Abstract
Almost three decades have passed since the first posttraumatic stress disorder (PTSD) neuroimaging study was published. Since then, the field of clinical neuroscience has made advancements in understanding the neural correlates of PTSD to create more efficacious treatment strategies. While gold-standard psychotherapy options are available, many patients do not respond to them, prematurely drop out, or never initiate treatment. Therefore, elucidating the neurobiological mechanisms that define the disorder can help guide clinician decision-making and develop individualized mechanisms-based treatment options. To this end, this narrative review highlights progress made in the last decade in adult and youth samples on three outstanding questions in PTSD research: (1) Which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure) alterations? (2) Which neural alterations can predict treatment outcomes and define clinical improvement? and (3) Can neuroimaging measures be used to define brain-based biotypes of PTSD? While the studies highlighted in this review have made progress in answering the three questions, the field still has much to do before implementing these findings into clinical practice. Overall, to better answer these questions, we suggest that future neuroimaging studies of PTSD should (A) utilize prospective longitudinal designs, collecting brain measures before experiencing trauma and at multiple follow-up time points post-trauma, taking advantage of multi-site collaborations/consortiums; (B) collect two scans to explore changes in brain alterations from pre-to-post treatment and compare changes in neural activation between treatment groups, including longitudinal follow up assessments; and (C) replicate brain-based biotypes of PTSD. By synthesizing recent findings, this narrative review will pave the way for personalized treatment approaches grounded in neurobiological evidence.
Similar content being viewed by others
Introduction
In 2013, the American Psychiatric Association revised the posttraumatic stress disorder (PTSD) criteria in the 5th edition of its “Diagnostic Statistical Manual of Mental Disorders” (DSM-5). While the DSM-IV classified PTSD under “Anxiety Disorders,” the DSM-5 has repositioned it within a newly established category of “Trauma-and Stressor-Related Disorders.” According to the DSM-5, traumatic events are defined as exposure to actual or threatened death, serious injury, or a threat to the physical integrity of oneself or others, either directly (witnessing trauma) or indirectly (learning that trauma happened to a close relative or friend) [1]. In addition to trauma exposure (i.e., criterion A), four symptom clusters that characterize the disorder are persistent re-experiencing the trauma (i.e., criterion B), avoiding people, places, or thoughts related to the trauma (i.e., criterion C), negative thoughts and feelings that began or worsened after the trauma (i.e., criterion D); and trauma-related increased in arousal and reactivity (i.e., criterion E). Symptoms must last at least one month, not be caused by drugs or other illnesses, and cause significant functional impairment. The DSM-5 introduced a developmental subtype of PTSD specifically for children aged six years or younger, aligning closely with adult diagnostic criteria. However, it adapts criterion A for this age group, allowing for indirect exposure to trauma, such as through witnessing an event or learning about a traumatic event affecting a parent or caregiver [1].
Epidemiology and prognosis
Worldwide, up to 70% of the adult population will experience at least one traumatic event (as defined by criterion A) in their lifetime [2], and the prevalence of PTSD ranges from 2 to 9% [3]. Indeed, four post-traumatic symptom trajectories have been highlighted in literature: resiliency, recovery, chronic, and delayed onset, the most common being the resiliency trajectory [4, 5]. Similarly, childhood trauma exposure is common, with up to two-thirds of youth reported having experienced a traumatic event and almost 5% of trauma-exposed youth meeting the criteria for PTSD [6,7,8]. It is important to note that females are more prone to developing PTSD than males [9, 10]. This disparity is theorized to be attributed to trauma one is exposed to, with females experiencing more interpersonal violence than males [11]. However, even when controlling for trauma type, females still exhibit greater PTSD prevalence [11]. This suggests that biological factors may contribute to this disparity. Given this, more studies are introducing sex as a biological variable to explore this disparity further. For in-depth reviews, see [12, 13].
PTSD is a debilitating disorder in many aspects across the lifespan. A PTSD diagnosis contributes to billions in annual productivity loss [14] and increased medical problems [15] and is associated with a variety of co-occurring disorders, including substance use disorders [16], depression, and anxiety [17]. For individuals diagnosed with PTSD, many treatment options are available. The most empirically supported options are trauma-focused interventions [18]. Of psychotherapy options available, up to half of the patients who complete treatment will show clinically meaningful improvement [19,20,21], and many patients prematurely drop out of treatment before receiving an adequate dose [22]. Furthermore, many patients fail to seek treatment altogether, especially in marginalized groups [23]. Given the considerable overlap between PTSD, depression, and anxiety, and because research still has not identified pharmaceutical targets specific for PTSD, sertraline and paroxetine are FDA-approved pharmacological options for PTSD, both with limited efficacy [24]. Research on using psychedelics to treat PTSD has skyrocketed and looks promising, though more research is needed to determine efficacy and validate safe implementation procedures [25, 26]. Psychotherapeutic treatments have shown a greater benefit than pharmacological intervention alone [27]. Determining the superiority of combining psychotherapy with pharmacological treatment needs further exploration [28]. To improve the efficacy of current treatment options and to design novel, more efficacious treatment options, we must understand the neural alterations that contribute to the development of PTSD, improve with treatment, and potentially define biotypes of the disorder.
Current narrative review
Given the influx of neuroimaging data published since the first neuroimaging paper using a PTSD sample in 1995 [29], an extensive library of reviews and meta-analyses has examined this literature [30,31,32,33,34,35,36,37,38,39,40]. Our narrative review builds upon this previous literature by exploring progress made in the past decade on three major questions in the field: (1) Which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure)? (2) Which neural alterations can predict treatment outcomes and define clinical improvement? and (3) Can neuroimaging measures be used to define brain-based biotypes of PTSD? This review will examine structural and functional magnetic resonance imaging (MRI) literature using univariate, bivariate, and network-based approaches in adult and youth PTSD populations. Following a brief overview of neural alterations in PTSD, we will address each question above by synthesizing current findings, identifying gaps, and discussing limitations. We included articles published in peer-reviewed journals and were found using in-house expertise and searches of databases including PubMed. We will conclude by highlighting the review’s limitations and suggest future directions. Tables 1–2 provide an overview of neuroimaging findings for questions 1 and 2 (respectively), and Figs. 1–2 illustrate these findings. We will begin by describing different neuroimaging techniques.
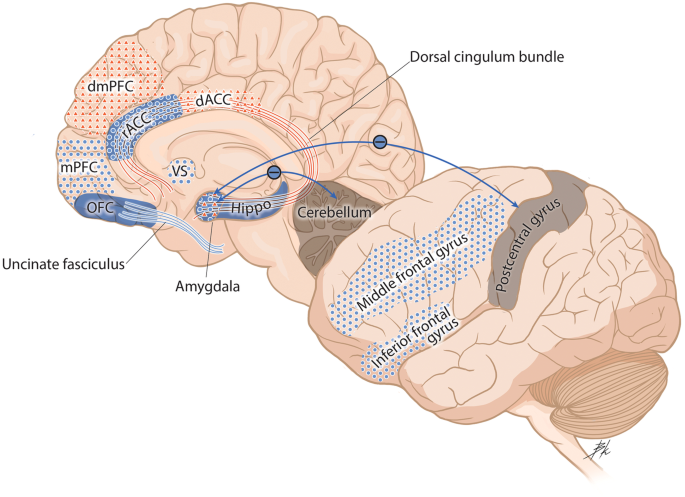
Blue dots represent decreased activation. Red triangles represent increased activation. Solid blue represents decreased volume. Solid blue lines represent decreased structural integrity. Red lines represented increased structural integrity. Functional connectivity findings are depicted with arrows, with blue lines (–) that represent decreased functional connectivity and red lines (+) that represent increased functional connectivity. dACC dorsal anterior cingulate cortex, dmPFC dorsomedial prefrontal cortex, Hippo hippocampus, mPFC medial prefrontal cortex, OFC orbitofrontal cortex, rACC rostral anterior cingulate cortex, VS ventral striatum.
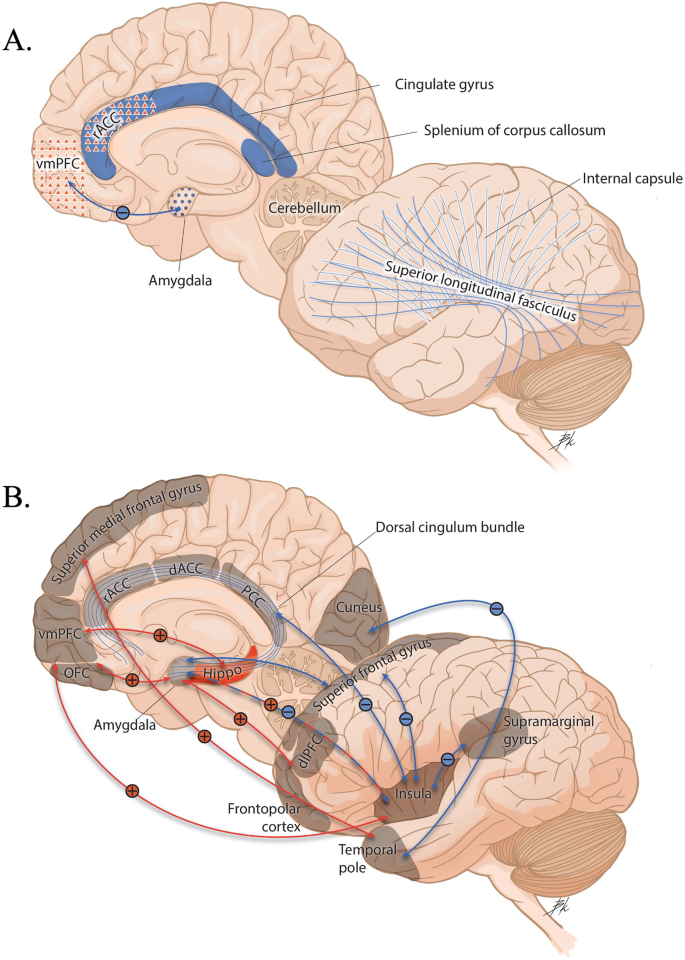
A Brain measures at baseline that predict a positive treatment response. B Brain measures associated with a positive response to treatment. Blue dots represent decreased activation. Red triangles represent increased activation. Solid blue represents decreased volume. Solid red represents greater volume. Solid blue lines represent decreased structural integrity. Functional connectivity findings are depicted with arrows, with blue lines (–) equating to decreased functional connectivity and red lines (+) equating to greater functional connectivity. dACC dorsal anterior cingulate cortex, dlPFC dorsolateral prefrontal cortex, Hippo hippocampus, OFC orbitofrontal cortex, PCC posterior cingulate cortex, rACC rostral anterior cingulate cortex, vmPFC ventromedial prefrontal cortex.
