Abstract
Antipsychotic drugs differ in their propensity to cause extrapyramidal side-effects (EPS), but their dose-effects are unclear. Therefore, we conducted a systematic review and dose-response meta-analysis. We searched multiple electronic databases up to 20.02.2023 for fixed-dose studies investigating 16 second-generation antipsychotics and haloperidol (all formulations and administration routes) in adults with acute exacerbations of schizophrenia. The primary outcome was the number of participants receiving antiparkinsonian medication, and if not available, the number of participants with extrapyramidal side-effects (EPS) and the mean scores of EPS rating scales were used as proxies. The effect-size was odds ratio (ORs) compared with placebo. One-stage random-effects dose-response meta-analyses with restricted cubic splines were conducted to estimate the dose-response curves. We also examined the relationship between dopamine D2 receptor (D2R) occupancy and ORs by estimating occupancies from administrated doses. We included data from 110 studies with 382 dose arms (37193 participants). Most studies were short-term with median duration of 6 weeks (range 3–26 weeks). Almost all antipsychotics were associated with dose-dependent EPS with varied degrees and the maximum ORs ranged from OR = 1.57 95%CI [0.97, 2.56] for aripiprazole to OR = 7.56 95%CI [3.16, 18.08] for haloperidol at 30 mg/d. Exceptions were quetiapine and sertindole with negligible risks across all doses. There was very low quality of findings for cariprazine, iloperidone, and zotepine, and no data for clozapine. The D2R occupancy curves showed that the risk increased substantially when D2R occupancy exceeded 75–85%, except for D2R partial agonists that had smaller ORs albeit high D2R occupancies. In conclusion, we found that the risk of EPS increases with rising doses and differs substantially in magnitude among antipsychotics, yet exceptions were quetiapine and sertindole with negligible risks. Our data provided additional insights into the current D2R therapeutic window for EPS.
Similar content being viewed by others
Introduction
Extrapyramidal side-effects (EPS) or drug-induced movement disorders, such as parkinsonism, dystonia, akathisia, and tardive dyskinesia [1], are among the most common side-effects of antipsychotic medications that can be present in up to a third of people with schizophrenia [2]. They can be stigmatizing and unpleasant, leading to nonadherence to treatment and the subsequent negative impacts [3]. Moreover, they often require the use of adjunctive medications, such as anticholinergic medications, which could further increase the side-effect burden, e.g., cognitive impairment and constipation [4]. Therefore, proper information about the risk of EPS associated with antipsychotic treatment is necessary.
The principal pathogenetic mechanism of antipsychotic-induced EPS is the blockade of the dopamine D2 receptor (D2R) signalling in the nigrostriatal pathway [5]. All current antipsychotics bind to the D2R, albeit with different affinities and receptor-binding profiles [6,7,8]. According to the receptor occupancy theory, the D2R occupancy of an antipsychotic depends on its affinity to the D2R and the plasma concentration [9], which is associated with the administrated dose [10]. Antipsychotic drugs typically reach maximum efficacy at doses corresponding to approximately 80% D2R occupancy, with higher doses beyond this threshold increasing the risk of EPS [8, 11,12,13,14,15,16,17]. However, the exact mechanism is more complex, and other receptors, including serotonin 5-HT1A, 5-HT2A, 5-HT2c and muscarinic M1 receptors, also play a role [8, 18,19,20]. Therefore, the risk of EPS varies among antipsychotics, with newer or “second-generation” antipsychotics generally having a lower risk [21].
While EPS may be dose-dependent, the dose-response curves remain unclear and can differ across medications [22]. Additionally, while the above-mentioned D2R therapeutic window has been documented in molecular imaging studies [8, 12,13,14], it has not yet been comprehensively evaluated in systematic reviews of clinical trials. To further elucidate these issues, we conducted a comprehensive systematic review and dose-response meta-analysis on antipsychotic-induced EPS.
Methods and materials
We followed the PRISMA statement (eAppendix 1) [23], pre-registered the protocol (PROSPERO-ID: CRD42020181467, data extraction for this analysis had started before submission of the protocol), and noted any deviations (eAppendix 2).
