable without major changes in psychopharmacological therapy for at least 4 weeks. Replication analyses were performed in N = 100 participants with untreated first episode psychosis defined as having <18 cumulative weeks of lifetime antipsychotic exposure. Seventy-nine percent were antipsychotic naïve, and those with prior treatment (21%) were at least 4 days free of any prior antipsychotic medications at the time of enrollment and initial assessments [44]. Except for first episode and prior treatment status, participants from each study sample met similar inclusion/exclusion criteria. Demographic and clinical characteristics of the study participants are summarized in Table 1 and Supplementary Tables S1 and S2. Institutional review boards approved the study at each recruitment site and written informed consent for phenotyping, and subsequent genetic studies was obtained before study participation.
Neuropsychological performance
Neuropsychological performance was assessed in the B-SNIP study sample using the Brief Assessment of Cognition in Schizophrenia (BACS) [45, 46]. The BACS consists of six subtests to assess four cognitive domains (verbal memory, working memory, processing speed, and reasoning). BACS composite and subtest z-scores were computed for each participant based on age-stratified and sex-stratified normative data [46]. The BACS composite z-score was evaluated as the primary outcome variable. The first episode study sample was administered a comparable neuropsychological battery assessing similar cognitive domains including verbal memory, visual memory, motor skills, executive function, attention, spatial abilities. A composite z-score was similarly constructed as the mean of domain scores and anchored to the demographically matched sample of healthy volunteers [10].
Medication assessments
A list of prescription and non-prescription medications, doses and administration frequency were collected from each case and control participant by conducting a detailed medication history interview. All individuals with a psychotic disorder had no major changes in medication regimen for at least 4 weeks, and we included the subjects who had detailed dosing information available in the analysis. Estimated anticholinergic potency of each scheduled medication was assigned using an updated version of the Anticholinergic Drug Scale (ADS) as previously described [43], which has been validated against serum anticholinergic activity (SAA) and widely used in previous research [36, 47]. Total ADS scores reflected the sum of all scheduled medications (both psychiatric and non-psychiatric) weighted by anticholinergic properties. Previous investigation of the relationships between ADS and BACS performance in B-SNIP participants identified a threshold effect of anticholinergic burden (ADS score ≥ 4 defined as high burden) [43], which was consistent in the participants of the present analysis (Supplementary Fig. S1). Based on this relationship, continuous anticholinergic scores were dichotomized to “high” and “low” burden for analyses in genetic association models [43]. To estimate antipsychotic exposures, doses were converted to chlorpromazine equivalents (CPZeq) [48].
Genotyping and imputation
Genomic DNA was extracted from whole blood using standard protocols and genotyped in the B-SNIP sample with the Illumina Infinium PsychChip array at the Broad Institute, and in the first episode sample with the Affymetrix Genome-Wide Human SNP Array 6.0 (Affymetrix, Santa Clara, CA, USA) as described previously [44, 49]. Quality control (QC) procedures were conducted using PLINK v1.9 [50]. Genotypes having call rates >98% by SNP and >98% by sample, and minor allele frequency (MAF) ≥ 0.01 were included in analyses. We excluded genetic markers that were monomorphic, deviating from Hardy–Weinberg Equilibrium (P < 10E−6), or genotype-inferred sex differing from reported sex. PREST-plus [51] and KING [52] were used to check cryptic relatedness, and individuals showing a 3rd degree or closer kinship were excluded. Genetic markers that passed QC procedures were imputed to the 1000 Genomes project multiethnic reference panel [53] using HAPI-UR for pre-phasing [54] and IMPUTE2 for imputation [55]. Poorly imputed SNPs were filtered for missingness (<5% by marker and <2% by sample) and MAF (<0.05).
Genome-wide association analyses
PLINK v1.9 was used to examine genome-wide associations with neurocognitive performance. Given the population admixture in our study sample set, participants were stratified into two major ancestry groups (predominantly European ancestry N = 521, predominantly African ancestry N = 295). Race stratification was performed using multi-dimensional scaling plot based on 1000 Genomes Project populations, resulting in the two predominating ancestry groups (Supplementary Fig. S2) [56]. Principal component analysis (PCA) was then performed separately within each ancestry subset. The first 15 eigenvectors captured ~80% of variance in each group and were used as covariates to account for residual population structure specific to each population (Supplementary Fig. S3) [57]. Composite z-scores on neuropsychological measures accounting for age and sex were examined as quantitative trait phenotypes using a linear model that also included ADS group to control for variance due to anticholinergic burden. Controls and persons with psychosis were combined for genome-wide association analyses to include a broader range of phenotypic variance, and increase the possibility of detecting genetic associations with cognitive performance [56, 58]. The GWAS results for each population were then combined by cross-ancestry meta-analysis, where both fixed-effects model and random-effect model were utilized [57]. The standard genome-wide significance threshold (P < 5 × E−8) was used to define significant SNP associations with the BACS. Quantile–quantile plot (Q–Q plot) for the meta-analysis was created to test for possible inflation in findings (Supplementary Fig. S4), and the genomic inflation factor (λ) of each GWAS was 1, suggesting that the population structures were properly adjusted. GWAS of the full cohort combined was additionally conducted using the first two PCA eigenvectors as covariates for comparison, which is presented in Supplementary Fig. S5.
