Abstract
Background
Preventing or delaying the onset of psychosis requires identification of those at risk for developing psychosis. For predictive purposes, the prodrome – a constellation of symptoms which may occur before the onset of psychosis – has been increasingly recognized as having utility. However, it is unclear what proportion of patients experience a prodrome or how this varies based on the multiple definitions used.
Methods
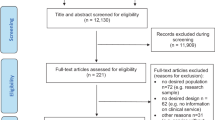
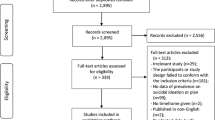
We conducted a systematic review and meta-analysis of studies of patients with psychosis with the objective of determining the proportion of patients who experienced a prodrome prior to psychosis onset. Inclusion criteria included a consistent prodrome definition and reporting the proportion of patients who experienced a prodrome. We excluded studies of only patients with a prodrome or solely substance-induced psychosis, qualitative studies without prevalence data, conference abstracts, and case reports/case series. We searched Ovid MEDLINE, Embase (Ovid), APA PsycInfo (Ovid), Web of Science Core Collection (Clarivate), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, APA PsycBooks (Ovid), ProQuest Dissertation & Thesis, on March 3, 2021. Studies were assessed for quality using the Critical Appraisal Checklist for Prevalence Studies. Narrative synthesis and proportion meta-analysis were used to estimate prodrome prevalence. I2 and predictive interval were used to assess heterogeneity. Subgroup analyses were used to probe sources of heterogeneity. (PROSPERO ID: CRD42021239797).
Results
Seventy-one articles were included, representing 13,774 patients. Studies varied significantly in terms of methodology and prodrome definition used. The random effects proportion meta-analysis estimate for prodrome prevalence was 78.3% (95% CI = 72.8–83.2); heterogeneity was high (I2 97.98% [95% CI = 97.71–98.22]); and the prediction interval was wide (95% PI = 0.411–0.936). There were no meaningful differences in prevalence between grouped prodrome definitions, and subgroup analyses failed to reveal a consistent source of heterogeneity.
Conclusions
This is the first meta-analysis on the prevalence of a prodrome prior to the onset of first episode psychosis. The majority of patients (78.3%) were found to have experienced a prodrome prior to psychosis onset. However, findings are highly heterogenous across study and no definitive source of heterogeneity was found despite extensive subgroup analyses. As most studies were retrospective in nature, recall bias likely affects these results. While the large majority of patients with psychosis experience a prodrome in some form, it is unclear if the remainder of patients experience no prodrome, or if ascertainment methods employed in the studies were not sensitive to their experiences. Given widespread investment in indicated prevention of psychosis through prospective identification and intervention during the prodrome, a resolution of this question as well as a consensus definition of the prodrome is much needed in order to effectively direct and organize services, and may be accomplished through novel, densely sampled and phenotyped prospective cohort studies that aim for representative sampling across multiple settings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
14 February 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41380-024-02481-0
References (References marked with an asterisk indicate studies included in the meta-analysis)
Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2:e141 https://doi.org/10.1371/journal.pmed.0020141.
Salazar de Pablo G, Estrade Vaz A, Cutroni M, Andlauer O, Fusar-Poli P. Establishing a clinical service to prevent psychosis: What, how and when? Systematic review. Transl Psychiatry. 2021;11:43. https://doi.org/10.1038/s41398-020-01165-x.
Wu EQ, Shi L, Birnbaum H, Hudson T, Kessler R. Annual prevalence of diagnosed schizophrenia in the USA: a claims data analysis approach. Psychol Med. 2006;36:1535–40. https://doi.org/10.1017/S0033291706008191.
Desai PR, Lawson KA, Barner JC, Rascati KL. Estimating the direct and indirect costs for community-dwelling patients with schizophrenia. J Pharm Health Serv Res. 2013;4:187–94. https://doi.org/10.1111/jphs.12027/epdf.
Kessler RC, Birnbaum H, Demler O, Falloon IR, Gagnon E, Guyer M. et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry. 2005;58:668–76. https://doi.org/10.1016/j.biopsych.2005.04.034.
Moreno-Küstner B, Martín C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PloS ONE. 2018;13:e0195687 https://doi.org/10.1371/journal.pone.0195687.
Häfner H. Prodrome, onset and early course of schizophrenia. In Murray RM, Jones PB, Susser E, van Os J, & Cannon M. editors. The epidemiology of schizophrenia. Cambridge University Press. 2003. pp. 124–47. https://doi.org/10.1002/9780470987353.ch8.
Häfner H, Löffler W, Maurer K, Hambrecht M, an der Heiden W. Depression, negative symptoms, social stagnation and social decline in the early course of schizophrenia. Acta Psychiatr Scand. 1999;100:105–18. https://doi.org/10.1111/j.1600-0447.1999.tb10831.x. *.
Gross G, Huber G, Klosterkötter J, & Linz M. Bonner Skala für die beurteilung von basissymptomen [BSABS; Bonn Scale for the Assessment of Basic Symptoms]. Berlin, Germany: Springer; 1987.