Neuroimaging techniques
Structural techniques
Structural MRI of PTSD populations typically determines alterations in the morphometry of brain regions in patients versus controls (trauma-exposed non-PTSD [TENC] or healthy controls [HC]). Morphometric measures include subcortical and cortical gray matter volumes, thickness, and white matter microstructure. There are two analysis pipelines one can follow: (1) surface-based, which identifies borders between pial and white matter surfaces, and (2) voxel-based, which labels each voxel in cortical and subcortical tissues and allows for calculating subcortical structures and total intracranial volume [41]. Thus, structural volume can be measured by contrasting volume inside the pial surface from the white surface and regions, not part of the cortex, or by measuring total cortical labeled voxels. Cortical thickness is measured by contrasting the distance between the pial and the white surface [41]. Generally, smaller volumes and lower cortical thickness are representative of poorer structural integrity. Diffusion tensor imaging is a structural tool used to measure the structural integrity of white matter tracts via the diffusivity of water molecules along the axial direction of white matter fibers. The pattern of diffusivity can be computed using scalar measures such as fractional anisotropy (FA), whereby lower FA values illustrate a reduced axonal packing density [42].
Functional techniques
Functional MRI (fMRI) can be used as an indirect proxy to measure brain activation with great spatial and limited temporal resolution. Researchers record activation during the presentation of different tasks designed to induce activation in regions responsible for given functions. There are many different approaches one can take to analyze fMRI data, which can be categorized into three general techniques. The simplest technique is univariate analyses, which examine the activation of single voxels in response to various tasks. As techniques developed with time, more researchers have also included bivariate analyses, which calculate the temporal association of two regions based on activation. This includes task-based and resting-state functional connectivity (FC), which measure spontaneous changes in brain activation during the completion or absence of a task, respectively. Finally, recent years have seen an increase in network-based approaches, which measure activation across many brain regions and networks. Network-based approaches in fMRI studies typically conceptualize the human brain as a network of interconnected functional components that operate in a coordinated dynamic fashion [43]. By employing such methods, researchers can overcome the limitations of traditional univariate and bivariate approaches by mitigating the bias of preselecting target regions a priori and allowing a more comprehensive investigation of large-scale brain organization (rather than isolated regions or simplistic circuits). In this narrative review, we will focus on the two primary tools for network-based analysis of neuroimaging data in PTSD: (1) independent component analysis (ICA), which isolates individual functional networks within the whole brain, and (2) graph theory methods, which examine properties of networks (e.g., nodes and edges of a graph) and characterize them based on their intercorrelations.
Neural alterations in PTSD
Adults
PTSD is the only DSM diagnosis with a known origin (i.e., experiencing trauma). Given the importance of traumatic memory in the development of the disorder, early neuroimaging studies sought to discover alterations in structure and function of brain regions implicated in fear learning and memory (e.g., amygdala and hippocampus) in patients with PTSD compared to controls. These discoveries have created “classical” neurocircuitry models of PTSD that emphasize an inability of cortical regions to successfully regulate subcortical regions important in initiating a fear response [33]. Research over the last decade has noted diminished structural integrity in areas associated with executive functions, including reduced cortical volumes in the anterior cingulate cortex (ACC) [44, 45] and frontal cortical regions [44, 46] in PTSD patients and in subcortical structures, including the amygdala and hippocampus (see [39, 47] for recent reviews). Furthermore, PTSD patients, compared to controls, have shown reduced white matter integrity in the uncinate fasciculus (UF) [48,49,50], corpus callosum, corticospinal tract, and enhanced white matter integrity in the inferior fronto-occipital fasciculus, and inferior temporal gyrus (for review see [51]), highlighting the structural disconnect between cortical and subcortical regions. Functional studies also support classical neurocircuitry models, with greater amygdala alongside reduced activation in brain regions associated with emotional regulation (e.g., ventromedial prefrontal cortex [vmPFC], inferior, superior, medial frontal gyrus [MFG], ACC, dorsolateral PFC [dlPFC], and dorsomedial PFC [dmPFC]) during emotion-related tasks [52,53,54,55,56,57,58,59,60,61,62], extinction recall [63], and fear generalization [64, 65]. Limitations of these classical neurocircuitry models of PTSD include the deficiency of the models to understand the biological bases of PTSD systems holistically rather than focusing on fear processes alone (see [35] for an in-depth discussion).
Network-level neural alterations in PTSD are present. Specifically, disruptions in connectivity structure or activation profiles within the salience network (SN), default mode network (DMN), and central executive network (CEN) may underlie univariate and bivariate impairments in PTSD patients. For example, hyperarousal and hyperreactivity symptoms were linked to increased activation of the amygdala and dACC, two critical nodes of the SN [33, 66, 67]. Further, intrusive symptoms, impaired fear extinction, and deficits in emotional regulation are associated with decreased activation of the hippocampus and vmPFC, two nodes of the DMN [31, 33, 68]. Decreased activation of nodes within the CEN, such as the IFG and MFG in PTSD, are present [32].
Numerous neuroimaging studies have employed ICA methodology to test alterations in large-scale networks in adults with PTSD (see reviews [69,70,71,72,73,74]). Overall, results are mixed and provide limited support for classical neurocircuitry models of PTSD. Within the DMN, most studies report decreased activation and connectivity at rest in PTSD patients [75,76,77], possibly associated with re-experiencing and dissociative symptoms [71, 78]. However, one study reported higher integration of the amygdala with the DMN in PTSD patients during a threat-processing task [79]. Research typically suggests increased activation and connectivity [83, 84] within the SN, potentially linked to hyperarousal and hypervigilance symptoms. In contrast, other findings indicate decreased SN connectivity in PTSD [48, 77]. The CEN seems to show reduced activation and connectivity among PTSD patients [32, 76].
In addition to alterations within each network, some recent evidence points to aberrant connectivity patterns between networks in PTSD. For example, Zhang and colleagues (2015) [77] reported decreased FC between the SN and DMN, possibly explaining previous contrasting findings regarding the connectivity of the SN in PTSD. As the SN is believed to facilitate the transition between the DMN and CEN in response to external cognitive demands [80], the reduced connectivity between the SN and DMN might suggest a compromised ability in PTSD to shift between a self-referential state and a cognitive control mode. In another study, PTSD patients showed increased excitatory influence of the executive central network (ECN, like the CEN) on the posterior DMN. Finally, Akiki et al. (2017) [71] suggested that PTSD is characterized by impaired SN, incapable of DMN-CEN modulation, and weakened top-down regulation of the SN by the CEN.
Several neuroimaging studies of PTSD used graph theory approaches in resting-state data to examine possible alternations in local and global connectivity patterns. One study found that PTSD patients exhibit a transformation from a random or regular network to a “small-world” network, compared to TENC [81]. The concept of “small-world” networks describes a network topology in which most nodes are not neighbors of one another, but still, nodes can be reached from every other by a small number of steps [82]. Furthermore, these patients show increased centrality in the DMN and SN [81] (i.e., amount of nodes with many paths passing through them). Indeed, more severe PTSD symptoms were linked to DMN alteration, including decreased FC strength [83], decreased functional integration, and increased segregation within the DMN [84]. Additionally, reduced within-network connectivity and decreased connectional density within a hippocampus-PFC network are associated with more severe re-experiencing symptoms in combat-exposed veterans [85]. These studies suggest a complex interplay of network alterations in PTSD.
Youth
In normative brain development, gray matter volume is shaped like an inverted U, whereby matter increases from birth to childhood, then around early adolescence, starts to decline until adulthood [86]. This development pattern is due to synaptic proliferation and pruning, which makes the child’s brain more efficient [87]. White matter generally increases throughout childhood and adolescence and then levels off [86]. This pattern represents increases in myelination over time to maximize neuronal transmission speed and adjust the timing and synchrony of neural spikes [88]. In total volume, including gray and white matter, young brains grow in size until late childhood/early adolescence, when they start to asymptote [89].
In pediatric samples, PTSD and TENC youth typically exhibit overall smaller amygdala [90,91,92] and hippocampal volumes [91, 93], including smaller CA2/3 hippocampal subfields [90, 94]. Studies report that youth with PTSD have smaller vmPFC volumes than TENC or HC youth [91, 95]. One study found no differences in the structure of the medial PFC (mPFC) between youth with PTSD and TENC [96], indicating that more work needs to be done to disentangle how maltreatment and PTSD relate to volume. Heyn and colleagues [97] (2022) explored sex differences in volume in female and male youth. Female youth with PTSD showed increased volume and surface area in the ventrolateral PFC and frontal pole regions. In contrast, male youth showed smaller volumes of these regions that predicted more severe symptoms one year later [97]. Additionally, youth with PTSD, compared to controls, had age- and sex-related differences in the UF, inferior longitudinal fasciculus, and cingulum bundle [98]. Finally, a review found that youth with PTSD had lower FA in the corpus callosum, including the anterior and posterior midbody, the isthmus, and the splenium [99], and increased PTSD symptoms have been related to lower FA in these regions [100].
Our comprehension of the typical developmental trajectories of brain function in youth remains limited. Univariate investigations have focused mostly on associations between childhood trauma and brain activation. In the past decade, a movement towards employing consistent brain atlases and pre-processing methods has emerged, particularly for comparing studies with limited sample sizes [101]. That said, the literature reviewed here will be specific to youth with PTSD and is, therefore, sparse.
In task-based fMRI, greater activation in the amygdala and dACC in response to emotional faces and threatening images have been found in youth with PTSD versus controls [102, 103]. Greater activation has been found in the ACC and frontal brain regions in maltreated youth than in HC during the presentation of negative stimuli [104]. Furthermore, there is an interesting pattern of decreased FC while viewing angry faces and increased FC while viewing happy faces, specifically between the dACC-dmPFC, amygdala-dmPFC, and amygdala-vlPFC [102]. Youth with PTSD showed increased PCC-vmPFC resting-state FC, which may indicate problems in self-referential tasks or memory consolidation [105]. In another resting-state study, youth with PTSD showed decreased PCC-hippocampus FC and increased PCC-insula and PCC-cerebellum FC [106].