Linear regression analysis was performed to further characterize the top associations, while controlling for the first two eigenvectors from the joint analysis and ADS group within persons with a psychotic disorder and in each ancestry group. For the top SNP, the change in R2 between regression models with and without ADS group was evaluated for significance using an F-test to test the improvement in the model by adding anticholinergic information. The analysis was repeated using the raw ADS score as a linear variable instead of the dichotomized ADS group for comparison and to confirm effect on the genetic model. Highly associated SNPs were also examined in relation to BACS subtests to quantify effect sizes using a linear regression model controlling for the first two eigenvectors and ADS group. Furthermore, all analyses were repeated additionally adjusting for DSM-IV diagnosis or within B-SNIP neurophysiology-defined Biotypes [58] to examine the potential effect of diagnosis or Biotypes. Top SNPs identified in the B-SNIP study sample GWAS were examined for replication and consistency of direction of effect and effect size in the first episode sample. Associations in the replication sample were also separately conducted within ancestry subsets, which were then combined using meta-analysis.
In additional analyses, we quantified and controlled for effects of symptom severity (Positive and Negative Syndrome Scale [PANSS total score]) and log transformed CPZeq as covariates in patients, and also conducted analyses of top genetic associations with BACS in subsets of participants receiving the most common monotherapy antipsychotic agents (aripiprazole N = 101, risperidone N = 95). We also examined effect sizes of significant results within psychosis subgroups defined by DSM-IV diagnosis and B-SNIP neurophysiology-defined Biotypes [59]. Statistical analyses were performed with SPSS version 23 (IBM Corp, Armonk, NY).
Functional analyses of top association findings and exploratory pathway analyses
Expression quantitative trait loci analyses of genome-wide significant SNPs were conducted to further examine the biological plausibility of top associations. Correlations of identified SNPs with gene expression were assessed using the United Kingdom Brain Expression Consortium (UKBEC, www.braineac.org) and the Genotype-Tissue Expression (GTEx) Portal (www.gtexportal.org/home).
Results
BACS composite score
GWAS of BACS composite score
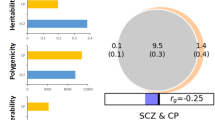
Analysis adjusting for anticholinergic medication burden revealed five genome-wide significant SNPs (top SNP, rs1076425; P = 3.25 × E−9). These SNPs are intronic variants of the inter-alpha-trypsin inhibitor heavy chain 1 gene (ITIH1) at chromosome 3p21.1 (Figs. 1 and 2a and Table 2). In addition, 49 of the top 82 associated variants P < 1 × 10−5 were located within several genes at the 3p21.1 region, including ITIH1, Scm like with four mbt domains 1 gene (SFMBT1), PHD finger protein 7 (PHF7), and inter-alpha-trypsin inhibitor heavy chain family member 4 gene (ITIH4) (Supplementary Table S3).
a Regional plot for rs1076425. The figure was created with LocusZoom (http://locuszoom.org/). b Composite BACS score by ITIH1 rs1076425 genotype in psychosis patients with 95% CI. SNP single-nucleotide polymorphism, Mb megabases, BACS brief assessment of cognition in schizophrenia, CI confidence interval.
Comparing BACS composite scores across genotype groups of the top finding, rs1076425, revealed that the G allele (minor allele) was associated with better cognitive performance. This relationship between rs1076425 genotype and BACS composite scores remained the same in an analysis restricted to the psychosis group (Fig. 2b). Posthoc analyses compared genetic associations in models with and without anticholinergic burden. These results revealed that four of five GWAS significant results identified by including anticholinergic burden would not have passed statistical thresholds, had this variable not been included in the primary models (Supplementary Fig. S6). R2 increased from 12.6 to 16.9% when anticholinergic burden was added to the regression model of the top SNP association, and this change in R2 was statistically significant (F(1, 801) = 40.907, P < 0.001) (Supplementary Table S4). Using raw ADS score instead of ADS group did not make a difference in the top SNP association (SNP effect size = 0.191 using ADS group vs. 0.180 using ADS raw score) with regression model comparisons available in Supplementary Table S4).
Influence of symptom severity and antipsychotic medications
The association of the rs1076425 (top SNP) with BACS composite score in persons with a psychotic disorder remained significant (P = 0.002) in regression analysis after additionally controlling for current symptom severity (PANSS total score) and estimated antipsychotic dose (CPZeq). Significant associations were also observed with the other four GWAS significant SNPs in similar analyses. Antipsychotic dose neither did not significantly differ across rs1076425 genotype groups (P = 0.721), nor did antipsychotic exposure change the relationship between rs1076425 or other top SNPs and BACS composite scores. Additionally, when examining subsets of individuals receiving individual antipsychotic agents as monotherapy (aripiprazole or risperidone), the effect size (β) of the genotype on cognitive performance in each subgroup remained consistent (β = 0.167 for all individuals, 0.176 for the risperidone group, and 0.145 for the aripiprazole group, Table 3). Our analyses did not identify effects of antipsychotic drug class (e.g., first or second generation) or dose on the observed genetic association.