Eligibility criteria
Participants
We included adults with acute exacerbations of schizophrenia spectrum disorders, i.e., schizophrenia, schizoaffective and schizophreniform disorder, without other restrictions in terms of age, sex, ethnicity, setting, previous response to treatment and diagnostic criteria. We analysed separately studies focusing on predominant negative symptoms, first-episode, and elderly, given that these patients may require lower doses and could be more vulnerable to side-effects [24]. We excluded studies on stable patients (relapse prevention studies) due to methodological and clinical heterogeneity, e.g., pre-exposure to antipsychotics in the stabilization phase.
Interventions
We included studies evaluating monotherapy with 16 second-generation antipsychotics, i.e., amisulpride, aripiprazole, asenapine, brexpiprazole, cariprazine, clozapine, iloperidone, lumateperone, lurasidone, olanzapine, quetiapine, paliperidone, risperidone, sertindole, ziprasidone, and zotepine, the first-generation antipsychotic haloperidol (commonly used as an active comparator), and placebo. Studies allocating participants to fixed-dosing schedules or narrow fixed dose ranges were eligible, and flexible-dosing schedules were excluded. There was no restriction in terms of formulations (e.g., oral, long-acting intramuscular injection, transdermal, and immediate- and extending-release). Different formulations were combined in the primary analysis by converting doses to daily oral equivalents similar to our previous analysis [25]. Nevertheless, they were also analysed separately in a sensitivity analysis.
Study design
We included open and blinded randomized-controlled trials (RCTs) with a minimum study duration of 3 weeks [26] comparing fixed-doses of the above-mentioned antipsychotics or placebo in people with acute exacerbation of schizophrenia. Nevertheless, we excluded studies that investigated only head-to-head comparisons between two different antipsychotics, as well as relapse-prevention studies. We also excluded studies with a high risk of bias in terms of randomization [27]. In case of crossover trials, we used the first phase in order to avoid carry-over effects [28]. Cluster-randomized trials were excluded because of unit-of-analysis problems [29].
Search strategy
We searched up to 06.03.2022 the study-based trial register of the Cochrane Schizophrenia Group [30], which included regular searches in multiple electronic databases and hand searches. We also conducted update searches up to 20.02.2023 in PubMed and CENTRAL. Moreover, we inspected reference lists of previous reviews on relevant topics (search strings and details provided in eAppendix 3).
Outcomes
We considered a priori three outcomes: (1) mean change scores of validated scales measuring EPS, e.g., preferably with the Simpson and Angus Scale (SAS) [31], (2) number of participants that received at least once antiparkinsonian medication, and (3) number of participants with at least one EPS.
The continuous data on scale scores were heavily skewed, and thus, we did not use them as the primary outcome. Moreover, in order to allow a more comprehensive synthesis with increased power, we defined our primary outcome post-hoc as dichotomous using data from the number of patients receiving antiparkinsonian medication, and if not available, data from the number of patients with at least one EPS and mean change scores of rating scales (see also below “Data synthesis”). Nevertheless, the findings for the three aforementioned outcomes were also reported separately as sensitivity analyses.
Data extraction and risk of bias assessment
Two of the reviewers (HW, SS, NN, DW, SL) independently selected studies, extracted data into a Microsoft Access database [32], and evaluated the risk of bias of individual studies using the Cochrane Risk of Bias tool 1 [27]. Discrepancies were solved by consensus, and study authors were contacted for further clarifications.
For continuous outcomes, we preferred change over endpoint data, and results accounting for missing outcome data over completer or per-protocol, giving preference to mixed-models of repeated measurement (MMRM) and multiple imputation over last-observation carried forward (LOCF). In case of missing standard deviations (SDs), they were calculated from standard errors, other test statistics, or imputed from the SDs of other studies [27, 33]. If only completer analyses were presented for dichotomous outcomes, we assumed that patients lost to follow-up did not have the outcome.
Data synthesis
The effect sizes for continuous outcomes were standardized mean differences (SMDs) because different EPS scales were expected, and for dichotomous were odds ratios (ORs) because of their preferred mathematical properties [34, 35]. We also transformed SMDs to ORs using the Hasselblad and Hedges’ method [36,37,38], in order to allow the combination of continuous and dichotomous data for the primary outcome, as well as comparability of the findings in a sensitivity analysis. Placebo or 0 mg was used as reference in the calculation of effect-sizes. ORs were interpreted as small (OR = 1.52), medium (OR = 2.74) and large (OR = 4.72), assuming a risk of 5% in the placebo group (eAppendix 2) [39].