Network-based analyses have had limited application in youth PTSD populations. This could be for numerous reasons, including low sample sizes and the novelty of computational imaging methods. The handful of studies that have used ICA and graph theory methods to identify alterations in youth with PTSD have identified a greater anticorrelation between DMN and task-positive network (TPN), indicative of difficulty switching between internal (DMN) and external (TPN) stimuli [105]. In one study of resting-state whole-brain connectivity in youth exposed to an earthquake, the PTSD group (compared to TENC) showed an increased clustering coefficient and a normalized characteristic path length and local efficiency, suggesting a shift toward regular networks [107]. Further, the authors found enhanced nodal centralities in the DMN and SN, which may be related to altered processing of negative emotions. They also found reduced centralities in the CEN, which may indicate worse goal-directed behaviors. In contrast, Xu and colleagues (2018) [108] reported a lower clustering coefficient among youth with PTSD compared to TENC. They further found increases in centralities in the attention and DMN and decreases in the salience and sensorimotor networks [109].
Question 1: which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure)?
An important goal in the PTSD field is to uncover whether the neural alterations in PTSD discussed above are predisposing risk factors that make an individual more susceptible to developing PTSD after experiencing trauma or acquired characteristics of the disorder. Uncovering these distinctions will enable the development of preventative interventions or the creation of more efficacious treatment options that target specific targets affected by the disorder. Many methodological approaches are used to disentangle predisposed from acquired neural alterations in PTSD [110]. The most methodologically sound techniques include prospective longitudinal studies, which collect neuroimaging data from participants either before trauma exposure or in the early aftermath of trauma and follow these participants at various time points post-trauma. Examples include the Neurobehavioral Moderators of Posttraumatic Disease Trajectories (NMPTDT) [111] and the Advancing Understanding of Recovery After Trauma (AURORA) studies [112]. While prospective longitudinal study designs are optimal for answering this question, they are hard to execute as they are often time-consuming, expensive, and have inherently poor participant attrition rates (see [111]). Further, though it is the goal to recruit participants before or in the early aftermath of trauma, participants may endorse childhood trauma experienced years before study participation, confounding the data collected.
Twin-pair designs have also been used to answer this question. Usually, these studies include monozygotic twin pairs, where one twin has PTSD from combat-related trauma, while their co-twin did not experience combat trauma nor has a PTSD diagnosis. A separate monozygotic twin pair contains a cotwin who experienced combat-related trauma but did not develop PTSD, and their cotwin did not experience combat-related trauma nor develop PTSD [113]. Again, limitations exist in this design, including an inability to determine whether the findings are attributed to heredity or shared environments.
Lastly, while not optimal, cross-sectional studies that explore brain alterations in three groups, PTSD, TENC, and HC, can provide some insight into whether alterations are PTSD-specific or related to trauma exposure.
Structural neuroimaging
Adults
Few structural imaging studies have used prospective longitudinal designs in the past decade. Studies that scanned participants pre-trauma and post-trauma found reduced hippocampal volume [68, 114], post-pre-trauma orbitofrontal cortex (OFC) volume, and pre-trauma ventral ACC were related to greater PTSD symptom severity post-trauma [115]. It is important to highlight that these studies had relatively small sample sizes (n < 50). One large study (n = 210) that scanned police recruits found smaller pre-trauma dentate gyrus volume was associated with greater PTSD symptom severity post-trauma and that experiencing more police-related trauma between scan assessments was related to an increase in the volume of the basal nucleus of the amygdala [116]. It should be noted that the studies reviewed consisted of resilient individuals, with many participants without a PTSD diagnosis.
Numerous recent longitudinal studies have investigated how structural neuroimaging data collected shortly after trauma correlate with or predict PTSD symptoms. Most of these studies supported the hypothesis that decreased hippocampal volume early post-trauma is a risk factor for the development of chronic PTSD [117,118,119,120,121]. However, one study found no associations between hippocampal volume, or any of its subregions, and PTSD symptoms across time [122]. These differences are likely due to differences in trauma experienced, the timing of neuroimaging measurements, analytic strategy, and other sample characteristics [122]. Reduced FA of the UF [123, 124] and greater FA of the dorsal cingulum [125] collected early post-trauma predicted greater PTSD symptoms at 3 months, 6 months, and 4 years later (respectively).
Cross-sectional studies comparing three groups - PTSD, TENC, and HC - found reduced hippocampal [126,127,128] and right amygdala volume [128] in the PTSD and TENC groups compared to the HC group. However, one study found that only the PTSD group showed significantly less hippocampal volume compared to the TENC and HC groups [129]. When examining hippocampal subregions, the CA1 and CA2-3/DG were significantly smaller in PTSD patients than in TENC and HC groups [130]. Differences in findings may be attributed to different trauma types endured, as has been found previously [131]. For example, the studies that found differences only in the PTSD group used samples that experienced combat-related trauma [129] or a terrorist attack [130] versus the loss of a loved one [126, 127] or a natural disaster [128].
Functional MRI
Adults
Using a prospective longitudinal study design, Admon and colleagues (2013) found that service members who exhibited reduced hippocampal volume post-pre-trauma also displayed reduced hippocampus-vmPFC FC, which was related to greater PTSD symptoms post-trauma [68]. In a separate study from the same research group, the authors found that greater amygdala activation in response to risk anticipation at pre- and post-trauma was related to more PTSD symptoms post-trauma [132] and reduced nucleus accumbens activation to reward post-trauma was related to greater PTSD symptoms post-trauma [132]. Zhang and colleagues (2022) [133] recently used a network-based approach to measure stress-induced connectivity, changing patterns of large-scale brain networks at baseline to the subsequent symptom development post-trauma. In this prospective sample of police trainees, increased coupling between the SN and anterior cerebellum was observed in participants with greater PTSD symptoms (particularly intrusion symptoms) [133]. Nevertheless, as this work focused on a relatively healthy and resilient sample, future studies in more severe PTSD samples are needed.
Greater hippocampal activation, collected early post-trauma, during fear extinction [134], but not when looking at fearful versus neutral face stimuli [135], predicted more severe PTSD symptoms at 3 months post-trauma. In comparison, lesser hippocampal activation during response inhibition predicted greater PTSD symptom severity post-trauma [136]. Highlighting the unique contribution of the hippocampus in these different constructs. Greater amygdala activation early post-trauma when viewing fearful facial expressions significantly predicted symptoms at 3 [137] and 12 months post-trauma [138]. In combat veterans, greater dACC activation to negative images predicted greater PTSD symptom severity four years later [125]. Similarly, more negative amygdala-cerebellum FC at rest and amygdala-post-central gyrus FC during trauma recall at 2 weeks post-trauma predicted 6-month PTSD symptom severity post-trauma [139]. In a longitudinal study of n = 171 recent trauma survivors, PTSD severity at 14 months after trauma was associated with decreased neural activity in the ventral striatum (VS) and the amygdala toward rewards versus punishments at 1 month after trauma [140]. Surprisingly, decreased VS activity and connectivity with the vmPFC were more predictive of PTSD symptoms compared to the amygdala’s activity, highlighting the important role of reward processing in PTSD development or recovery [140]. Similarly, lesser activation in cortical regions early post-trauma during fear conditioning [141] and response inhibition [142] is related to greater PTSD symptoms 3 and 6 month post-trauma, respectively. However, greater dmPFC activation to fearful versus neutral face stimuli early post-trauma was associated with greater PTSD symptoms 3 months later [137]. Finally, a longitudinal study showed that while FC changes at 3 weeks post-trauma involved the DMN and frontal–limbic–striatal network, only changes in the DMN persisted at the 2 year follow-up [143].
Using a three-group design, one study examined the neural correlates of memory suppression in PTSD and found that the PTSD and TENC groups exhibited disrupted MFG activation while attempting memory suppression compared to HC, suggesting that disruptions in the MFG are apparent even in those trauma-exposed, regardless of PTSD status [144]. Regional parameters of the insular lobe, putamen, and precuneus of typhoon-related PTSD patients, TENC, were abnormal compared to HCs [145].
Recent twin studies have shown that PTSD patients exhibit reduced activation in the rostral ACC and MFG compared to their non-trauma-exposed cotwins and trauma-exposed individuals without PTSD. This diminished response, observed during exposure to trauma-related cues and to surprised faces, indicates that changes in these cortical areas are likely acquired traits of the disorder [146, 147].
Youth
One study found that increased hippocampal activation to threatening images over one year predicted a non-remitting PTSD trajectory, compared to a remission trajectory and HC groups [148].
Summary
Overall, across longitudinal prospective study designs and studies utilizing three groups, hippocampal alterations (lesser hippocampal volume and function) appear to be a pre-exposure risk factor for the development of PTSD [68, 114, 116,117,118,119,120,121, 126,127,128,129,130, 134,135,136]. Creating interventions that promote hippocampal neurogenesis will be important to use to prevent the development of PTSD early after trauma. Furthermore, alterations in cortical regions such as the vmPFC, ACC, and MFG are apparent early after trauma and predictive of later PTSD symptoms [115, 125, 137, 138, 141, 142, 144,145,146,147]. As such, interventions introduced early post-trauma that promote greater FC between frontal-limbic networks can potentially strengthen these connections. There are many limitations to the studies reviewed above, including limited sample sizes, many of the longitudinal studies reviewed included participants with sub-threshold PTSD, and there was not much variability concerning trauma type. Thus, the generalizability of the findings across trauma types is questionable. For a pictorial overview of findings, see Fig. 1.
Question 2: which neural correlates predict treatment outcomes and define treatment improvement?
To date, while trauma-focused cognitive behavioral therapies are gold-standard treatment options for PTSD, many people do not respond well to treatment [19, 20]. Uncovering the neural mechanisms that predict symptom improvement and define treatment response will be crucial in helping guide clinician-decision making and provide a more precision-medicine approach to treatment. Given the recent reviews published on this topic [40, 149,150,151], we review studies not included in these reviews, provide an overall summary of findings, and discuss limitations.