Genetic relationships across DSM diagnosis, Biotype, and ancestry subgroups
The association between the top SNP and BACS composite scores remained significant in each race group with similar effect sizes (Table 3). Analyses stratified by diagnosis revealed the associations were significant in schizophrenia, schizophrenia + schizoaffective disorder, and psychotic bipolar disorder groups, with the largest effect size in schizophrenia (Table 3). The effect of the top SNP was found to be significant only in the Biotype 1 group among the 3 B-SNIP defined Biotype groups (Table 3). All findings remained consistent after adjusting for diagnosis group (Supplementary Table S4).
BACS subtests
The effect sizes of top SNPs were comparable across subtests of the BACS, and all associations between the significant variants and each BACS subtest were statistically significant (Supplementary Table S5). The most robust association was observed with Verbal Fluency (β of the top SNP = 0.182, P < 0.001).
Replication of findings in the first episode study sample
In the first episode psychosis study sample, where participants were largely medication naïve and free of anticholinergic burden, all five GWAS significant SNPs were replicated with nominally significant associations with composite cognitive scores (Supplementary Table S6). The effect sizes of the significant SNPs in the first episode participants were greater than those in B-SNIP. For those SNPs, first episode individuals who were homozygous for the minor allele had better composite cognitive scores, consistent with the direction and magnitude of effect observed in the B-SNIP study sample.
Discussion
GWAS to date have identified a number of candidate genes and risk loci for psychotic disorders [60, 61]. Examining genetic associations with quantitative intermediate phenotypes related to psychotic illness, such as cognitive impairment, can be a complementary research strategy to advance understanding of psychotic illness and treatment development. Our GWAS of cognitive performance in clinically stable persons with psychotic disorders and healthy controls revealed associations at the chromosome 3p21.1 region, which is a gene rich locus previously identified in disease risk studies of schizophrenia and bipolar disorder [60,61,62,63,64,65,66,67,68,–69] as well as cognitive ability in healthy individuals [70]. The associations remained consistent in each diagnostic group and for each BACS subtest, and were of similar magnitude, suggesting no moderating effects of diagnosis or types of cognitive tests on the reported associations. We replicated our findings in a separate, first-episode psychosis study sample free of antipsychotic drugs at the time of assessment. Importantly, accounting for anticholinergic burden improved our ability to detect gene-cognition associations, yielding novel findings that bridge prior disease risk findings with prior cognitive associations in healthy persons, clarifying this as a psychosis risk locus related to pathophysiological mechanisms of cognitive impairment. In addition to the scientific advance in establishing genetic associations with cognitive impairment, these findings highlight the importance of considering drug utilization and dosing information in gene-phenotype studies of neuropsychiatric disorders.
We identified significant associations with global cognitive performance in variants at the chromosome 3p21.1 locus. This locus was also identified in a previous GWAS and meta-analysis of cognitive processing that reported 3p21.1 relationships in a generally healthy population of European ancestry [70]. Of the five GWAS significant SNPs in our study, four were observed to have significant associations with general cognitive ability in that study: rs1076425 (z-score = −6.081, P = 1.19 × E−9 in Davies et al.), rs2284350 (z-score = −6.441, P = 1.19 × E−10 in Davies et al.), rs2300149 (z-score = 6.581, P = 4.67 × E−11 in Davies et al.), and rs2239550 (z-score = 6.601, P = 4.09 × E−11 in Davies et al.) [70]. With respect to disease risk, the Psychiatric Genomics Consortium (PGC) has identified chr3p21.1 as a risk locus for bipolar disorder [60], schizophrenia [61, 67], and three other major psychiatric disorders (autism spectrum disorder, attention deficit-hyperactivity disorder, and major depressive disorder) [71]. These findings were also confirmed in other GWAS and meta-analyses [62,63,64,65,–66, 68, 69].
The top SNP identified herein was rs1076425 located in the inter-alpha-trypsin inhibitor heavy chain 1 gene (ITIH1), where the minor G allele was associated with better cognitive performance. The ITIH1 gene encodes a member of inter-alpha-trypsin inhibitors that is extensively expressed in the liver (www.gtexportal.org) but also in the brain (www.braineac.org). The inter-alpha inhibitor family appears to have anti-proteolytic and anti-inflammatory activities;[72] however, little information exists on the specific biological function of ITIH1. Expression quantitative trait loci (eQTL) analyses showed that all five top SNPs in our study are significantly correlated with expression of the guanine nucleotide-binding protein-like 3 gene (GNL3) and inter-alpha-trypsin inhibitor heavy chain family member 4 gene (ITIH4) in multiple regions of the human brain (www.gtexportal.org/www.braineac.org).