McGlashan TH, Johannessen JO. Early detection and intervention with schizophrenia: rationale. Schizophr Bull. 1996;22:201–22. https://doi.org/10.1093/schbul/22.2.201.
Cupo L, McIlwaine SV, Daneault JG, Malla AK, Iyer SN, Joober R. et al. Timing, distribution, and relationship between nonpsychotic and subthreshold psychotic symptoms prior to emergence of a first episode of psychosis. Schizophr Bull. 2021;47:604–14. https://doi.org/10.1093/schbul/sbaa183. *.
Institute of Medicine (US) Committee on prevention of mental disorders. In Mrazek PJ, & Haggerty RJ. editors. Reducing risks for mental disorders: frontiers for preventive intervention research. National Academies Press (US). 1994. https://pubmed.ncbi.nlm.nih.gov/25144015/.
Yung A, Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D. et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust NZ J Psychiatry. 2005;39:964–71. https://doi.org/10.1111/j.1440-1614.2005.01714.x.
McGlashan TH, Miller TJ, Woods SW, Hoffman RE, & Davidson L. Instrument for the assessment of prodromal symptoms and states. Early intervention in psychotic disorders, 2001. 135–9. https://link.springer.com/chapter/10.1007/978-94-010-0892-1_7.
McGorry PD, Yung AR, Phillips LJ. The “close-in” or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull. 2003;29:771–90. https://doi.org/10.1093/oxfordjournals.schbul.a007046.
Salazar de Pablo G, Radua J, Pereira J, Bonoldi I, Arienti V, Besana F. et al. Probability of transition to psychosis in individuals at clinical high risk: an updated meta-analysis. JAMA Psychiatry. 2021;78:970–8. https://doi.org/10.1001/jamapsychiatry.2021.0830.
Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L. et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220–9. https://doi.org/10.1001/archgenpsychiatry.2011.1472.
Devoe DJ, Farris MS, Townes P, Addington J. Interventions and transition in youth at risk of psychosis: a systematic review and meta-analyses. J Clin Psychiatry. 2020;81:17r12053 https://doi.org/10.4088/JCP.17r12053.
Killackey E, Yung AR. Effectiveness of early intervention in psychosis. Curr Opin Psychiatry. 2007;20:121–5. https://doi.org/10.1097/YCO.0b013e328017f67d.
Worthington MA, Cannon TD. Prediction and prevention in the clinical high-risk for psychosis paradigm: a review of the current status and recommendations for future directions of inquiry. Front Psychiatry. 2021;12:770774 https://doi.org/10.3389/fpsyt.2021.770774.
Davies C, Radua J, Cipriani A, Stahl D, Provenzani U, McGuire P. et al. Efficacy and acceptability of interventions for attenuated positive psychotic symptoms in individuals at clinical high risk of psychosis: a network meta-analysis. Front Psychiatry. 2018;9:187 https://doi.org/10.3389/fpsyt.2018.00187.
Fusar-Poli P, Davies C, Solmi M, Brondino N, De Micheli A, Kotlicka-Antczak M. et al. Preventive treatments for psychosis: umbrella review (just the evidence). Front Psychiatry. 2019;10:764 https://doi.org/10.3389/fpsyt.2019.00764.
Addington J, Liu L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA. et al. North American prodrome longitudinal study (NAPLS 2): the prodromal symptoms. J Nerv Ment Dis. 2015;203:328–35. https://doi.org/10.1097/NMD.0000000000000290. *.
Addington J, Piskulic D, Liu L, Lockwood J, Cadenhead KS, Cannon TD. et al. Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophr Res. 2017;190:90–95. https://doi.org/10.1016/j.schres.2017.03.043.
Gale C, Glue P, Gallagher S. Bayesian analysis of posttest predictive value of screening instruments for the psychosis high-risk state. JAMA Psychiatry. 2013;70:880–1. https://doi.org/10.1001/jamapsychiatry.2013.1320.
Simon AE, Ferrero FP, Merlo MCG. Prodromes of first-episode psychosis: how can we challenge neurospecificity. Compr Psychiatry. 2001;42:382–92. https://doi.org/10.1053/comp.2001.26272.
Woods SW, Powers AR,III, Taylor JH, Davidson CA, Johannesen JK, Addington J. et al. Lack of diagnostic pluripotentiality in patients at clinical high risk for psychosis: specificity of comorbidity persistence and search for pluripotential subgroups. Schizophr Bull. 2018;44:254–63. https://doi.org/10.1093/schbul/sbx138.
Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, Yung AR. Outcomes of non-transitioned cases in a sample at ultra-high risk for psychosis. Am J Psychiatry. 2015;172:249–58.
Schultze-Lutter F, Rahman J, Ruhrmann S, Michel C, Schimmelmann BG. et al. Duration of unspecific prodromal and clinical high risk states, and early help-seeking in first-admission psychosis patients. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1831–41. https://doi.org/10.1007/s00127-015-1093-3. *.
Shah JL, Crawford A, Mustafa SS, Iyer SN, Joober R. et al. Is the clinical high-risk state a valid concept? Retrospective examination in a first-episode psychosis sample. Psychiatr Serv. 2017;68:1046–52. https://doi.org/10.1176/appi.ps.201600304. *.