Baseline prediction of PTSD symptom improvement
Adults
In females who developed PTSD as a result of interpersonal trauma, pre-treatment FA values of the internal capsule, cingulate gyrus, superior longitudinal fasciculus, and splenium of the corpus callosum were positively correlated with changes in PTSD symptoms after cognitive processing therapy [152]. One study showed that lesser pre-treatment amygdala activation and greater MFG to fearful versus happy facial expressions were associated with a better response to prolonged exposure therapy (PE) [153]. Furthermore, this study found a greater decrease in the amygdala activation across blocks of fearful facial expression was associated with better symptomatic improvement [153]. Lower pre-treatment vmPFC-amygdala connectivity during an emotional face-viewing task predicted symptom improvement in individuals with PTSD, an effect that was strongest in individuals who received ketamine (versus midazolam) [154]. Additionally, this study showed symptom improvement following ketamine was predicted by decreased dACC activity during an emotional conflict regulation task and an increased resting-state FC between the vmPFC and anterior insula [154]. On the other hand, ketamine did not promote a greater increase in amygdala-mPFC resting-state FC but elicited a stronger transient decrease in vmPFC-amygdala compared to midazolam [155]. A longitudinal resting-state fMRI study employing support vector machine learning highlighted the precuneus, dmPFC, lingual gyrus, supplementary motor area, and cerebellum showed the highest prognostic remittance value from paroxetine treatment [156]. Lastly, Korgaonkar and colleagues (2020) found that lower pre-treatment connectivity in the cingulo-opercular, salience, and dorsal attention networks was associated with a better response to trauma-focused cognitive behavioral therapy (TF-CBT) [157].
Youth
Few studies have explored whether neuroimaging measures can predict treatment response in youth diagnosed with PTSD. Decreased pre-treatment activation in the posterior cingulate, mid-cingulate, and hippocampus predicted greater symptom improvement [158]. Another study trained a support vector machine from brain networks created from an ICA, finding that the bilateral superior temporal gyrus center network distinguished between non-responders and responders to trauma-focused therapies [159]. This may indicate that auditory processing and social cognition may be important for PTSD remission [160]. Girls who experienced greater reductions in PTSD symptoms exhibited decreased amygdala-insula connectivity during reappraisal compared to those experiencing milder reductions [161].
Neuroimaging correlates of PTSD symptom improvement
Adults
Increased hippocampal volume appeared in PTSD patients who completed CBT [162], eye-movement desensitization and realization (EMDR) alone [163] or paired with a Tetris video game intervention [164], and in those who remitted following psychotherapy [165]. Over time, lesser dorsal cingulum FA was found in individuals whose PTSD symptoms decreased after trauma-focused treatment [166]. Interestingly, recent work reported the normalization of CEN connectivity following cognitive processing therapy for PTSD [167]. Greater reduction in PTSD symptoms was associated with larger pre- to post-treatment increases in the inferior frontal junction inhibition of the amygdala [168]. PTSD patients who showed clinical improvement exhibited a reduced relative influence of the anterior insula over motor, affective, and self-other distinction regions [169]. Upon completion of PE, PTSD patients showed increased pre-post FC in basolateral amygdala-OFC, centromedial amygdala-OFC, and hippocampus-vmPFC. In contrast, TENC saw no significant pre-post changes in connectivity after PE, suggesting that amygdala FC normalized similarly to TENC [170]. One study showed that a reduction in PTSD symptom severity was associated with decreased connectivity between the visual cortex and temporal lobe regions and increased connectivity between the superior frontal gyrus and temporal pole regions after EMDR and TF-CBT, suggesting minor differences exist in neurophysiological outcome that is therapy-specific, particularly in those who experienced natural-disaster [171].
Summary
Overall, the studies reviewed here and previously published reviews [40, 149,150,151] suggest that treatment non-response in adults was predicted by greater activation in regions responsible for threat detection, lesser activation in emotion regulation, executive function, and contextual processing regions, and altered crosstalk between regions within the DMN and regions important in emotion processing, cognitive function, and salience. In youth, studies are sparse but show a pattern of greater activation in memory-related regions, while lesser connectivity between fear learning-related regions predicted symptom reduction. There are many limitations of the studies reviewed. First, given the stringent inclusion/exclusion criteria many of these intervention studies endorse, their sample sizes are limited. Second, the definition of a responder versus a non-responder to treatment is not objective, and studies define this differently. Third, some variables are not controlled for, making it hard to determine the effect of treatment. For example, no direct comparison exists between groups undergoing different treatment options. Fourth, the analyses are largely ROI-specific. Fifth, no study have examined longitudinal treatment response outcomes. Lastly, many studies did not include a wait-list control group; only one study explored neural differences in treatment response between treatment types. For a pictorial overview of findings, see Fig. 2.
Question 3: are there neuroimaging-based biotypes that define PTSD?
Psychiatry is moving towards a more precision-medicine approach, aiming to improve objective diagnosis, prediction, and treatment of mental disorders. Currently, to be diagnosed with PTSD, participants need to meet a certain number of symptoms that are largely self-reported and subjective, making the disorder highly heterogeneous [172]. To overcome the weak link between subjective-based diagnostic methods and objective-based neuroimaging assessments, recent studies have aimed to stratify PTSD to identify consistent subgroups based on objective brain-based markers [173,174,175]. Accordingly, Stevens and colleagues (2021) conducted a pioneering study to identify brain-based biotypes of psychiatric vulnerability shortly after trauma [176]. Using two cohorts from the AURORA longitudinal study of trauma survivors (n = 69 discovery cohort; n = 77 internal replication cohort) [112], the authors found and replicated three clusters based on early post-trauma brain activity during fMRI tasks assessing threat and reward reactivity, as well as response inhibition. These clusters were associated with distinct clinical trajectories up to 6 months post-trauma, with the group showing increased reactivity to threat and reward experiencing the most severe subsequent PTSD and anxiety symptoms [176]. In collaboration with Stevens and colleagues, Ben-Zion and colleagues (2023) conducted a conceptual replication of these brain-based biotypes [177] using a comparable dataset from the NMPTDT longitudinal study of trauma survivors [111]. While the authors found four clusters based on task-based fMRI data, they were not identical to the previously identified biotypes and were associated with prospective PTSD or anxiety symptoms. While there were many differences between the studies (AURORA and NMPTDT) that could contribute to the non-replication, this study highlights that additional replication studies are needed to identify more stable and generalizable neuroimaging-based biotypes before treatment implications can be fully realized [177, 178].
Overall implications, future directions, and limitations
This narrative review aimed at exploring progress made in the past decade on three major questions in the field: (1) Which neural alterations serve as predisposing (pre-exposure) risk factors for PTSD development, and which are acquired (post-exposure)? (2) Which neural alterations can predict treatment outcomes and define clinical improvement? and (3) Can neuroimaging measures be used to define brain-based biotypes of PTSD? We present a synthesis of neuroimaging studies from the past decade in adults and youth with PTSD. Below, we present implications, provide areas of future research to be explored for each question, and highlight the limitations of our narrative review.
In the past decade, neuroimaging research on PTSD has advanced our understanding of the causal pathways of neural alterations within the disorder. However, we still cannot use the current neuroimaging knowledge to predict PTSD symptom trajectories or improve prevention and treatment options. Many of the above findings require replication in larger and more diverse samples with different trauma types across different methodologies. Importantly, future models used to determine the risk of developing trauma-related psychopathology will likely include information regarding demographics, socioeconomic status, and other clinical characteristics; thus, it is important to consider these factors when designing forthcoming studies. In the last ten years, we have seen a surge of longitudinal studies that collect neuroimaging measures early post-trauma and again at subsequent time points. While such studies are resource-intensive, scientists can answer questions not asked before, largely because of the development of large collaborations across multiple sites such as NMPTDT and AURORA research initiatives. The continuation and creation of more collaborations like these, with a focus on the collection of neuroimaging data shortly after trauma (and if possible, even pre-trauma) and at subsequent time points post-trauma, will be crucial in providing evidence to answer the vulnerability versus acquired characteristics of PTSD. To capture the dynamic evolution of the post-traumatic stress response, it is essential to incorporate multiple time points and ensure an adequately long follow-up period post-trauma (e.g., more than a year post-trauma), during which most of the recovery is anticipated.
Much work has been done to determine neural pre-treatment predictors of response and whether treatment normalizes alterations found in the disorder. While we have a relative understanding of potential predictors and changes associated with treatment response, much work still needs to be done to use this information in the clinic. Many of the studies reviewed had small sample sizes, used different treatment options, and samples were not diverse regarding sociodemographic factors and trauma type. Future studies should seek to replicate previous findings with bigger sample sizes, comparisons should be made between treatments, and more community-based samples should be prioritized.
The significant clinical heterogeneity observed in PTSD (and other post-traumatic psychopathologies), coupled with recent advancements in statistical and computational techniques, has spurred the pursuit of identifying homogeneous PTSD subtypes using data-driven methodologies. However, the assumption of distinct and homogeneous subgroups may not be clinically useful or accurately reflect the underlying biology of PTSD. For instance, most clustering methods will invariably produce clusters, even without any inherent data structure, highlighting the importance of differentiating between biologically and clinically relevant subtypes and random data fluctuations or noise [179, 180]. Future research aiming to identify brain-based biotypes of PTSD will benefit from global collaborations between research teams, combining unique large-scale datasets and sharing of analytic pipelines (as exemplified recently by Stevens [176] and Ben-Zion [177]). Furthermore, subsequent studies will benefit from employing hybrid methodologies that integrate theory- and data-driven approaches Field [195,196] and implementing open science protocols (e.g., preregistration, transparent reporting of all results).
Few investigations explored here explicitly examined sex as a biological variable. As has been recently reviewed [13], the underlying neurobiological correlates of sex differences in PTSD are unknown. Most of the studies discussed here did not include a direct comparison between males and females. However, a handful of studies did examine female-only or male-only samples, which do not allow for the generalization of findings to the opposite sex. Thus, more studies should examine sex differences in their samples.
We have highlighted findings in youth. Still, much more work is needed to parse better the brain’s natural development versus the impact trauma may have on brain regions. Few studies have explored the questions posed in youth samples. Though resources are a limiting factor, future studies should execute longitudinal study designs that start in youth to determine the role of childhood trauma, potentially before it happens, in the development of trauma-related psychopathology in adulthood. Additionally, genetic and neurobiological studies linking transgenerational PTSD presentation would be beneficial in parsing preventative markers for developing PTSD. Thus, focusing on youth populations would be optimal in answering our first main question.