Nucleostemin is encoded by GNL3 and known to play an important role in control of cell cycle progression in central nervous system (CNS) stem cells. It has been shown that both depletion and overexpression of nucleostemin decreases stem cell proliferation in CNS [73]. A previous GWAS reported a suggestive association of GNL3 with bipolar disorder [63], and one of the SNPs found to be jointly influencing schizophrenia risk and cognitive ability of healthy persons in a previous study was also identified as an eQTL for GNL3 [20]. Moreover, a recent study revealed that GNL3 overexpression resulted in a significant reduction of dendritic spines in rat cortical neurons [19]. Evidence of nucleostemin dysregulation causing abnormal CNS stem cell proliferation [73] and reduced density of rat dendritic spines [19], along with GWAS findings, suggests that GNL3 may be a potential candidate molecule for further investigation in relation to cognitive deficits as well as increasing psychosis risk. ITIH4 encodes inter-alpha-trypsin inhibitor heavy chain 4 that appears to be involved in varied inflammatory responses [74]. Although its biological function is not fully understood, this gene has been associated with schizophrenia disease risk [61, 67, 69], as well as intracranial volume in persons with schizophrenia [75].
The present findings derived from our GWAS of cognition combining a case and control sample with replication in untreated first episode patients, provides further clarity that this locus may represent a region of the genome related to psychosis risk associated with cognitive mechanisms or cognitive aspects of disease. Despite these findings, it is difficult to pinpoint whether there is a specific gene that unequivocally accounts for the association findings due to the large area of strong linkage disequilibrium (LD) in this region (Fig. 2a) [76, 77]. Further efforts, including mapping and physiological pathway studies, will be required to identify whether there is one causal gene or a collective impact of multiple genes responsible for associations with this locus.
Prior analyses of associations in this region, as well as top findings from our study suggest links to both neurodevelopmental and possibly inflammatory mechanisms. An exploratory examination of our top genetic findings in the drug interactome database (https://www.dgidb.org/) identified pathway connections to known immune system modulating drugs (e.g., fostamatinib, ipilimumab, everolimus, etc.). The direct clinical relevance or application of these links is not clear. However, altered immune and inflammation pathways have gained recent attention for links to neuropathology [78], as well as possible interventions including other anti-inflammatory drugs or biologics such as tocilizumab and fingolimod [79].
Accumulating evidence has quantified the adverse cognitive effects of anticholinergic medications [24, 27, 28, 43]. Despite this, drug exposures are not typically accounted for in genetic association studies of cognition in psychotic disorders. Psychosis-spectrum disorders are often treated with numerous medications that have anticholinergic properties at varying doses, and with varying and established effects on cognition [24, 25, 34, 35]. The present findings demonstrate the importance of taking into account the influence of anticholinergic medications in association studies of this patient population. Given established alterations of learning and memory functions in psychotic disorders [3], and of cholinergic systems for these cognitive functions [80], it is noteworthy that genetic associations herein were nonspecific with regard to BACS subtests. This is consistent with observations that cognitive deficits in schizophrenia primarily represent a generalized deficit [7]. We observed a greater number of GWAS significant associations and significantly improved genetic association models when controlling for anticholinergic medication burden. The most likely explanation for these enhancements is that reducing background variance due to medication exposure improved our ability to detect true genetic associations. Replication of our GWAS findings in first episode psychosis patients without significant drug exposure further supports the notion that genetic associations may be more detectable when the influence of medications are partialed out.
This study has potential limitations that must be considered when interpreting the results. First, the cross-sectional study design only captures cognitive performance at a single point in time, precluding longitudinal characterization and true causal inference of genotype–phenotype associations. However, we note that cognitive deficits in psychotic disorders are a relatively stable trait [10, 81]. Second, the sample size was relatively modest for GWAS. The combined patient and control sample was used to increase sample size and phenotypic variance. However, we note that our top associations were replicated with consistent direction of effect and effect sizes in an independent untreated first episode psychosis study sample. While our sample is not large enough to unequivocally identify associations with smaller genetic effects or associations within individual groups sorted by DSM diagnoses or B-SNIP Biotypes, the effect sizes of our primary findings were similar across race and diagnosis groups in posthoc stratified analyses (Table 3). Third, medication information used in the present study was obtained by conducting a medication history interview, which may not reflect actual medication adherence and lifetime anticholinergic load. Nevertheless, the collected information was further corroborated by patients’ family members and medical chart records when needed. Therefore, despite this limitation, we believe the anticholinergic burden information is reliable and given our findings and those of previous studies, valuable to be included in these types of analyses.
In conclusion, we identified significant associations between global cognitive ability and SNPs at the chromosome 3p21.1 locus in persons with psychotic disorders and healthy controls. This region has been previously reported in disease risk association studies, and cognitive impairments in the general population. These findings further support a mechanistic relationship between genes in this region and molecular pathology of disease related to cognitive dysfunction. These data also provide compelling evidence indicating that anticholinergic exposure information can impact the detection of genetic associations with cognitive phenotypes, highlighting the importance of accounting for medication effects in future genetic studies of neuropsychiatric disorders.