Brady LS, Larrauri CA.AMP SCZ Steering Committee. Accelerating Medicines Partnership® Schizophrenia (AMP® SCZ): Developing tools to enable early intervention in the psychosis high risk state. World Psychiatry. 2023;22:42–43. https://doi.org/10.1002/wps.21038.
Yung AR, Wood SJ, Malla A, Nelson B, McGorry P, Shah J. The reality of at risk mental state services: a response to recent criticisms. Psychol Med. 2021;51:212–8. https://doi.org/10.1017/S003329171900299X.
Ajnakina O, David AS, Murray RM. At risk mental state’ clinics for psychosis - an idea whose time has come - and gone!. Psychol Med. 2019;49:529–34. https://doi.org/10.1017/S0033291718003859.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160 https://doi.org/10.1136/bmj.n160.
Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E. et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med Res Methodol. 2021;21:189 https://doi.org/10.1186/s12874-021-01381-z.
Yale University. Reference Deduplicator. 2021. https://library.medicine.yale.edu/reference-deduplicator.
Covidence systematic review software. Veritas Health Innovation Melbourne, Australia. 2023. Available at www.covidence.org.
Varsamis J, Adamson JD. Early schizophrenia. Can Psychiatr Assoc J. 1971;16:487–97. https://journals.sagepub.com/doi/pdf/10.1177/070674377101600604.*.
Häfner H, Riecher A, Maurer K, Löffler W, Munk-Jørgensen P, Strömgren E. How does gender influence age at first hospitalization for schizophrenia? A transnational case register study. Psychol Med. 1989;19:903–18. https://doi.org/10.1017/S0033291700005626.
Huber G, Gross G, Schüttler R, Linz M. Longitudinal studies of schizophrenic patients. Schizophr Bull. 1980;6:592–605. https://doi.org/10.1093/schbul/6.4.592.
Ferrara M, Guloksuz S, Mathis WS, Li F, Lin IH, Syed S. et al. First help-seeking attempt before and after psychosis onset: measures of delay and aversive pathways to care. Soc Psychiatry Psychiatr Epidemiol. 2021;56:1359–69. https://doi.org/10.1007/s00127-021-02090-0. *.
Joanna Briggs Institute. (2017). Critical appraisal checklist for prevalence studies. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Prevalence_Studies2017_0.pdf.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.
Migliavaca CB, Stein C, Colpani V, Barker TH, Ziegelmann PK, Munn Z. et al. Meta-analysis of prevalence: I2 statistic and how to deal with heterogeneity. Res Synth Methods. 2022;13:363–7. https://doi.org/10.1002/jrsm.1547.
Spence JR, Stanley DJ. Prediction interval: what to expect when you’re expecting … a replication. PLoS ONE. 2016;11:e0162874 https://doi.org/10.1371/journal.pone.0162874.
Häfner H, Riecher-Rössler A, Hambrecht M, Maurer K, Meissner S, Schmidtke A. et al. IRAOS: an instrument for the assessment of onset and early course of schizophrenia. Schizophr Res. 1992;6:209–23. https://doi.org/10.1016/0920-9964(92)90004-o.
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders. 3rd ed. Arlington, VA: Author.
Borenstein M, Hedges LE, Higgins JPT, & Rothstein HR. Comprehensive meta-analysis (Version 4). [Computer software]. 2022. www.Meta-Analysis.com.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. https://doi.org/10.2307/2533446.
Tan HY, Ang YG. First-episode psychosis in the military: a comparative study of prodromal symptoms. Aust NZ J Psychiatry. 2001;35:512–9. https://doi.org/10.1046/j.1440-1614.2001.00912.x. *.
Dominguez-Martinez T, Cristobal-Narvaez P, Kwapil TR, Barrantes-Vidal N. Clinical and psychosocial characterization of at-risk mental state and recent onset psychosis patients from an Early Psychosis Program in Barcelona (Spain). Actas Espanolas de Psiquiatria. 2017;45:145–56. https://pubmed.ncbi.nlm.nih.gov/28745387/.*.
Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K. et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–5.
Häfner H, Nowotny B. Epidemiology of early-onset schizophrenia. Eur Arch Psychiatry Clin Neurosci. 1995;245:80–92. https://doi.org/10.1007/BF02190734.
Maki P, Koskela S, Murray GK, Nordstrom T, Miettunen J, Jaaskelainen E. et al. Difficulty in making contact with others and social withdrawal as early signs of psychosis in adolescents—The Northern Finland Birth Cohort 1986. Eur Psychiatry. 2014;29:345–51. https://doi.org/10.1016/j.eurpsy.2013.11.003. *.
Mustonen A, Niemela S, Nordstrom T, Murray GK, Maki P, Jaaskelainen E. et al. Adolescent cannabis use, baseline prodromal symptoms and the risk of psychosis. Br J Psychiatry. 2018;212:227–33. https://doi.org/10.1192/bjp.2017.52. *.