We estimated dose-response curves for each antipsychotic separately with a one-stage random-effects dose-response meta-analysis in a frequentist framework [40]. We used restricted cubic splines with three knots, which were set at the 25th, 50th and 75th percentiles of the doses, except for asenapine, at 10th, 50th and 90th percentiles, because the former percentiles could not form three knot points. We estimated the maximum risk for EPS and the corresponding dose. Dose-response curves were evaluated descriptively, as well as with a Wald test and the coefficients of the model [41]. Heterogeneity was quantified with the variance partition coefficient (VPC), which is a multivariate extension of the I2 statistic [40].
Patient subgroups were analysed separately and the robustness of the results were evaluated in predefined sensitivity analyses: (i) excluding non-dose-finding studies, i.e., single dose arm versus placebo, (ii) excluding studies with treatment-resistant patients, (iii) excluding open studies, (iv) analysing different formulations separately, (v) using knot points at 10th, 50th and 95th percentiles, and (vi) analysing separately the three outcome measures of EPS.
Furthermore, we post-hoc explored the relationship between D2R occupancy and the risk of EPS (eAppendix 2). We converted the dose-response curves of individual antipsychotics to occupancy-response curves by estimating the median D2R occupancy from the daily dose using Michaelis-Menten models derived from the previous meta-analysis of Lako et al 2013 (see eAppendix 2 for the formulas and their limitations) [11]. The meta-analysis of Lako et al 2013 provided formulas for eight antipsychotics, i.e., amisulpride, aripiprazole, clozapine, haloperidol, olanzapine, quetiapine, risperidone, and ziprasidone [11]. Moreover, we conducted a dose-response meta-analysis by combining the estimated D2R occupancies of the above-mentioned antipsychotics, except for aripiprazole that is a D2R partial agonist [42]. In this analysis, we set the knot points at the 25th, 50th and 75th percentiles of D2R occupancies >50%, given that we expected changes at this part of the curve [43].
We evaluated small-study effects and the potentially associated publication bias when there were at least 10 studies available with funnel plots of the pairwise comparison between an antipsychotic (any dose) versus placebo, and with dose-response meta-regression for sample size (eAppendix 2).
Quality of the evidence was evaluated with the GRADE approach [44], which was adapted to a dose-response meta-analysis and considering the domains of risk of bias, reporting bias, indirectness, inconsistency, and imprecision (eAppendix 9). The results of the assessments were summarized into four categories, i.e., high, moderate, low and very low confidence of evidence.
Data analysis was conducted with meta v5.1-1 [45] and dosresmeta v2.0.1 [41] in R statistical software v4.0.3 [46].
Results
We included 110 studies with 382 dose arms and 37193 participants in this meta-analysis. The PRISMA diagram of the search is provided in Fig. 1. The table of study characteristics is presented in eAppendix 4. There were no eligible studies for the elderly subgroup, and sparse data on the subgroups of predominant negative symptoms (amisulpride and olanzapine) and first-episode (risperidone). We had data for all antipsychotics of interest, except for clozapine. The median study duration was 6 weeks (3–26 weeks). The participants had a mean age of 38.8 years old and around a third of them were female. For overall risk of bias of included studies, 66 studies were rated as low, 37 moderate, and 7 high. Summary of risk of bias assessments is provided (eAppendix 5).
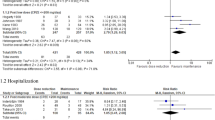
Dose-response curves of antipsychotic-induced extrapyramidal side-effects
The findings for each antipsychotic for the general population of chronically-ill patients with an acute exacerbation, and when available for other patient subgroups, are presented below and in Fig. 2. Detailed descriptions of heterogeneity assessment, sensitivity analyses, and small-study effects are presented in eAppendices 6–8. We also appraised quality of evidence for each antipsychotic drug separately using GRADE approach and reported the assessments in the results (detailed assessments are provided in eAppendix 9).