Funding and disclosure
This work was supported by funding from the National Institute of Mental Health (MH083888 to J.R.B., MH072767 to S.K.H., MH083126 to J.L.R., MH077945 to G.D.P., MH085485 to B.A.C., MH077851 to C.A.T., MH078113 to M.S.K., MH077852 to G.K.T., MH096957 to E.S.G., MH077862 to J.A.S.). J.L.R. has received investigator-initiated support from Naurex, Inc. R.L. has received honoraria, served as a consultant, or advisory board member for Janssen-Cilag, Otsuka Pharma and Lundbeck. R.S.E.K. is the owner of VeraSci, a for-profit business that receives revenues from over 100 companies, most of which are pharmaceutical companies. VeraSci holds the copyright for the BACS used in this study, and R.S.E.K receives royalties directly. He has also received consulting income from Akili in the past year. C.A.T. declares an ad hoc consulting relationship with Sunovion, Astellas and Merck and membership on a Merck DSMB; C.A.T. is on the Clinical Advisory Board at Kynexis and Karuna Therapeutics and holds stock in Karuna. M.S.K. has received support from Sunovion and is a consultant to Forum Pharmaceuticals. J.A.S. has received support from VeraSci. The other authors report nothing to disclose. The funding agencies had no role in the design and conduct of the study collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References
Hill SK, Reilly JL, Harris MSH, Rosen C, Marvin RW, Deleon O, et al. A comparison of neuropsychological dysfunction in first-episode psychosis patients with unipolar depression, bipolar disorder, and schizophrenia. Schizophr Res. 2009;113:167–75.
Hill SK, Reilly JL, Keefe RSE, Gold JM, Bishop JR, Gershon ES, et al. Neuropsychological impairments in schizophrenia and psychotic bipolar disorder: findings from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. Am J Psychiatry. 2013;170:1275–84.
Hill SK, Beers SR, Kmiec JA, Keshavan MS, Sweeney JA. Impairment of verbal memory and learning in antipsychotic-naïve patients with first-episode schizophrenia. Schizophr Res. 2004;68:127–36.
Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P, et al. Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry. 1994;51:124–31.
Aas M, Dazzan P, Mondelli V, Melle I, Murray RM, Pariante CM. A systematic review of cognitive function in first-episode psychosis, including a discussion on childhood trauma, stress, and inflammation. Front Psychiatry. 2014;4:182.
Bilder RM, Goldman RS, Robinson D, Reiter G, Bell L, Bates JA, et al. Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am J Psychiatry. 2000;157:549–59.
Reilly JL, Sweeney JA. Generalized and specific neurocognitive deficits in psychotic disorders: utility for evaluating pharmacological treatment effects and as intermediate phenotypes for gene discovery. Schizophr Bull. 2014;40:516–22.
Keefe RSE, Fenton WS. How should DSM-V criteria for schizophrenia include cognitive impairment? Schizophr Bull. 2007;33:912–20.
Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30.
Hill SK, Schuepbach D, Herbener ES, Keshavan MS, Sweeney JA. Pretreatment and longitudinal studies of neuropsychological deficits in antipsychotic-naïve patients with schizophrenia. Schizophr Res. 2004;68:49–63.
Stefanopoulou E, Manoharan A, Landau S, Geddes JR, Goodwin G, Frangou S. Cognitive functioning in patients with affective disorders and schizophrenia: a meta-analysis. Int Rev Psychiatry. 2009;21:336–56.
Velthorst E, Meyer EC, Giuliano AJ, Addington J, Cadenhead KS, Cannon TD, et al. Neurocognitive profiles in the prodrome to psychosis in NAPLS-1. Schizophr Res. 2019;204:311–9.
Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160:636–45.
Smeland OB, Bahrami S, Frei O, Shadrin A, O’Connell K, Savage J, et al. Genome-wide analysis reveals extensive genetic overlap between schizophrenia, bipolar disorder, and intelligence. Mol Psychiatry. 2020;25:844–53.
Hubbard L, Tansey KE, Rai D, Jones P, Ripke S, Chambert KD, et al. Evidence of common genetic overlap between schizophrenia and cognition. Schizophr Bull. 2016;42:832–42.
Hagenaars SP, Harris SE, Davies G, Hill WD, Liewald DCM, Ritchie SJ, et al. Shared genetic aetiology between cognitive functions and physical and mental health in UK Biobank (N=112 151) and 24 GWAS consortia. Mol Psychiatry. 2016;21:1624–32.
Trampush JW, Yang MLZ, Yu J, Knowles E, Davies G, Liewald DC, et al. GWAS meta-analysis reveals novel loci and genetic correlates for general cognitive function: a report from the COGENT consortium. Mol Psychiatry. 2017;22:336–45.