Limitations
There are notable strengths of this narrative review, including providing a synthesis of neuroimaging studies in both adult and youth samples that explore three leading questions in the PTSD field. Despite these strengths, limitations do exist. First, the authors have tried to include all the pertinent studies to answer the three questions, though a systematic protocol was not used when exploring studies. Second, given the number of studies available to be reviewed, the conclusions drawn from each question are limited. Further, as outlined above, methodological variability exists in the studies reviewed, including differences in scanning parameters and PTSD samples. This variability limits the reliability and validity of the conclusions made. Regardless of these limitations, this review is important as it provides insight into where the field stands on these three questions, highlighting that much research still needs to be conducted to make stronger conclusions.
Despite the limitations of the studies reviewed and of this narrative review, PTSD neuroimagers have made much progress in the last decade and have much more to make, especially in answering questions related to disparities in the development of the disorder and translating the knowledge collected beyond academia, to the communities we serve.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5TM, 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc.; 2013. xliv, 947 p. (Diagnostic and statistical manual of mental disorders: DSM-5TM, 5th ed).
Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016;46:327–43.
Paganin W, Signorini S. Biomarkers of post-traumatic stress disorder from emotional trauma: a systematic review. Eur J Trauma Dissociation. 2023;7:100328.
Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Psychol Trauma Theory Res Pr Policy. 2008;S:101–13.
Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev. 2018;63:41–55.
McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, et al. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2013;52:815–830.e14.
Blom M, Oberink R. The validity of the DSM-IV PTSD criteria in children and adolescents: a review. Clin Child Psychol Psychiatry. 2012;17:571–601.
Ramsdell KD, Smith AJ, Hildenbrand AK, Marsac ML. Posttraumatic stress in school-age children and adolescents: medical providers’ role from diagnosis to optimal management. Pediatr Health Med Ther. 2015;6:167–80.
Cover KK, Maeng LY, Lebrón-Milad K, Milad MR. Mechanisms of estradiol in fear circuitry: implications for sex differences in psychopathology. Transl Psychiatry. 2014;4:e422–e422.
Miller-Graff LE, Howell KH. Posttraumatic stress symptom trajectories among children exposed to violence. J Trauma Stress. 2015;28:17–24.
Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132:959–92.
Helpman L, Zhu X, Suarez-Jimenez B, Lazarov A, Monk C, Neria Y. Sex differences in trauma-related psychopathology: a critical review of neuroimaging literature (2014–2017). Curr Psychiatry Rep. 2017;19:104.
Eder-Moreau E, Zhu X, Fisch CT, Bergman M, Neria Y, Helpman L. Neurobiological alterations in females with PTSD: a systematic review. Front Psychiatry. 2022 ;13:862476.
Brunello N, Davidson JR, Deahl M, Kessler RC, Mendlewicz J, Racagni G, et al. Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology. 2001;43:150–62.
Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Physical Health Conditions Associated with Posttraumatic Stress Disorder in U.S. Older Adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Am Geriatr Soc. 2012;60:296–303.
Fani N, Jain J, Hudak LA, Rothbaum BO, Ressler KJ, Michopoulos V. Post-trauma anhedonia is associated with increased substance use in a recently-traumatized population. Psychiatry Res. 2020;285:112777.
Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61:22–32.
Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. J Consult Clin Psychol. 2005;73:953–64.
Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71:134–68.
Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005 ;162:214–27.
Schnurr PP, Chard KM, Ruzek JI, Chow BK, Resick PA, Foa EB, et al. Comparison of prolonged exposure vs cognitive processing therapy for treatment of posttraumatic stress disorder among US veterans: a randomized clinical trial. JAMA Netw Open. 2022;5:e2136921.
Lewis C, Roberts NP, Gibson S, Bisson JI. Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: systematic review and meta-analysis. Eur J Psychotraumatol. 2020;11:1709709.
Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG. Treatment barriers for low-income, urban african americans with undiagnosed posttraumatic stress disorder. J Trauma Stress. 2008;21:218–22.
Cipriani A, Williams T, Nikolakopoulou A, Salanti G, Chaimani A, Ipser J, et al. Comparative efficacy and acceptability of pharmacological treatments for post-traumatic stress disorder in adults: a network meta-analysis. Psychol Med. 2018;48:1975–84.
Henner RL, Keshavan MS, Hill KP. Review of potential psychedelic treatments for PTSD. J Neurol Sci. 2022;439:120302.
Krediet E, Bostoen T, Breeksema J, van Schagen A, Passie T, Vermetten E. Reviewing the potential of psychedelics for the treatment of PTSD. Int J Neuropsychopharmacol. 2020;23:385–400.
Barawi KS, Lewis C, Simon N, Bisson JI. A systematic review of factors associated with outcome of psychological treatments for post-traumatic stress disorder. Eur J Psychotraumatol. 2020;11:1774240.
Merz J, Schwarzer G, Gerger H. Comparative efficacy and acceptability of pharmacological, psychotherapeutic, and combination treatments in adults with posttraumatic stress disorder: a network meta-analysis. JAMA Psychiatry. 2019;76:904–13.
Bremner JD, Randall P, Scott TM, Bronen RA, Seibyl JP, Southwick SM, et al. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152:973–81.
Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. Longo DL, editor. N Engl J Med. 2017;376:2459–69.
Liberzon I, Abelson JL. Context processing and the neurobiology of post-traumatic stress disorder. Neuron. 2016;92:14–30.
Patel R, Spreng RN, Shin LM, Girard TA. Neurocircuitry models of posttraumatic stress disorder and beyond: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev. 2012;36:2130–42.
Pitman RK, Rasmusson AM, Koenen KC, Shin LM, Orr SP, Gilbertson MW, et al. Biological studies of posttraumatic stress disorder. Nat Rev Neurosci. 2012;13:769–87.
Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research-past, present, and future. Biol Psychiatry. 2006;60:376–82.
Ross MC, Cisler JM. Altered large-scale functional brain organization in posttraumatic stress disorder: A comprehensive review of univariate and network-level neurocircuitry models of PTSD. NeuroImage Clin. 2020;27:102319.
Shin LM, Rauch SL, Pitman RK. Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann N. Y Acad Sci. 2006;1071:67–79.
O’Doherty DCM, Chitty KM, Saddiqui S, Bennett MR, Lagopoulos J. A systematic review and meta-analysis of magnetic resonance imaging measurement of structural volumes in posttraumatic stress disorder. Psychiatry Res Neuroimaging. 2015;232:1–33.
Hinojosa CA. Does hippocampal volume in patients with posttraumatic stress disorder vary by trauma type? Harv Rev Psychiatry. 2022;30:118.
Ben-Zion Z, Korem N, Fine N, Katz S, Siddhanta M, Funaro MC, et al. Structural neuroimaging of hippocampus and amygdala subregions in post-traumatic stress disorder (PTSD): a scoping review. Biol Psychiatry Glob Open Sci [Internet]. 2023 [cited 2023 Aug 29]; Available from: https://www.sciencedirect.com/science/article/pii/S2667174323000812.
van Rooij SJH, Sippel LM, McDonald WM, Holtzheimer PE. Defining focal brain stimulation targets for PTSD using neuroimaging. Depress Anxiety. 2021. https://doi.org/10.1002/da.23159.
Backhausen LL, Herting MM, Tamnes CK, Vetter NC. Best practices in structural neuroimaging of neurodevelopmental disorders. Neuropsychol Rev. 2022;32:400–18.
Figley CR, Uddin MN, Wong K, Kornelsen J, Puig J, Figley TD. Potential pitfalls of using fractional anisotropy, axial diffusivity, and radial diffusivity as biomarkers of cerebral white matter microstructure. Front Neurosci [Internet]. 2022 [cited 2023 Sep 14];15. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2021.799576.
Bassett DS, Sporns O. Network neuroscience. Nat Neurosci. 2017;20:353–64.
Wang X, Xie H, Chen T, Cotton AS, Salminen LE, Logue MW, et al. Cortical volume abnormalities in posttraumatic stress disorder: an ENIGMA-psychiatric genomics consortium PTSD workgroup mega-analysis. Mol Psychiatry. 2021;26:4331–43.
Baldaçara L, Zugman A, Araújo C, Cogo-Moreira H, Lacerda ALT, Schoedl A, et al. Reduction of anterior cingulate in adults with urban violence- related PTSD. J Affect Disord. 2014;168:13–20.
Roy O, Levasseur-Moreau J, Renauld E, Hébert LJ, Leblond J, Bilodeau M, et al. Whole-brain morphometry in Canadian soldiers with posttraumatic stress disorder. Ann NY Acad Sci. 2022;1509:37–49.
Li L, Zhang Y, Zhao Y, Li Z, Kemp GJ, Wu M, et al. Cortical thickness abnormalities in patients with post-traumatic stress disorder: a vertex-based meta-analysis. Neurosci Biobehav Rev. 2022;134:104519.
Koch SBJ, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, Olff M. Decreased uncinate fasciculus tract integrity in male and female patients with PTSD: a diffusion tensor imaging study. J Psychiatry Neurosci Jpn 2017;42:331–42.
O’Doherty DCM, Ryder W, Paquola C, Tickell A, Chan C, Hermens DF, et al. White matter integrity alterations in post‐traumatic stress disorder. Hum Brain Mapp. 2017;39:1327–38.
Olson EA, Cui J, Fukunaga R, Nickerson LD, Rauch SL, Rosso IM. Disruption of white matter structural integrity and connectivity in posttraumatic stress disorder: A TBSS and tractography study. Depress Anxiety. 2017;34:437–45.
Ju Y, Ou W, Su J, Averill CL, Liu J, Wang M, et al. White matter microstructural alterations in posttraumatic stress disorder: An ROI and whole-brain based meta-analysis. J Affect Disord. 2020;266:655–70.
van Rooij SJH, Rademaker AR, Kennis M, Vink M, Kahn RS, Geuze E. Neural correlates of trauma-unrelated emotional processing in war veterans with PTSD. Psychol Med. 2015;45:575–87.
Mazza M, Tempesta D, Pino MC, Catalucci A, Gallucci M, Ferrara M. Regional cerebral changes and functional connectivity during the observation of negative emotional stimuli in subjects with post-traumatic stress disorder. Eur Arch Psychiatry Clin Neurosci. 2013;263:575–83.
Mazza M, Tempesta D, Pino MC, Nigri A, Catalucci A, Guadagni V, et al. Neural activity related to cognitive and emotional empathy in post-traumatic stress disorder. Behav Brain Res. 2015;282:37–45.