Jackson HJ, McGorry PD, Dudgeon P. Prodromal symptoms of schizophrenia in first-episode psychosis: prevalence and specificity. Compr Psychiatry. 1995;36:241–50. https://doi.org/10.1016/s0010-440x(95)90068-3. *.
Costello A. Mental health diagnoses during the year prior to schizophrenia, U.S. Armed Forces, 2001–10. MSMR. 2012;19:10–13. https://pubmed.ncbi.nlm.nih.gov/22452716/.*.
Woodberry KA, Serur RA, Hallinan SB, Mesholam-Gately RI, Giuliano AJ, Wojcik JD. et al. Frequency and pattern of childhood symptom onset reported by first episode schizophrenia and clinical high risk youth. Schizophr Res. 2014;158:45–51. https://doi.org/10.1016/j.schres.2014.05.017. *.
Beiser M, Erickson D, Fleming JA, Iacono WG. Establishing the onset of psychotic illness. Am J Psychiatry. 1993;150:1349–54. https://doi.org/10.1176/ajp.150.9.1349.
Compton MT, Chien VH, Leiner AS, Goulding SM, Weiss PS. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Soc Psychiatry Psychiatr Epidemiol. 2008;43:975–82. https://doi.org/10.1007/s00127-008-0397-y. *.
Ito S, Nemoto T, Tsujino N, Ohmuro N, Matsumoto K, Matsuoka H. et al. Differential impacts of duration of untreated psychosis (DUP) on cognitive function in first-episode schizophrenia according to mode of onset. Eur Psychiatry. 2015;30:995–1001. https://doi.org/10.1016/j.eurpsy.2015.08.004.
McGlashan TH. Premorbid adjustment, onset types, and prognostic scaling: still informative?. Schizophr Bull. 2008;34:801–5. https://doi.org/10.1093/schbul/sbn073.
Morgan C, Abdul-Al R, Lappin J, Jones P, Fearon P, Leese M. et al. Clinical and social determinants of duration of untreated psychosis in the ÆSOP first-episode psychosis study. Br J Psychiatry. 2006;189:446–52. https://doi.org/10.1192/bjp.bp.106.021303. *.
Kanahara N, Yoshida T, Oda Y, Yamanaka H, Moriyama T, Hayashi H. et al. Onset pattern and long-term prognosis in schizophrenia: 10-year longitudinal follow-up study. PLoS ONE. 2013;8:e67273 https://doi.org/10.1371/journal.pone.0067273. *.
Shah JL, Jones N, van Os J, McGorry PD, Gülöksüz S. Early intervention service systems for youth mental health: integrating pluripotentiality, clinical staging, and transdiagnostic lessons from early psychosis. Lancet Psychiatry. 2022;9:413–22. https://doi.org/10.1016/S2215-0366(21)00467-3.
Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rössler A, Schultze-Lutter F. et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–20. https://doi.org/10.1001/jamapsychiatry.2013.269.
Solmi, Radua M, Olivola J, Croce M, Soardo E, Salazar de Pablo L. et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27:281–95. https://doi.org/10.1038/s41380-021-01161-7.
Shah JL, Scott J, McGorry PD, Cross SPM, Keshavan MS, Nelson B. et al. Transdiagnostic clinical staging in youth mental health: a first international consensus statement. World Psychiatry. 2020;19:233–42. https://doi.org/10.1002/wps.20745.
Carrión RE, Correll CU, Auther AM, Cornblatt BA. A severity-based clinical staging model for the psychosis prodrome: Longitudinal findings from the New York Recognition and Prevention Program. Schizophr Bull. 2017;43:64–74. https://doi.org/10.1093/schbul/sbw155.
Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S. et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders?. Clin Psychol Sci. 2014;2:119–37. https://doi.org/10.1177/2167702613497473.
Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby R. et al. The hierarchical taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126:454–77. https://doi.org/10.1037/abn0000258.
Riecher-Rössler A, Butler S, Kulkarni J. Sex and gender differences in schizophrenic psychoses-a critical review. Arch Women’s Ment Health. 2018;21:627–48. https://doi.org/10.1007/s00737-018-0847-9.
Brand BA, de Boer JN, Dazzan P, Sommer IE. Towards better care for women with schizophrenia-spectrum disorders. Lancet Psychiatry. 2022;9:330–6. https://doi.org/10.1016/S2215-0366(21)00383-7.
Bunk D, Eggers C, Volberg G, Schebaum-Stein T. Dimensions of premorbid disorders in childhood-onset schizophrenia (COS). Neurol Psychiatry Brain Res. 2003;10:183–92. *.
Carter B, Wootten J, Archie S, Terry AL, Anderson KK. Sex and gender differences in symptoms of early psychosis: a systematic review and meta-analysis. Arch Women’s Ment Health. 2022;25:679–91. https://doi.org/10.1007/s00737-022-01247-3.
Ferrara M, Srihari VH. Early intervention for psychosis in the United States: tailoring services to improve care for women. Psychiatr Serv. 2021;72:5–6. https://doi.org/10.1176/appi.ps.202000205.
Srihari VH, Kane JM. Early intervention services 2.0: designing systems for the next generation of work. Biol Psychiat. 2020;88:291–3.