Forstner AJ, Hecker J, Hofmann A, Maaser A, Reinbold CS, Mühleisen TW, et al. Identification of shared risk loci and pathways for bipolar disorder and schizophrenia. PLoS ONE. 2017;12:e0171595.
Yang Z, Zhou D, Li H, Cai X, Liu W, Wang L, et al. The genome-wide risk alleles for psychiatric disorders at 3p21.1 show convergent effects on mRNA expression, cognitive function, and mushroom dendritic spine. Mol Psychiatry. 2020;25:48–6.
Smeland OB, Frei O, Kauppi K, Hill WD, Li W, Wang Y, et al. Identification of genetic loci jointly influencing schizophrenia risk and the cognitive traits of verbal-numerical reasoning, reaction time, and general cognitive function. JAMA Psychiatry. 2017;74:1065–75.
Harvey PD, Sun N, Bigdeli TB, Fanous AH, Aslan M, Malhotra AK, et al. Genome-wide association study of cognitive performance in U.S. veterans with schizophrenia or bipolar disorder. Am J Med Genet B. 2020;183:181–94.
Mallet J, Le Strat Y, Dubertret C, Gorwood P. Polygenic risk scores shed light on the relationship between schizophrenia and cognitive functioning: review and meta-analysis. J Clin Med Res. 2020;9:341.
Nielsen RE, Levander S, Kjaersdam Telléus G, Jensen SOW, Østergaard Christensen T, Leucht S. Second-generation antipsychotic effect on cognition in patients with schizophrenia-a meta-analysis of randomized clinical trials. Acta Psychiatr Scand. 2015;131:185–96.
Sweeney JA, Keilp JG, Haas GL, Hill J, Weiden PJ. Relationships between medication treatments and neuropsychological test performance in schizophrenia. Psychiatry Res. 1991;37:297–308.
Reilly JL, Harris MSH, Keshavan MS, Sweeney JA. Adverse effects of risperidone on spatial working memory in first-episode schizophrenia. Arch Gen Psychiatry. 2006;63:1189–97.
Woodward ND, Purdon SE, Meltzer HY, Zald DH. A meta-analysis of neuropsychological change to clozapine, olanzapine, quetiapine, and risperidone in schizophrenia. Int J Neuropsychopharmacol. 2005;8:457–72.
Minzenberg MJ, Poole JH, Benton C, Vinogradov S. Association of anticholinergic load with impairment of complex attention and memory in schizophrenia. Am J Psychiatry. 2004;161:116–24.
Wojtalik JA, Eack SM, Pollock BG, Keshavan MS. Prefrontal gray matter morphology mediates the association between serum anticholinergicity and cognitive functioning in early course schizophrenia. Psychiatry Res. 2012;204:61–67.
Brébion G, Bressan RA, Amador X, Malaspina D, Gorman JM. Medications and verbal memory impairment in schizophrenia: the role of anticholinergic drugs. Psychol Med. 2004;34:369–74.
Strauss ME, Reynolds KS, Jayaram G, Tune LE. Effects of anticholinergic medication on memory in schizophrenia. Schizophr Res. 1990;3:127–9.
Keefe RSE, Sweeney JA, Gu H, Hamer RM, Perkins DO, McEvoy JP, et al. Effects of olanzapine, quetiapine, and risperidone on neurocognitive function in early psychosis: a randomized, double-blind 52-week comparison. Am J Psychiatry. 2007;164:1061–71.
Keedy SK, Reilly JL, Bishop JR, Weiden PJ, Sweeney JA. Impact of antipsychotic treatment on attention and motor learning systems in first-episode schizophrenia. Schizophr Bull. 2015;41:355–65.
Sweeney JA, Haas GL, Keilp JG, Long M. Evaluation of the stability of neuropsychological functioning after acute episodes of schizophrenia: one-year followup study. Psychiatry Res. 1991;38:63–76.
Chakos MH, Glick ID, Miller AL, Hamner MB, Miller DD, Patel JK, et al. Baseline use of concomitant psychotropic medications to treat schizophrenia in the CATIE trial. Psychiatr Serv. 2006;57:1094–101.
Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophr Bull. 1996;22:413–30.
Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The Anticholinergic Drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharm. 2006;46:1481–6.
Tamminga CA, Ivleva EI, Keshavan MS, Pearlson GD, Clementz BA, Witte B, et al. Clinical phenotypes of psychosis in the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). Am J Psychiatry. 2013;170:1263–74.
Hill SK, Harris MSH, Herbener ES, Pavuluri M, Sweeney JA. Neurocognitive allied phenotypes for schizophrenia and bipolar disorder. Schizophr Bull. 2008;34:743–59.
Lee J, Rizzo S, Altshuler L, Glahn DC, Miklowitz DJ, Sugar CA, et al. Deconstructing bipolar disorder and schizophrenia: a cross-diagnostic cluster analysis of cognitive phenotypes. J Affect Disord. 2016;209:71–79.
Harvey PD, Wingo AP, Burdick KE, Baldessarini RJ. Cognition and disability in bipolar disorder: lessons from schizophrenia research. Bipolar Disord. 2010;12:364–75.