Moser DA, Aue T, Suardi F, Kutlikova H, Cordero MI, Rossignol AS, et al. Violence-related PTSD and neural activation when seeing emotionally charged male–female interactions. Soc Cogn Affect Neurosci. 2015;10:645.
Offringa R, Handwerger Brohawn K, Staples LK, Dubois SJ, Hughes KC, Pfaff DL, et al. Diminished rostral anterior cingulate cortex activation during trauma-unrelated emotional interference in PTSD. Biol Mood Anxiety Disord. 2013;3:1–6.
Stevens JS, Jovanovic T, Fani N, Ely TD, Glover EM, Bradley B, et al. Disrupted amygdala-prefrontal functional connectivity in civilian women with posttraumatic stress disorder. J Psychiatr Res. 2013;47:1469–78.
Killgore WDS, Britton JC, Schwab ZJ, Price LM, Weiner MR, Gold AL, et al. Cortico-limbic responses to masked affective faces across ptsd, panic disorder, and specific phobia. Depress Anxiety. 2014;31:150–9.
Stevens JS, Almli LM, Fani N, Gutman DA, Bradley B, Norrholm SD, et al. PACAP receptor gene polymorphism impacts fear responses in the amygdala and hippocampus. Proc Natl Acad Sci. 2014;111:3158–63.
Neumeister, Feldker P, Heitmann K, Helmich CY, Gathmann R, Becker MPI B, et al. Interpersonal violence in posttraumatic women: brain networks triggered by trauma-related pictures. Soc Cogn Affect Neurosci. 2017;12:555–68.
Xiong K, Zhang Y, Qiu M, Zhang J, Sang L, Wang L, et al. Negative emotion regulation in patients with posttraumatic stress disorder. PLoS ONE. 2013;12:e81957.
Bruce SE, Buchholz KR, Brown WJ, Yan L, Durbin A, Sheline YI. Altered emotional interference processing in the amygdala and insula in women with Post-Traumatic Stress Disorder. NeuroImage Clin 2012;2:43–9.
Garfinkel SN, Abelson JL, King AP, Sripada RK, Wang X, Gaines LM, et al. Impaired contextual modulation of memories in PTSD: an fMRI and psychophysiological study of extinction retention and fear renewal. J Neurosci J Soc Neurosci. 2014;34:13435–43.
Morey RA, Dunsmoor JE, Haswell CC, Brown VM, Vora A, Weiner J, et al. Fear learning circuitry is biased toward generalization of fear associations in posttraumatic stress disorder. Transl Psychiatry. 2015;5:e700.
Diener SJ, Nees F, Wessa M, Wirtz G, Frommberger U, Penga T, et al. Reduced amygdala responsivity during conditioning to trauma-related stimuli in posttraumatic stress disorder. Psychophysiology. 2016;53:1460–71.
Bressler SL, Menon V. Large-scale brain networks in cognition: emerging methods and principles. Trends Cogn Sci. 2010;14:277–90.
Menon V, Uddin LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. 2010;214:655–67.
Admon R, Leykin D, Lubin G, Engert V, Andrews J, Pruessner J, et al. Stress-induced reduction in hippocampal volume and connectivity with the ventromedial prefrontal cortex are related to maladaptive responses to stressful military service. Hum Brain Mapp. 2013;34:2808–16.
Bao W, Gao Y, Cao L, Li H, Liu J, Liang K, et al. Alterations in large-scale functional networks in adult posttraumatic stress disorder: A systematic review and meta-analysis of resting-state functional connectivity studies. Neurosci Biobehav Rev. 2021;131:1027–36.
Koch SBJ, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, Olff M. Aberrant resting-state brain activity in posttraumatic stress disorder: a meta-analysis and systematic review. Depress Anxiety. 2016;33:592–605.
Akiki TJ, Averill CL, Abdallah CG. A network-based neurobiological model of PTSD: evidence from structural and functional neuroimaging studies. Curr Psychiatry Rep. 2017;19:81.
Fenster RJ, Lebois LAM, Ressler KJ, Suh J. Brain circuit dysfunction in post-traumatic stress disorder: from mouse to man. Nat Rev Neurosci. 2018;19:535–51.
Neria Y. Functional neuroimaging in PTSD: from discovery of underlying mechanisms to addressing diagnostic heterogeneity. Am J Psychiatry. 2021;178:128–35.
Norbury A, Seeley SH, Perez-Rodriguez MM, Feder A. Functional neuroimaging of resilience to trauma: convergent evidence and challenges for future research. Psychol Med. 2023;53:3293–305.
Reuveni I, Bonne O, Giesser R, Shragai T, Lazarovits G, Isserles M, et al. Anatomical and functional connectivity in the default mode network of post‐traumatic stress disorder patients after civilian and military‐related trauma. Hum Brain Mapp. 2015;37:589–99.
Shang J, Lui S, Meng Y, Zhu H, Qiu C, Gong Q, et al. Alterations in low-level perceptual networks related to clinical severity in ptsd after an earthquake: a resting-state fMRI study. PLOS ONE. 2014;9:e96834.
Zhang Y, Liu F, Chen H, Li M, Duan X, Xie B, et al. Intranetwork and internetwork functional connectivity alterations in post-traumatic stress disorder. J Affect Disord. 2015 ;187:114–21.
Tursich M, Ros T, Frewen PA, Kluetsch RC, Calhoun VD, Lanius RA. Distinct intrinsic network connectivity patterns of post-traumatic stress disorder symptom clusters. Acta Psychiatr Scand. 2015;132:29–38.
Rabellino D, Tursich M, Frewen PA, Daniels JK, Densmore M, Théberge J, et al. Intrinsic connectivity networks in post-traumatic stress disorder during sub- and supraliminal processing of threat-related stimuli. Acta Psychiatr Scand. 2015;132:365–78.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Lei D, Li K, Li L, Chen F, Huang X, Lui S, et al. Disrupted functional brain connectome in patients with posttraumatic stress disorder. Radiology. 2015;276:818–27.
Watts DJ, Strogatz SH. Collective dynamics of ‘small-world’ networks. Nature. 1998;393:440–2.
Zhang XD, Yin Y, Hu XL, Duan L, Qi R, Xu Q, et al. Altered default mode network configuration in posttraumatic stress disorder after earthquake: A resting-stage functional magnetic resonance imaging study. Med (Baltim). 2017;96:e7826.
Akiki TJ, Averill CL, Wrocklage KM, Scott JC, Averill LA, Schweinsburg B, et al. Default mode network abnormalities in posttraumatic stress disorder: A novel network-restricted topology approach. NeuroImage. 2018;176:489–98.
Spielberg JM, McGlinchey RE, Milberg WP, Salat DH. Brain network disturbance related to posttraumatic stress and traumatic brain injury in veterans. Biol Psychiatry. 2015;78:210–6.
Giedd JN, Raznahan A, Alexander-Bloch A, Schmitt E, Gogtay N, Rapoport JL. Child psychiatry branch of the national institute of mental health longitudinal structural magnetic resonance imaging study of human brain development. Neuropsychopharmacology. 2015;40:43–9.
Tau GZ, Peterson BS. Normal development of brain circuits. Neuropsychopharmacology. 2010;35:147–68.
Fields RD, Stevens-Graham B. New insights into neuron-glia communication. Science. 2002;298:556–62.
Peterson M, Warf BC, Schiff SJ. Normative human brain volume growth. J Neurosurg Pediatr. 2018;21:478–85.
Jeong HJ, Durham EL, Moore TM, Dupont RM, McDowell M, Cardenas-Iniguez C, et al. The association between latent trauma and brain structure in children. Transl Psychiatry. 2021;11:1–9.
Morey RA, Haswell CC, Hooper SR, De Bellis MD. Amygdala, hippocampus, and ventral medial prefrontal cortex volumes differ in maltreated youth with and without chronic posttraumatic stress disorder. Neuropsychopharmacology. 2016;41:791–801.
Phillips RD, De Bellis MD, Brumback T, Clausen AN, Clarke-Rubright EK, Haswell CC, et al. Volumetric trajectories of hippocampal subfields and amygdala nuclei influenced by adolescent alcohol use and lifetime trauma. Transl Psychiatry. 2021;11:1–13.
Kribakaran S, Danese A, Bromis K, Kempton MJ, Gee DG. Meta-analysis of structural magnetic resonance imaging studies in pediatric posttraumatic stress disorder and comparison with related conditions. Biol Psychiatry Cogn Neurosci Neuroimag. 2020;5:23–34.
Postel C, Viard A, André C, Guénolé F, de Flores R, Baleyte J, et al. Hippocampal subfields alterations in adolescents with post‐traumatic stress disorder. Hum Brain Mapp. 2018;40:1244–52.
Keding TJ, Herringa RJ. Abnormal structure of fear circuitry in pediatric post-traumatic stress disorder. Neuropsychopharmacology. 2015;40:537–45.
Rinne-Albers MA, Boateng CP, van der Werff SJ, Lamers-Winkelman F, Rombouts SA, Vermeiren RR, et al. Preserved cortical thickness, surface area and volume in adolescents with PTSD after childhood sexual abuse. Sci Rep. 2020;10:3266.
Heyn SA, Bailowitz S, Russell JD, Herringa RJ. Sex-based variations of prefrontal structure and longitudinal symptoms in pediatric posttraumatic stress disorder. Depress Anxiety. 2022;39:902–12.
Russell JD, Heyn SA, Dean DC, Herringa RJ. Pediatric PTSD is characterized by age- and sex-related abnormalities in structural connectivity. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2021;46:2217–23.
Siehl S, Wicking M, Pohlack S, Winkelmann T, Zidda F, Steiger-White F, et al. Structural white and gray matter differences in a large sample of patients with Posttraumatic Stress Disorder and a healthy and trauma-exposed control group: Diffusion tensor imaging and region-based morphometry. NeuroImage Clin. 2020;28:102424.
Rinne-Albers MAW, van der Werff SJA, van Hoof MJ, van Lang ND, Lamers-Winkelman F, Rombouts SA, et al. Abnormalities of white matter integrity in the corpus callosum of adolescents with PTSD after childhood sexual abuse: a DTI study. Eur Child Adolesc Psychiatry. 2016;25:869–78.
Zhang Y, Wei H, Cronin MJ, He N, Yan F, Liu C. Longitudinal atlas for normative human brain development and aging over the lifespan using quantitative susceptibility mapping. NeuroImage. 2018;171:176–89.