This figure shows the dose-response curves of 16 individual antipsychotics for extrapyramidal side-effects (EPS) in different subgroups of patients with schizophrenia. The X-axis displays the daily antipsychotic dose (mg/d), while the Y-axis displays the odds ratios (ORs) for the risk of EPS associated with a specific antipsychotic dose compared to non-exposure (i.e., placebo or 0 mg/d). The colored areas display the 95% confidence intervals (95%CI). The color key displays the confidence in the evidence according to the GRADE approach (green=high, blue=moderate, yellow=low, red=very low). a: different formulations were pooled; b: knot locations at the 10th, 50th, and 90th percentiles were used; n. studies=number of studies; n. arms=number of arms; N=number of participants; OR odds ratio; EPS extrapyramidal side-effects.
Amisulpride
There was low confidence of evidence of an increasing monotonic curve, i.e., higher risk of EPS with increasing doses, reaching large odds ratios (ORs) up to 5.79 95%CI [2.06, 16.25] at 1200 mg/d (number of studies n = 1, number of participants N = 255, number of arms k = 4; VPC not estimable; p value of the Wald test = 0.004). Although the single available trial did not include a placebo arm [47], ORs were calculated using 0 mg/d as the reference point. It should be noted that this is an extrapolation, which is prone to bias.
In patients with predominant negative symptoms, lower amisulpride doses up to 300 mg/d, which are sufficient for this indication [48], were investigated. There was very low confidence of evidence of a relatively flat curve with small point estimates up to a maximum of OR 1.41 [0.55, 3.60] at 80.9 mg/d, yet 95%CI could not exclude the null effect and medium-to-large ORs (n = 4, N = 591, k = 10; median VPC = 0%, p value = 0.75).
Aripiprazole
There was low confidence of evidence of a linear curve reaching small ORs up to 1.57 [0.97, 2.56] at 30 mg/d, but 95%CI did not exclude the null effect (n = 9, N = 2259, k = 26; median VPC = 52%; p value = 0.17).
Asenapine
There was moderate confidence of evidence of a linear curve reaching small-to-medium ORs up to 2.14 [1.27, 3.62] at 20 mg/d (n = 6, N = 2242, k = 17, median VPC = 24.2%; p value = 0.01).
Brexpiprazole
There was high confidence of evidence of an almost linear curve with small ORs reaching up to 1.68 [1.21, 2.34] at 5 mg/d (n = 4, N = 2178, k = 17; median VPC = 0%, p value = 0.006).
Cariprazine
There was very low confidence of evidence of a linear curve reaching up to a medium OR 3.52 [1.56, 7.96] at 9 mg/d (n = 5, N = 1918, k = 17; median VPC = 45.6%; p value = 0.01).
Clozapine
We found no usable data for clozapine.
Haloperidol
There was moderate confidence of evidence of an increasing monotonic relationship with large ORs after 10 mg/d up to a maximum OR 7.56 [3.16, 18.08] at 30 mg/day (n = 17, N = 2623, k = 38; median VPC = 48.2%, p value < 0.001).
Iloperidone
There was very low confidence of evidence of a relatively flat curve reaching small point estimates up to OR 1.55 [0.46, 5.26] at 24 mg/d, but 95%CI were very wide and could not exclude the null and larger effects (n = 2, N = 952, k = 6; median VPC = 0%, p value = 0.65).
Lumateperone
There was low confidence of evidence of a J-shaped relationship with the risk being increased above >60 mg/d reaching large point estimates up to OR 5.52 [0.38, 80.46] at 120 mg/day. However, 95%CI were very wide and could not exclude the null and larger effects (n = 3, N = 1225, k = 9; median VPC = 7.8%, p value = 0.46).
Lurasidone
There was low confidence of evidence of an increasing linear relationship with medium-to-large ORs for doses up to 160 mg/d, and large ORs for higher doses up to a maximum of 6.93 [3.23, 14.84] at 240 mg/d (n = 11, N = 3649, k = 32; median VPC = 13.6%, p value < 0.001). Only one study [49] investigated lurasidone dose above 160 mg/day, i.e., 240 mg/d, in treatment-resistant patients, which explained the wider 95%CI at these doses. Small-study effects were indicated by funnel plot asymmetry and dose-response meta-regression for sample size (p = 0.04) (eAppendix 8).