Hill SK, Keshavan MS, Thase ME, Sweeney JA. Neuropsychological dysfunction in antipsychotic-naive first-episode unipolar psychotic depression. Am J Psychiatry. 2004;161:996–1003.
Herms EN, Bishop JR, Okuneye VT, Tamminga CA, Keshavan MS, Pearlson GD, et al. No connectivity alterations for striatum, default mode, or salience network in association with self-reported antipsychotic medication dose in a large chronic patient group. Schizophr Res. 2020. https://doi.org/10.1016/j.schres.2020.06.017.
Eum S, Hill SK, Rubin LH, Carnahan RM, Reilly JL, Ivleva EI, et al. Cognitive burden of anticholinergic medications in psychotic disorders. Schizophr Res. 2017;190:129–35.
Stevenson JM, Reilly JL, Harris MSH, Patel SR, Weiden PJ, Prasad KM, et al. Antipsychotic pharmacogenomics in first episode psychosis: a role for glutamate genes. Transl Psychiatry. 2016;6:e739.
Keefe RSE, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68:283–97.
Keefe RSE, Harvey PD, Goldberg TE, Gold JM, Walker TM, Kennel C, et al. Norms and standardization of the Brief Assessment of Cognition in Schizophrenia (BACS). Schizophr Res. 2008;102:108–15.
Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15:31.
Andreasen NC, Pressler M, Nopoulos P, Miller D, Ho B-C. Antipsychotic dose equivalents and dose-years: a standardized method for comparing exposure to different drugs. Biol Psychiatry. 2010;67:255–62.
Alliey-Rodriguez N, Grey TA, Shafee R, Asif H, Lutz O, Bolo NR, et al. NRXN1 is associated with enlargement of the temporal horns of the lateral ventricles in psychosis. Transl Psychiatry. 2019;9:230.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MAR, Bender D, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75.
Sun L, Dimitromanolakis A. PREST-plus identifies pedigree errors and cryptic relatedness in the GAW18 sample using genome-wide SNP data. BMC Proc. 2014;8:S23.
Manichaikul A, Mychaleckyj JC, Rich SS, Daly K, Sale M, Chen W-M. Robust relationship inference in genome-wide association studies. Bioinformatics 2010;26:2867–73.
1000 Genomes Project Consortium, Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, et al. An integrated map of genetic variation from 1092 human genomes. Nature 2012;491:56–5.
Williams AL, Patterson N, Glessner J, Hakonarson H, Reich D. Phasing of many thousands of genotyped samples. Am J Hum Genet. 2012;91:238–51.
Howie B, Fuchsberger C, Stephens M, Marchini J, Abecasis GR. Fast and accurate genotype imputation in genome-wide association studies through pre-phasing. Nat Genet. 2012;44:955–9.
Lencer R, Mills LJ, Alliey-Rodriguez N, Shafee R, Lee AM, Reilly JL, et al. Genome-wide association studies of smooth pursuit and antisaccade eye movements in psychotic disorders: findings from the B-SNIP study. Transl Psychiatry. 2017;7:e1249.
Peterson RE, Kuchenbaecker K, Walters RK, Chen C-Y, Popejoy AB, Periyasamy S, et al. Genome-wide association studies in ancestrally diverse populations: opportunities, methods, pitfalls, and recommendations. Cell 2019;179:589–603.
Gershon ES, Pearlson G, Keshavan MS, Tamminga C, Clementz B, Buckley PF, et al. Genetic analysis of deep phenotyping projects in common disorders. Schizophr Res. 2018;195:51–57.
Clementz BA, Sweeney JA, Hamm JP, Ivleva EI, Ethridge LE, Pearlson GD, et al. Identification of distinct psychosis biotypes using brain-based biomarkers. Am J Psychiatry. 2016;173:373–84.
Psychiatric GWAS Consortium Bipolar Disorder Working Group. Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4. Nat Genet. 2011;43:977–83.
Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014;511:421–7.
Charney AW, Ruderfer DM, Stahl EA, Moran JL, Chambert K, Belliveau RA, et al. Evidence for genetic heterogeneity between clinical subtypes of bipolar disorder. Transl Psychiatry. 2017;7:e993.
Scott LJ, Muglia P, Kong XQ, Guan W, Flickinger M, Upmanyu R, et al. Genome-wide association and meta-analysis of bipolar disorder in individuals of European ancestry. Proc Natl Acad Sci USA. 2009;106:7501–6.
Chen DT, Jiang X, Akula N, Shugart YY, Wendland JR, Steele CJM, et al. Genome-wide association study meta-analysis of European and Asian-ancestry samples identifies three novel loci associated with bipolar disorder. Mol Psychiatry. 2013;18:195–5.
Ripke S, O’Dushlaine C, Chambert K, Moran JL, Kähler AK, Akterin S, et al. Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat Genet. 2013;45:1150–9.
Li Z, Chen J, Yu H, He L, Xu Y, Zhang D, et al. Genome-wide association analysis identifies 30 new susceptibility loci for schizophrenia. Nat Genet. 2017;49:1576–83.