Shah JL, Allen NB, Avenevoli S, Correll CU, Fisher HL, Hickie IB, et al. A developmentally informed approach to characterizing, staging, and intervening in youth mental health problems. From the population to the clinic. In Uhlhaas PJ, & Wood SJ, editors. Youth mental health: a paradigm for prevention and early intervention. Cambridge, MA: The MIT Press. 2020.
Benrimoh D, Fisher V, Mourgues C, Sheldon AD, Smith R, & Powers AR. Barriers and solutions to the adoption of clinical tools for computational psychiatry. 2022. https://doi.org/10.48550/arXiv.2301.04570.
August SM, Kiwanuka JN, McMahon RP, Gold JM. The MATRICS consensus cognitive battery (MCCB): clinical and cognitive correlates. Schizophrenia Res. 2012;134:76–82. https://doi.org/10.1016/j.schres.2011.10.015.
Powers AR, Mathys C, Corlett PR. Pavlovian conditioning-induced hallucinations result from overweighting of perceptual priors. Science. 2017;357:596–600. https://doi.org/10.1126/science.aan3458.
Teufel C, Subramaniam N, Dobler V, Perez J, Finnemann J, Mehta PR. et al. Shift toward prior knowledge confers a perceptual advantage in early psychosis and psychosis-prone healthy individuals. Proc Natl Acad Sci USA. 2015;112:13401–6. https://doi.org/10.1073/pnas.1503916112.
Kafadar E, Fisher VL, Quagan B, Hammer A, Jaeger H, Mourgues C. et al. Conditioned hallucinations and prior overweighting are state-sensitive markers of hallucination susceptibility. Biol Psychiatry. 2022;92:772–80. https://doi.org/10.1016/j.biopsych.2022.05.007.
Vercammen A, Aleman A. Semantic expectations can induce false perceptions in hallucination-prone individuals. Schizophr Bull. 2010;36:151–6. https://doi.org/10.1093/schbul/sbn063.
Huckvale K, Venkatesh S, Christensen H. Toward clinical digital phenotyping: a timely opportunity to consider purpose, quality, and safety. NPJ Digital Med. 2019;2:1–11. https://doi.org/10.1038/s41746-019-0166-1.
Trovão N, Prata J, VonDoellinger O, Santos S, Barbosa M, Coelho R. Peripheral biomarkers for first-episode psychosis-opportunities from the neuroinflammatory hypothesis of schizophrenia. Psychiatry Investig. 2019;16:177–84. https://doi.org/10.30773/pi.2018.12.19.1.
Veronese M, Santangelo B, Jauhar S, D’Ambrosio E, Demjaha A, Salimbeni H. et al. A potential biomarker for treatment stratification in psychosis: evaluation of an [18F] FDOPA PET imaging approach. Neuropsychopharmacol. 2021;46:1122–32. https://doi.org/10.1038/s41386-020-00866-7.
Fernandes BS, Karmakar C, Tamouza R, Tran T, Yearwood J, Hamdani N, et al. Precision psychiatry with immunological and cognitive biomarkers: a multi-domain prediction for the diagnosis of bipolar disorder or schizophrenia using machine learning. Transl Psychiatry. 2020;10:162 https://doi.org/10.1038/s41398-020-0836-4.
Mirzakhanian H, Singh F, Cadenhead KS. Biomarkers in psychosis: an approach to early identification and individualized treatment. Biomark Med. 2014;8:51–57. https://doi.org/10.2217/bmm.13.134.
Nieman DH, McGorry PD. Detection and treatment of at-risk mental state for developing a first psychosis: making up the balance. Lancet Psychiatry. 2015;2:825–34. https://doi.org/10.1016/S2215-0366(15)00221-7.
Keshavan MS, DeLisi LE, Seidman LJ. Early and broadly defined psychosis risk mental states. Schizophr Res. 2011;126:1–10. https://doi.org/10.1016/j.schres.2010.10.006.
Sandeep M. Characterisation of the prodrome to a first episode of psychotic mania: a retrospective study. 2012. (1815532270). 10153933, 178. *.
Yung AR, McGorry PD. The initial prodrome in psychosis: descriptive and qualitative aspects. Aust NZ J Psychiatry. 1996;30:587–99. https://doi.org/10.3109/00048679609062654. *.
Yıldızhan E, Türkcan A, İnan S, Erenkuş Z, Yalçın Ö, Erdoğan A. İlk Psikoz Atağı: Belirtiler, Tedavi Başlangıcı ve Klinik Yanıt İlişkisi [First episode psychosis: relationship of symptoms, initial treatment and clinical response]. Turk Psikiyatr Derg. 2015;26:77–86. https://pubmed.ncbi.nlm.nih.gov/26111283/.*.
Sullivan HS. The relation of onset to outcome in schizophrenia. Schizophrenia (Dementia Praecox). 1932. 111–8. *.