Olanzapine
There was moderate confidence of evidence of an almost linear relationship with negligible ORs for doses up to 20 mg/d, and small-to-medium ORs at higher doses reaching a maximum of OR 2.73 [0.78, 9.54] at 40 mg/d. Nevertheless, there were only limited data at doses >20 mg/d from a single study [50], and the 95%CI were wide and could not exclude the null and large effects (n = 16, N = 3813, k = 40, median VPC = 20.4%, p value = 0.28).
Doses up to 20 mg/d were available from one 26-weeks study in patients with predominant negative symptoms [51]. There was very low confidence of evidence of a flat curve and a maximum OR 1.14 [0.42, 3.11] at 20 mg/d, yet 95%CI were wide and did not exclude the null and medium effects (n = 1, N = 174, k = 3, VPC not estimable, p value = 0.91).
Paliperidone
There was high confidence of evidence of an increasing linear curve reaching small-to-medium ORs up to a maximum OR 2.07 [1.31, 3.26] at 15 mg/d (n = 11, N = 4215, k = 36; median VPC = 35%, p value = 0.007).
Quetiapine
There was moderate confidence of evidence of a relatively flat curve indicating no relationship and a negligible risk of a maximum OR 1.11 [0.48, 2.55] at 1200 mg/d (n = 9, N = 3058, k = 32; median VPC = 30.7%; p value = 0.94). Nevertheless, high doses >800 mg/d were only investigated in two studies with treatment-resistant patients [52, 53].
Risperidone
There was high confidence of evidence of an increasing linear curve with small-to-medium ORs and reaching a maximum 3.30 [2.37, 4.61] at 16 mg/d (n = 23, N = 6151, k = 60, median VPC = 22.4%, p value < 0.001).
In first-episode patients, risperidone doses up to 6 m/g were investigated. There was very low confidence of an increasing monotonic relationship reaching a maximum OR 3.53 [0.05, 232.38] at 6 mg/d. Nevertheless, the 95%CI were wide and did not exclude the null and large effects (n = 2, N = 72, k = 4; medium VPC = 19.4%, p = 0.64).
Sertindole
There was moderate confidence of evidence of a relatively flat curve indicating no relationship and a negligible risk up to a maximum OR 1.10 [0.70, 1.73] at 24 mg/d (n = 4, N = 1332, k = 15; median VPC = 0%; p value = 0.12).
Ziprasidone
There was low confidence of a linear curve with small-to-medium ORs reaching up to 3.06 [1.47, 6.38] at 320 mg/d (n = 8, N = 1785, k = 25, median VPC = 28.9%; p value = 0.003).
Zotepine
There was very low confidence of a relatively flat curve with small ORs reaching up to 1.38 [0.03, 68.44] at 208 mg/d, but 95%CI were very wide and could not exclude the null and larger effects (n = 2, N = 119, k = 4, median VPC = 40.9%; p value = 0.99).
Sensitivity analyses
We only conducted sensitivity analyses in chronically-ill patients with schizophrenia, since we had sparse data in predominant negative symptoms and first-episode schizophrenia. The results did not materially change in sensitivity analyses, yet some analyses had limited power, i.e., comparisons between different formulations. A more detailed discussion is provided in eAppendix 7. Notably, there were some differences in the magnitude of odds ratios (ORs) across the different outcome measures for extrapyramidal side-effects, and particularly, ORs derived from scale-derived data tended to be smaller than from the number of patients receiving antiparkinsonian medication or those with at least one EPS (eAppendix 7). Nevertheless, their dose-response curves had generally similar shapes.
D2R occupancy and risk of EPS
We post-hoc plotted the dose-response curves of individual antipsychotics by converting daily doses to median D2R occupancies using readily available formulas for aripiprazole, amisulpride, haloperidol, olanzapine paliperidone, quetiapine, risperidone, and ziprasidone [11]. We downrated the confidence in the evidence given that D2R occupancies were estimated from the administered doses [11]. It should also be highlighted that there were no available formulas from Lako et al 2013 to estimate D2R occupancies from the daily dose of the other included antipsychotics [11]. There were also no usable EPS data for clozapine, as mentioned above.