Keding TJ, Herringa RJ. Paradoxical prefrontal–amygdala recruitment to angry and happy expressions in pediatric posttraumatic stress disorder. Neuropsychopharmacology. 2016;41:2903–12.
Wolf RC, Herringa RJ. Prefrontal-amygdala dysregulation to threat in pediatric posttraumatic stress disorder. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2016;41:822–31.
McLaughlin KA, Peverill M, Gold AL, Alves S, Sheridan MA. Child maltreatment and neural systems underlying emotion regulation. J Am Acad Child Adolesc Psychiatry. 2015;54:753–62.
Patriat R, Birn RM, Keding TJ, Herringa RJ. Default-mode network abnormalities in pediatric posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2016;55:319–27.
Viard A, Mutlu J, Chanraud S, Guenolé F, Egler PJ, Gérardin P, et al. Altered default mode network connectivity in adolescents with post-traumatic stress disorder. NeuroImage Clin. 2019;22:101731.
Suo X, Lei D, Li K, Chen F, Li F, Li L, et al. Disrupted brain network topology in pediatric posttraumatic stress disorder: a resting-state fMRI study. Hum Brain Mapp. 2015;36:3677–86.
Xu J, Chen F, Lei D, Zhan W, Sun X, Suo X, et al. Disrupted functional network topology in children and adolescents with post-traumatic stress disorder. Front Neurosci [Internet]. 2018 [cited 2023 Sep 13];12. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2018.00709.
Xu J, Chen F, Lei D, Zhan W, Sun X, Suo X, et al. Disrupted functional network topology in children and adolescents with post-traumatic stress disorder. Front Neurosci [Internet]. 2018 [cited 2023 Jul 14];12. Available from: https://www.frontiersin.org/articles/10.3389/fnins.2018.00709.
Admon R, Milad MR, Hendler T. A causal model of post-traumatic stress disorder: disentangling predisposed from acquired neural abnormalities. Trends Cogn Sci. 2013;17:337–47.
Ben-Zion Z, Fine NB, Keynan NJ, Admon R, Halpern P, Liberzon I, et al. Neurobehavioral moderators of post-traumatic stress disorder (PTSD) trajectories: study protocol of a prospective MRI study of recent trauma survivors. Eur J Psychotraumatology. 2019;10:1683941.
McLean SA, Ressler K, Koenen KC, Neylan T, Germine L, Jovanovic T, et al. The AURORA Study: a longitudinal, multimodal library of brain biology and function after traumatic stress exposure. Mol Psychiatry. 2020;25:283–96.
Pitman RK, Gilbertson MW, Gurvits TV, May FS, Lasko NB, Metzger LJ, et al. Clarifying the origin of biological abnormalities in PTSD through the study of identical twins discordant for combat exposure. Ann NY Acad Sci. 2006;1071:242–54.
Sekiguchi A, Kotozaki Y, Sugiura M, Nouchi R, Takeuchi H, Hanawa S, et al. Resilience after 3/11: structural brain changes 1 year after the Japanese earthquake. Mol Psychiatry. 2015;20:553–4.
Sekiguchi A, Sugiura M, Taki Y, Kotozaki Y, Nouchi R, Takeuchi H, et al. Brain structural changes as vulnerability factors and acquired signs of post-earthquake stress. Mol Psychiatry. 2013;18:618–23.
Koch SBJ, van Ast VA, Kaldewaij R, Hashemi MM, Zhang W, Klumpers F, et al. Larger dentate gyrus volume as predisposing resilience factor for the development of trauma-related symptoms. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2021;46:1283–92.
Xie H, Erwin MC, Elhai JD, Wall JT, Tamburrino MB, Brickman KR, et al. Relationship of hippocampal volumes and posttraumatic stress disorder symptoms over early post-trauma periods. Biol Psychiatry Cogn Neurosci Neuroimag. 2018;3:968–75.
Quidé Y, Andersson F, Dufour-Rainfray D, Descriaud C, Brizard B, Gissot V, et al. Smaller hippocampal volume following sexual assault in women is associated with post-traumatic stress disorder. Acta Psychiatr Scand. 2018;138:312–24.
Ben-Zion Z, Artzi M, Niry D, Keynan NJ, Zeevi Y, Admon R, et al. Neuroanatomical risk factors for posttraumatic stress disorder in recent trauma survivors. Biol Psychiatry Cogn Neurosci Neuroimag. 2020;5:311–9.
Ben-Zion Z, Korem N, Spiller TR, Duek O, Keynan JN, Admon R, et al. Longitudinal volumetric evaluation of hippocampus and amygdala subregions in recent trauma survivors. Mol Psychiatry. 2023;28:657–67.
Lindgren L, Bergdahl J, Nyberg L. Longitudinal evidence for smaller hippocampus volume as a vulnerability factor for perceived stress. Cereb Cortex. 2016;26:3527–33.
Weis CN, Webb EK, Huggins AA, Kallenbach M, Miskovich TA, Fitzgerald JM, et al. Stability of hippocampal subfield volumes after trauma and relationship to development of PTSD symptoms. NeuroImage. 2021;236:118076.
Harnett NG, Stevens JS, van Rooij SJH, Ely TD, Michopoulos V, Hudak L, et al. Multimodal structural neuroimaging markers of risk and recovery from posttrauma anhedonia: a prospective investigation. Depress Anxiety. 2021;38:79–88.
Fani N, Michopoulos V, van Rooij SJH, Clendinen C, Hardy RA, Jovanovic T, et al. Structural connectivity and risk for anhedonia after trauma: A prospective study and replication. J Psychiatr Res. 2019;116:34–41.
Kennis M, van Rooij SJH, Reijnen A, Geuze E. The predictive value of dorsal cingulate activity and fractional anisotropy on long-term PTSD symptom severity. Depress Anxiety. 2017;34:410–8.
Luo Y, Liu Y, Qin Y, Zhang X, Ma T, Wu W, et al. The atrophy and laterality of the hippocampal subfields in parents with or without posttraumatic stress disorder who lost their only child in China. Neurol Sci J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2017;38:1241–7.
Luo Y, Shan H, Liu Y, Wu L, Zhang X, Ma T, et al. Decreased left hippocampal volumes in parents with or without posttraumatic stress disorder who lost their only child in China. J Affect Disord. 2016;197:223–30.
Zhang L, Lu L, Bu X, Li H, Tang S, Gao Y, et al. Alterations in hippocampal subfield and amygdala subregion volumes in posttraumatic subjects with and without posttraumatic stress disorder. Hum Brain Mapp. 2021;42:2147–58.
van Rooij SJH, Kennis M, Sjouwerman R, van den Heuvel MP, Kahn RS, Geuze E. Smaller hippocampal volume as a vulnerability factor for the persistence of post-traumatic stress disorder. Psychol Med. 2015;45:2737–46.
Postel C, Mary A, Dayan J, Fraisse F, Vallée T, Guillery-Girard B, et al. Variations in response to trauma and hippocampal subfield changes. Neurobiol Stress. 2021;15:100346.
Hinojosa, CA Does Hippocampal Volume in Patients with Posttraumatic Stres…: Harvard Review of Psychiatry. [cited 2023 Aug 2]; Available from: https://journals.lww.com/hrpjournal/Abstract/2022/03000/Does_Hippocampal_Volume_in_Patients_with.3.aspx.
Admon R, Lubin G, Rosenblatt JD, Stern O, Kahn I, Assaf M, et al. Imbalanced Neural Responsivity to Risk and Reward Indicates Stress Vulnerability in Humans. Cereb Cortex. 2013;23:28–35.
Zhang W, Kaldewaij R, Hashemi MM, Koch SBJ, Smit A, van Ast VA, et al. Acute-stress-induced change in salience network coupling prospectively predicts post-trauma symptom development. Transl Psychiatry. 2022;12:1–8.
van Rooij SJH, Ravi M, Ely TD, Michopoulos V, Winters SJ, Shin J, et al. Hippocampal activation during contextual fear inhibition related to resilience in the early aftermath of trauma. Behav Brain Res. 2021;408:113282.
Tanriverdi, Gregory B, Olino DF, Ely TM, Harnett TD, Rooij NG, et al. Hippocampal threat reactivity interacts with physiological arousal to predict PTSD symptoms. J Neurosci. 2022;42:6593–604.
van Rooij SJH, Stevens JS, Ely TD, Hinrichs RC, Michopoulos V, Winters SJ, et al. The role of the hippocampus in predicting future PTSD symptoms in recently traumatized civilians. Biol Psychiatry. 2018;84:106–15.
Wang X, Xie H, Cotton AS, Duval ER, Tamburrino MB, Brickman KR, et al. Preliminary study of acute changes in emotion processing in trauma survivors with PTSD symptoms. PloS One. 2016;11:e0159065.
Stevens JS, Kim YJ, Galatzer-Levy IR, Reddy R, Ely TD, Nemeroff CB, et al. Amygdala reactivity and anterior cingulate habituation predict posttraumatic stress disorder symptom maintenance after acute civilian trauma. Biol Psychiatry. 2017;81:1023–9.
Belleau EL, Ehret LE, Hanson JL, Brasel KJ, Larson CL, deRoon-Cassini TA. Amygdala functional connectivity in the acute aftermath of trauma prospectively predicts severity of posttraumatic stress symptoms. Neurobiol Stress. 2020;12:100217.
Ben-Zion Z, Shany O, Admon R, Keynan NJ, Avisdris N, Balter SR, et al. Neural responsivity to reward versus punishment shortly after trauma predicts long-term development of posttraumatic stress symptoms. Biol Psychiatry Cogn Neurosci Neuroimag. 2022;7:150–61.
Harnett NG, Ference EW, Wood KH, Wheelock MD, Knight AJ, Knight DC. Trauma exposure acutely alters neural function during Pavlovian fear conditioning. Cortex. 2018;109:1–13.
Powers A, Hinojosa CA, Stevens JS, Harvey B, Pas P, Rothbaum BO, et al. Right inferior frontal gyrus and ventromedial prefrontal activation during response inhibition is implicated in the development of PTSD symptoms. Eur J Psychotraumatology. 2022;13:2059993.
Du MY, Liao W, Lui S, Huang XQ, Li F, Kuang WH, et al. Altered functional connectivity in the brain default-mode network of earthquake survivors persists after 2 years despite recovery from anxiety symptoms. Soc Cogn Affect Neurosci. 2015;10:1497–505.