Skokou M, Katrivanou A, Andriopoulos I, Gourzis P. Sintomatología de las fases activa y prodrómica de la esquizofrenia paranoide de inicio en el joven y de inicio tardío [Active and prodromal phase symptomatology of young-onset and late-onset paranoid schizophrenia]. Rev de Psiquiatria y Salud Ment. 2012;5:150–9. https://doi.org/10.1016/j.rpsm.2012.03.002. *.
Shioiri T, Shinada K, Kuwabara H, Someya T. Early prodromal symptoms and diagnoses before first psychotic episode in 219 inpatients with schizophrenia. Psychiatry Clin Neurosci. 2007;61:348–54. https://doi.org/10.1111/j.1440-1819.2007.01685.x. *.
Schothorst PF, Emck C, van Engeland H. Characteristics of early psychosis. Compr Psychiatry. 2006;47:438–42. https://doi.org/10.1016/j.comppsych.2006.03.003. *.
Stepniak B, Papiol S, Hammer C, Ramin A, Everts S, Hennig L. et al. Accumulated environmental risk determining age at schizophrenia onset: a deep phenotyping-based study. Lancet Psychiatry. 2014;1:444–53. https://doi.org/10.1016/S2215-0366(14)70379-7. *.
Salvatore P, Khalsa HM, Hennen J, Tohen M, Yurgelun-Todd D, Casolari F. et al. Psychopathology factors in first-episode affective and non-affective psychotic disorders. J Psychiatr Res. 2007;41:724–36. https://doi.org/10.1016/j.jpsychires.2006.04.008. *.
Russell AT. The clinical presentation of childhood-onset schizophrenia. Schizophr Bull. 1994;20:631–46. https://doi.org/10.1093/schbul/20.4.631. *.
Röpcke B, Eggers C. Early-onset schizophrenia: a 15-year follow-up. Eur Child Adolesc Psychiatry. 2005;14:341–50. https://doi.org/10.1007/s00787-005-0483-6. *.
Renwick L, Lyne J, Donoghue BO, Owens L, Doyle R, Hill M. et al. Prodromal symptoms and remission following first episode psychosis. Schizophr Res. 2015;168:30–36. https://doi.org/10.1016/j.schres.2015.07.001. *.
Perkins DO, Leserman J, Jarskog LF, Graham K, Kazmer J. et al. Characterizing and dating the onset of symptoms in psychotic illness: the symptom onset in schizophrenia (SOS) inventory. Schizophr Res. 2000;44:1–10. https://doi.org/10.1016/s0920-9964(99)00161-9. *.
Rabe-Jabllonska J, Kotlicka-Antczak M, Gmitrowicz A. Clinical picture and duration of prodromal period of schizophrenia in adolescents. Arch Psychiatry Psychother. 2000;2:31–38. *.
Naqvi HA, Hussain S, Islam M, Huma S. Early psychosis symptoms. J Coll Physicians Surg Pak. 2014;24:198–202. https://www.jcpsp.pk/archive/2014/Mar2014/13.pdf.*.
Møller P, Husby R. The initial prodrome in schizophrenia: searching for naturalistic core dimensions of experience and behavior. Schizophr Bull. 2000;26:217–32. https://doi.org/10.1093/oxfordjournals.schbul.a033442. *.
Meng H, Schimmelmann BG, Koch E, Bailey B, Parzer P, Gunter M. et al. Basic symptoms in the general population and in psychotic and non-psychotic psychiatric adolescents. Schizophr Res. 2009;111:32–38. https://doi.org/10.1016/j.schres.2009.03.001. *.
Kohn D, Niedersteberg A, Wieneke A, Bechdolf A, Pukrop R, Ruhrmann S. et al. Early course of illness in first episode schizophrenia with long duration of untreated illness—a comparative study. Fortschr Der Neurol Psychiatr. 2004;72:88–92. https://doi.org/10.1055/s-2003-812509. *.
Kim Y, Lee JY, Yong SK, Jung HY, Lee KY. Reliability of the Korean Nottingham Onset Schedule (K-NOS) in Korean first-episode psychosis patients. Clin Psychopharmacol Neurosci. 2009;7:51–56. https://www.cpn.or.kr/journal/view.html?uid=69&vmd=Full.*.
Jackson HJ, McGorry PD, Dakis J, Harrigan S, Henry L, Mihalopoulos C. The inter-rater and test–retest reliabilities of prodromal symptoms in first-episode psychosis. Aust NZ J Psychiatry. 1996;30:498–504. https://doi.org/10.3109/00048679609065023. *.
Iida J, Iwasaka H, Hirao F, Hashino K, Matsumura K, Tahara K. et al. Clinical features of childhood-onset schizophrenia with obsessive-compulsive symptoms during the prodromal phase. Psychiatry Clin Neurosci. 1995;49:201–7. https://doi.org/10.1111/j.1440-1819.1995.tb01885.x. *.
Huber G, Gross G, Schüttler R. A long-term follow-up study of schizophrenia: psychiatric course of illness and prognosis. Acta Psychiatr Scand. 1975;52:49–57. https://doi.org/10.1111/j.1600-0447.1975.tb00022.x. *.
Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase in schizophrenia. Schizophr Bull. 2002;28:415–29. https://doi.org/10.1093/oxfordjournals.schbul.a006950. *.