Schizophrenia Psychiatric Genome-Wide Association Study (GWAS) Consortium. Genome-wide association study identifies five new schizophrenia loci. Nat Genet. 2011;43:969–76.
Sleiman P, Wang D, Glessner J, Hadley D, Gur RE, Cohen N, et al. GWAS meta analysis identifies TSNARE1 as a novel Schizophrenia/Bipolar susceptibility locus. Sci Rep. 2013;3:3075.
Li Z, Xiang Y, Chen J, Li Q, Shen J, Liu Y, et al. Loci with genome-wide associations with schizophrenia in the Han Chinese population. Br J Psychiatry. 2015;207:490–4.
Davies G, Lam M, Harris SE, Trampush JW, Luciano M, Hill WD, et al. Study of 300,486 individuals identifies 148 independent genetic loci influencing general cognitive function. Nat Commun. 2018;9:2098.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
Kobayashi H. Endogenous anti-inflammatory substances, inter-alpha-inhibitor and bikunin. Biol Chem. 2006;387:1545–9.
Tsai RYL, McKay RDG. A nucleolar mechanism controlling cell proliferation in stem cells and cancer cells. Genes Dev. 2002;16:2991–3003.
Song J, Patel M, Rosenzweig CN, Chan-Li Y, Sokoll LJ, Fung ET, et al. Quantification of fragments of human serum inter-alpha-trypsin inhibitor heavy chain 4 by a surface-enhanced laser desorption/ionization-based immunoassay. Clin Chem. 2006;52:1045–53.
Smeland OB, Wang Y, Frei O, Li W, Hibar DP, Franke B, et al. Genetic overlap between schizophrenia and volumes of Hippocampus, putamen, and intracranial volume indicates shared molecular genetic mechanisms. Schizophr Bull. 2017. https://doi.org/10.1093/schbul/sbx148.
Vassos E, Steinberg S, Cichon S, Breen G, Sigurdsson E, Andreassen OA, et al. Replication study and meta-analysis in European samples supports association of the 3p21.1 locus with bipolar disorder. Biol Psychiatry. 2012;72:645–50.
Kondo K, Ikeda M, Kajio Y, Saito T, Iwayama Y, Aleksic B, et al. Genetic variants on 3q21 and in the Sp8 transcription factor gene (SP8) as susceptibility loci for psychotic disorders: a genetic association study. PLoS ONE. 2013;8:e70964.
Lizano P, Lutz O, Xu Y, Rubin LH, Paskowitz L, Lee AM, et al. Multivariate relationships between peripheral inflammatory marker subtypes and cognitive and brain structural measures in psychosis. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-00914-0.
Jeppesen R, Christensen RHB, Pedersen EMJ, Nordentoft M, Hjorthøj C, Köhler-Forsberg O, et al. Efficacy and safety of anti-inflammatory agents in treatment of psychotic disorders—a comprehensive systematic review and meta-analysis. Brain Behav Immun. 2020;90:364–80.
Haam J, Yakel JL. Cholinergic modulation of the hippocampal region and memory function. J Neurochem. 2017;142:111–21.
Pavuluri MN, West A, Hill SK, Jindal K, Sweeney JA. Neurocognitive function in pediatric bipolar disorder: 3-year follow-up shows cognitive development lagging behind healthy youths. J Am Acad Child Adolesc Psychiatry. 2009;48:299–7.
Acknowledgements
We thank the patients and their families who participated in this study, and Gunvant Thaker, MD, for his scientific contributions to the B-SNIP consortium. We also thank Tom Kono and the University of Minnesota Supercomputing Institute for assistance with DNA array imputation for the replication sample.
Author information
Authors and Affiliations
Contributions
All authors had substantial contributions to either the conceptual design (J.R.B., S.E.), acquisition (J.L.R., S.K.K., E.I., G.D.P., B.A.C., C.A.T., M.S.K., E.S.G., J.A.S., and J.R.B.), analysis (S.E., S.K.H., N.A.R., J.M.S., L.J.M., A.M.L., J.L.R., J.A.S., and J.R.B.), or interpretation of data (all authors) for the work. All authors were involved with drafting the work and/or revising it critically for important intellectual content and approve of the final version to be published. S.E. and J.R.B. agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Eum, S., Hill, S.K., Alliey-Rodriguez, N. et al. Genome-wide association study accounting for anticholinergic burden to examine cognitive dysfunction in psychotic disorders. Neuropsychopharmacol. 46, 1802–1810 (2021). https://doi.org/10.1038/s41386-021-01057-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-021-01057-8
This article is cited by
-
The genetic relationships between brain structure and schizophrenia
Nature Communications (2023)
-
Cross-diagnostic determinants of cognitive functioning: the muscarinic cholinergic receptor as a model system
Translational Psychiatry (2023)
-
Distinct sex-specific DNA methylation differences in Alzheimer’s disease
Alzheimer's Research & Therapy (2022)