Sullivan DR, Marx B, Chen MS, Depue BE, Hayes SM, Hayes JP. Behavioral and neural correlates of memory suppression in PTSD. J Psychiatr Res. 2019;112:30–7.
Chen HJ, Ke J, Qiu J, Xu Q, Zhong Y, Lu GM, et al. Altered whole-brain resting-state functional connectivity and brain network topology in typhoon-related post-traumatic stress disorder. Ther Adv Psychopharmacol. 2023;13:20451253231175302.
Dahlgren MK, Laifer LM, VanElzakker MB, Offringa R, Hughes KC, Staples-Bradley LK, et al. Diminished medial prefrontal cortex activation during the recollection of stressful events is an acquired characteristic of PTSD. Psychol Med. 2018;48:1128–38.
Hinojosa CA, VanElzakker MB, Hughes KC, Offringa R, Sangermano LM, Spaulding IG, et al. Exaggerated amygdala activation to ambiguous facial expressions is a familial vulnerability factor for posttraumatic stress disorder. J Psychiatr Res. 2022;156:451–9.
George GC, Keding TJ, Heyn SA, Herringa RJ. Longitudinal hippocampal circuit change differentiates persistence and remission of pediatric posttraumatic stress disorder. Depress Anxiety. 2022;39:8–18.
Manthey A, Sierk A, Brakemeier EL, Walter H, Daniels JK Does trauma-focused psychotherapy change the brain? A systematic review of neural correlates of therapeutic gains in PTSD. Eur J Psychotraumatology. 2021;12:1929025.
Malejko K, Abler B, Plener PL, Straub J. Neural correlates of psychotherapeutic treatment of post-traumatic stress disorder: a systematic literature review. Front Psychiatry. 2017;8:85.
Colvonen PJ, Glassman LH, Crocker LD, Buttner MM, Orff H, Schiehser DM, et al. Pretreatment biomarkers predicting PTSD psychotherapy outcomes: A systematic review. Neurosci Biobehav Rev. 2017;75:140–56.
Graziano RC, Vuper TC, Yetter MA, Bruce SE. Treatment outcome of posttraumatic stress disorder: a white matter tract analysis. J Anxiety Disord. 2021;81:102412.
Hinojosa CA, VanElzakker MB, Kaur N, Felicione JM, Charney ME, Bui E, et al. Pre-treatment amygdala activation and habituation predict symptom change in post-traumatic stress disorder. Front Behav Neurosci [Internet]. 2023 [cited 2023 Sep 14];17. Available from: https://www.frontiersin.org/articles/10.3389/fnbeh.2023.1198244.
Norbury A, Rutter SB, Collins AB, Costi S, Jha MK, Horn SR, et al. Neuroimaging correlates and predictors of response to repeated-dose intravenous ketamine in PTSD: preliminary evidence. Neuropsychopharmacology. 2021;46:2266–77.
Danböck SK, Duek O, Ben-Zion Z, Korem N, Amen SL, Kelmendi B, et al. Effects of a dissociative drug on fronto-limbic resting-state functional connectivity in individuals with posttraumatic stress disorder: a randomized controlled pilot study. Psychopharmacol (Berl). 2024;241:243–52.
Yuan M, Qiu C, Meng Y, Ren Z, Yuan C, Li Y, et al. Pre-treatment resting-state functional MR imaging predicts the long-term clinical outcome after short-term paroxtine treatment in post-traumatic stress disorder. Front Psychiatry [Internet]. 2018 [cited 2024 Feb 11];9. Available from: https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2018.00532.
Korgaonkar MS, Chakouch C, Breukelaar IA, Erlinger M, Felmingham KL, Forbes D, et al. Intrinsic connectomes underlying response to trauma-focused psychotherapy in post-traumatic stress disorder. Transl Psychiatry. 2020;10:1–11.
Garrett A, Cohen JA, Zack S, Carrion V, Jo B, Blader J, et al. Longitudinal changes in Brain function associated with Symptom Improvement in Youth with PTSD. J Psychiatr Res. 2019;114:161.
Zhutovsky P, Zantvoord JB, Ensink JBM, op den Kelder R, Lindauer RJL, van Wingen GA. Individual prediction of trauma-focused psychotherapy response in youth with posttraumatic stress disorder using resting-state functional connectivity. NeuroImage Clin. 2021;32:102898.
Steuwe C, Daniels JK, Frewen PA, Densmore M, Pannasch S, Beblo T, et al. Effect of direct eye contact in PTSD related to interpersonal trauma: an fMRI study of activation of an innate alarm system. Soc Cogn Affect Neurosci. 2014;9:88–97.
Cisler JM, Sigel BA, Steele JS, Smitherman S, Vanderzee K, Pemberton J, et al. Changes in functional connectivity of the amygdala during cognitive reappraisal predict symptom reduction during trauma-focused cognitive-behavioral therapy among adolescent girls with post-traumatic stress disorder. Psychol Med. 2016;46:1–11.
Levy-Gigi E, Szabó C, Kelemen O, Kéri S. Association among clinical response, hippocampal volume, and FKBP5 gene expression in individuals with posttraumatic stress disorder receiving cognitive behavioral therapy. Biol Psychiatry. 2013;74:793–800.
Bossini L, Santarnecchi E, Casolaro I, Koukouna D, Caterini C, Cecchini F, et al. Morphovolumetric changes after EMDR treatment in drug-naïve PTSD patients. Riv Psichiatr. 2017;52:24–31.
Butler O, Herr K, Willmund G, Gallinat J, Kühn S, Zimmermann P. Trauma, treatment and tetris: video gaming increases hippocampal volume in male patients with combat-related posttraumatic stress disorder. J Psychiatry Neurosci. JPN. 2020;45:279–87.
Butler O, Willmund G, Gleich T, Gallinat J, Kühn S, Zimmermann P. Hippocampal gray matter increases following multimodal psychological treatment for combat‐related post‐traumatic stress disorder. Brain Behav [Internet]. 2018 May [cited 2023 Aug 9];8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5943737/.
Kennis M, van Rooij SJH, Tromp DPM, Fox AS, Rademaker AR, Kahn RS, et al. Treatment outcome-related white matter differences in veterans with posttraumatic stress disorder. Neuropsychopharmacol Publ Am Coll Neuropsychopharmacol. 2015;40:2434–42.
Vuper TC, Philippi CL, Bruce SE. Altered resting-state functional connectivity of the default mode and central executive networks following cognitive processing therapy for PTSD. Behav Brain Res. 2021;409:113312.
Fonzo GA, Goodkind MS, Oathes DJ, Zaiko YV, Harvey M, Peng KK, et al. Amygdala and insula connectivity changes following psychotherapy for posttraumatic stress disorder: a randomized clinical trial. Biol Psychiatry. 2021;89:857–67.
Leroy A, Very E, Birmes P, Yger P, Szaffarczyk S, Lopes R, et al. Intrusive experiences in posttraumatic stress disorder: Treatment response induces changes in the directed functional connectivity of the anterior insula. NeuroImage Clin. 2022;34:102964.
Zhu X, Suarez-Jimenez B, Lazarov A, Helpman L, Papini S, Lowell A, et al. Exposure-based therapy changes amygdala and hippocampus resting-state functional connectivity in patients with posttraumatic stress disorder. Depress Anxiety. 2018;35:974–84.
Santarnecchi E, Bossini L, Vatti G, Fagiolini A, La Porta P, Di Lorenzo G, et al. Psychological and brain connectivity changes following trauma-focused CBT and EMDR treatment in single-episode PTSD patients. Front Psychol. 2019;10:129.
Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspect Psychol Sci J Assoc Psychol Sci. 2013;8:651–62.
Maron-Katz A, Zhang Y, Narayan M, Wu W, Toll RT, Naparstek S, et al. Individual patterns of abnormality in resting-state functional connectivity reveal two data-driven PTSD subgroups. Am J Psychiatry. 2020;177:244–53.
McClellan France J, Jovanovic T. Human fear neurobiology reimagined: can brain-derived biotypes predict fear-based disorders after trauma? Neurosci Biobehav Rev. 2023;144:104988.
Ahrenholtz R, Hiser J, Ross MC, Privratsky A, Sartin-Tarm A, James GA, et al. Unique neurocircuitry activation profiles during fear conditioning and extinction among women with posttraumatic stress disorder. J Psychiatr Res. 2021;141:257–66.
Stevens JS, Harnett NG, Lebois LAM, van Rooij SJH, Ely TD, Roeckner A, et al. Brain-based biotypes of psychiatric vulnerability in the acute aftermath of trauma. Am J Psychiatry. 2021;178:1037–49.
Ben-Zion Z, Spiler TR, Keynan JN, Admon R, Levy I, Liberzon I, et al. Evaluating the evidence for brain-based biotypes of psychiatric vulnerability in the acute aftermath of trauma. Am J Psychiatry. 2023;180:146–154.
Stein MB, Bomyea J. Replicating predictive cluster-based imaging biotypes after trauma: a bridge too far? Am J Psychiatry. 2023;180:114–6.
Liu Y, Hayes DN, Nobel A, Marron JS. Statistical significance of clustering for high-dimension, low-sample size data. J Am Stat Assoc. 2008;103:1281–93.
Dinga R, Schmaal L, Penninx BWJH, van Tol MJ, Veltman DJ, van Velzen L, et al. Evaluating the evidence for biotypes of depression: methodological replication and extension of. NeuroImage Clin. 2019;22:101796.
Acknowledgements
CAH is supported under an NIAAA Award, K99AA031333. GCG is supported under a NIMH T32 grant, T32MH125786. ZB-Z is supported by Yale University School of Medicine (Dr. Ifat Levy & Dr. Ilan Harpaz-Rotem). We would like to thank Drs. Sanne van Rooij and Jennifer Stevens for providing critical feedback on the manuscript, and Bona Kim, M.A., C.M.I. for creating the figures.
Author information
Authors and Affiliations
Contributions
CAH was responsible for conceptualization, data curation for all sections, project administration, visualization, validation, writing the original draft, and reviewing and editing the manuscript. GCG helped with data curation for subsections, writing the original draft, and reviewing and editing the manuscript. ZBZ helped with data curation for subsections, writing the original draft, and reviewing and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hinojosa, C.A., George, G.C. & Ben-Zion, Z. Neuroimaging of posttraumatic stress disorder in adults and youth: progress over the last decade on three leading questions of the field. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02558-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02558-w