Gottlieb BS. Prognosis of hebephrenia; a study of onset and clinical manifestations. Psychiatr Q. 1941;15:54–63. https://doi.org/10.1007/BF01613954. *.
Creel SM. Prodromal psychosocial behaviors in soldiers with schizophrenic and schizophreniform disorder. Mil Med. 1988;153:146–50. https://doi.org/10.1093/milmed/153.3.146. *.
Coryell W, Zimmerman M. Diagnosis and outcome in schizo-affective depression: a replication. J Affect Disord. 1988;15:21–27. https://doi.org/10.1016/0165-327(88)90005-5. *.
Conus P, Cotton S, Schimmelmann BG, McGorry PD, Lambert M. The first-episode psychosis outcome study: premorbid and baseline characteristics of an epidemiological cohort of 661 first-episode psychosis patients. Early Interv Psychiatry. 2007;1:191–200. https://doi.org/10.1111/j.1751-7893.2007.00026.x. *.
Chen Y, Farooq S, Edwards J, Chew-Graham CA, Shiers D, Frisher M. et al. Patterns of symptoms before a diagnosis of first episode psychosis: a latent class analysis of UK primary care electronic health records. BMC Med. 2019;17:227 https://doi.org/10.1186/s12916-019-1462-y. *.
Chen EYH, Dunn ELW, Miao M, Yeung WS, Wong CK, Chan WF. et al. The impact of family experience on the duration of untreated psychosis (DUP) in Hong Kong. Soc Psychiatry Psychiatr Epidemiol. 2005;40:350–6. https://doi.org/10.1007/s00127-005-0908-z. *.
Day R, Nielsen JA, Korten A, Ernberg G, Dube KC, Gebhart J. et al. Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization. Cult Med Psychiatry. 1987;11:123–205. https://doi.org/10.1007/BF00122563. *.
Bensi M, Armando M, Censi V, Aiello D, Fortes Lindau J, Cavaggioni G. et al. Segni e sintomi prodromici all’esordio psicotico. Uno studio sulla Duration of Untreated Illness (DUI) in un campione di pazienti con diagnosi di psicosi non affettiva [Early signs and symptoms before the psychotic onset. A study on the Duration of Untreated Illness (DUI) in a sample of patients with diagnosis of “non-affective psychotic disorders”]. La Clinica Terapeutica. 2011;162:11–18. https://pubmed.ncbi.nlm.nih.gov/21448540/. *.
Bechdolf A, Halve S, Schultze-Lutter F, & Klosterkötter J. Selbst wahrnehmbare Vulnerabilität, Prodromalsymptome und Bewältigungsreaktionen vor schizophrenen und affektiven Episoden [Self-experienced vulnerability, prodromicsymptoms and coping strategies before schizophrenic and affective episodes]. Fortschr Neurol Psychiatr. 1998;66:378–86. https://doi.org/10.1055/s2007-995275.
Addington J, van Mastrigt S, Hutchinson J, Addington D. Pathways to care: help seeking behaviour in first episode psychosis. Acta Psychiatr Scand. 2002;106:358–64. https://doi.org/10.1034/j.1600-0447.2002.02004.x.
Barajas A, Pelaez T, Gonzalez O, Usall J, Iniesta R, Arteaga M. et al. Predictive capacity of prodromal symptoms in first-episode psychosis of recent onset. Early Intervent Psychiatry. 2019;13:414–24. https://doi.org/10.1111/eip.12498. *.
Hafner H. Onset and early course as determinants of the further course of schizophrenia. Acta Psychiatr Scand Suppl. 2000;407:44–48. https://pubmed.ncbi.nlm.nih.gov/11261639/.*.
Compton MT, Esterberg ML, Druss BG, Walker EF, Kaslow NJ. A descriptive study of pathways to care among hospitalized urban African American first-episode schizophrenia-spectrum patients. Soc Psychiatry Psychiatr Epidemiol. 2006;41:566–73. https://doi.org/10.1007/s00127-006-0065-z. *.
Compton MT, Broussard B, Ramsay CE, Stewart T. Pre-illness cannabis use and the early course of nonaffective psychotic disorders: associations with premorbid functioning, the prodrome, and mode of onset of psychosis. Schizophr Res. 2011;126:71–76. https://doi.org/10.1016/j.schres.2010.10.005. *.
Eggers C, Bunk D. Frühentwicklung kindlicher schizophrenien [Early development of childhood-onset schizophrenia]. Fortschr der Neurol Psychiatr. 2009;77:558–67. https://doi.org/10.1055/s-0028-1109737. *.
Guloksuz S, Pries LK, Ten Have M, de Graaf R, van Dorsselaer S, Klingenberg B. et al. Association of preceding psychosis risk states and non-psychotic mental disorders with incidence of clinical psychosis in the general population: a prospective study in the NEMESIS-2 cohort. World Psychiatry. 2020;19:199–205. https://doi.org/10.1002/wps.20755. *.
Schultze-Lutter F, Ruhrmann S, Berning J, Maier W, Klosterkotter J. Basic symptoms and ultrahigh risk criteria: symptom development in the initial prodromal state. Schizophr Bull. 2010;36:182–91. https://doi.org/10.1093/schbul/sbn072. *.
Emck C, Schothorst PF, Van Engeland H. Psychosen bij jeugdigen [Early onset psychosis]. Tijdschr Voor Psychiatr. 2001;43:757–65. https://research.vu.nl/en/publications/psychosen-bij-jeugdigen.*.
Pierre K. An Exploration of the harbingers that differentiate the schizophrenia prodrome from a “Bad Patch”. 2010. https://escholarship.mcgill.ca/concern/theses/x346d463j. *.
Iyer SN, Boekestyn L, Cassidy CM, King S, Joober R, Malla AK. Signs and symptoms in the pre-psychotic phase: description and implications for diagnostic trajectories. Psychol Med. 2008;38:1147–56. https://doi.org/10.1017/S0033291708003152. *.
Hafner H. When, how and with what does schizophrenia begin?. J Brasileiro de Psiquiatria. 1996;45:7–21. *.
Maurer K, Konnecke R, Loffler W, Hafner H. Some new results from the ABC-study on early course and early recognition. Neurol Psychiatry Brain Res. 1998;6:9–18. *.
Häfner H, Nowotny B, Löffler W, an der Heiden W, Maurer K. When and how does schizophrenia produce social deficits?. Eur Arch Psychiatry Clin Neurosci. 1995;246:17–28. https://doi.org/10.1007/BF02191811. *.
Häfner H, Maurer K, Löffler W, an der Heiden W, Stein A, Könnecke R, et al. Onset and prodromal phase as determinants of the course. Search for the causes of schizophrenia: Vol. IV Balance of the century. Steinkopff. 1999. pp. 35–58. https://doi.org/10.1007/978-3-642-47076-9_3l. *.
Hafner H. Onset and course of the first schizophrenic episode. Kaohsiung J Med Sci. 1998;14:413–31. https://pubmed.ncbi.nlm.nih.gov/9739575/.*.
Compton MT, Kelley ME, Ramsay CE, Pringle M, Goulding SM, Esterberg ML. et al. Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. Am J Psychiatry. 2009;166:1251–7. https://doi.org/10.1176/appi.ajp.2009.09030311. *.
Compton MT, Goulding SM, Walker EF. Characteristics of the retrospectively assessed prodromal period in hospitalized patients with first-episode nonaffective psychosis: findings from a socially disadvantaged, low-income, predominantly African American population. J Clin Psychiatry. 2010;71:1279–85. https://doi.org/10.4088/JCP.08m04678yel. *.
Eggers C, Bunk D. The long-term course of childhood-onset schizophrenia: a 42-year followup. Schizophr Bull. 1997;23:105–17. https://doi.org/10.1093/schbul/23.1.105. *.
Eggers C, Bunk D, Krause D. Schizophrenia with onset before the age of eleven: clinical characteristics of onset and course. J Autism Dev Disord. 2000;30:29–38. https://doi.org/10.1023/a:1005408010797. *.
Eggers C. The course of infantile and prepubertal schizophrenia. Monographien Aus Dem Gesamtgeb Der Psychiatr. 1973;9:250 https://doi.org/10.1007/978-3-662-13371-2. *.
Acknowledgements
We would like to extend our sincere thanks to the library sciences department at Yale University for their significant contributions to the process of finding, requesting, and making available articles for this review. We would also like to thank all those authors who made a significant effort to provide us with data missing from their articles in support of this review. These included: Dr. Jackson, Dr. Riecher-Rossler, Dr. Yildizhan, Dr. Pelizza, Dr. Ehrenreich, Dr. Barrantes, Dr. Velthorst, Dr. Salvatore, Dr. Dazzan, Dr. Conus, Dr. McGorry, Dr. Skokou, Dr. Woodberry, Dr. Van Os, Dr. Sullivan, Dr. Mustonen, and Dr. Renwick.
Funding
No funding was received in connection to this review. D.B. is a shareholder, founder, and employee of Aifred Health, a digital mental health company which was not involved in any way with this review and whose work is not relevant to the aims of this review. D.B. did not receive funding from Aifred Health in connection to this review.
Author information
Authors and Affiliations
Contributions
DB contributed to study conceptualization and the study protocol, data collection, conducted the data analysis, and led manuscript writing and revisions. VD, ACW, and PP contributed to study conceptualization and the study protocol, data collection, manuscript writing. MCF contributed to study conceptualization, prepared the search strategy, and contributed to manuscript writing. MF, ARP III, SWW, SG, ARY and VS contributed to study conceptualization, advised on analyses, and contributed to manuscript writing and revision. JS provided supervision, contributed to study conceptualization and the study protocol, advised on the data analysis, and contributed to manuscript writing and revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the author’s name Sinan Guloksuz was incorrectly written as Sinahin Guloksuz.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benrimoh, D., Dlugunovych, V., Wright, A.C. et al. On the proportion of patients who experience a prodrome prior to psychosis onset: A systematic review and meta-analysis. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02415-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02415-w