The curves of D2R antagonists had generally a similar shape indicating a substantial increase of the risk of EPS at D2R occupancies above 75–85% (Fig. 3). To further explore this relationship, we combined findings for D2R antagonists in a dose-response meta-analysis by using the estimated median D2R occupancy instead of the dose (Fig. 4). Again, we found that the risk of EPS was negligible to small at D2R occupancies below 75–85% (e.g., OR60% = 1.22 [0.99, 1.52], OR80% = 1.73 [1.38, 2.17]), but increased substantially at D2R occupancies exceeding 75–85% reaching up to OR90% = 2.96 [1.72, 5.07] (n = 68, N = 17396, k = 194; median VPC = 48.1%; p value < 0.001). However, the confidence in the evidence was low due to major concerns in indirectness, i.e., estimation of the median D2R occupancy from the dose of six antipsychotics (eAppendix 10).
This figure shows the relationships between dopamine 2 receptor (D2R) occupancies and risk of extrapyramidal side-effects (EPS) of seven individual antipsychotics (amisulpride, aripiprazole, haloperidol, olanzapine, quetiapine, risperidone, ziprasidone). The X-axis displays the median D2R occupancies (%) calculated from prescribed daily doses using formulas from Lako et al 2013 [11]. There were no available data and/or formulas for the other antipsychotics considered in this review. The Y-axis displays the corresponding ORs for the risk of EPS associated with a specific level of D2R occupancy compared with non-exposure (i.e., placebo or 0%). The colored areas display the 95% confidence intervals (95%CI). The color key displays the confidence in the evidence according to the GRADE approach (green=high, blue=moderate, yellow=low, red=very low). D2R dopamine 2 receptor; EPS extrapyramidal side-effects; OR odds ratio.
This figure shows the relationships between dopamine 2 receptor (D2R) occupancies and risk of extrapyramidal side-effects (EPS) of D2R antagonists combined (amisulpride, haloperidol, olanzapine, quetiapine, risperidone, ziprasidone). The X-axis displays the median D2R occupancies (%) calculated from prescribed daily doses using formulas from Lako et al 2013 [11]. There were no available data and/or formulas for the other antipsychotics considered in this review. The Y-axis displays the corresponding ORs for the risk of EPS associated with a specific level of D2R occupancy compared with non-exposure (i.e. placebo or 0%). The colored areas display the 95% confidence intervals (95%CI). The color key displays the confidence in the evidence according to the GRADE approach (green=high, blue=moderate, yellow=low, red=very low). D2R dopamine 2 receptor; EPS extrapyramidal side-effects; OR odds ratio.
On the other hand, the curve of the partial D2R agonist aripiprazole was relatively flat and the risk of EPS was small even at D2R occupancies above 85% (Fig. 3). As mentioned above, we could not estimate curves of the other partial D2R agonists, i.e., brexpiprazole and cariprazine, due to the lack of available formulas for these antipsychotics [11].
Discussion
This dose-response meta-analysis provided the most comprehensive and up-to-date synthesis of randomized evidence on the relationship between dose, D2R occupancy and extrapyramidal side-effects (EPS) of antipsychotics.
Summary of findings
We found that almost all antipsychotic drugs could cause dose-dependent EPS, except for quetiapine and sertindole (no data for clozapine, very low quality of findings for iloperidone and zotepine). However, the risk of EPS varied across antipsychotics in accordance to the well-established evidence from a previous network meta-analysis [21].
Our analysis identified two main shapes of dose-response curves: (i) monotonic or linear curves indicating a rising risk of EPS with increasing doses of haloperidol, lurasidone, amisulpride, lumateperone, cariprazine, risperidone, ziprasidone, olanzapine, asenapine, paliperidone, brexpiprazole, and aripiprazole (in descending order of their maximum ORs), and (ii) flat curves indicating no dose-response relationship for iloperidone, quetiapine, sertindole, and zotepine.
Notably, we had very low confidence in the estimates of the effects for certain groups and medications. Specifically, we had very low confidence in the estimates for individuals with predominant negative symptoms and first-episode schizophrenia, as well as for cariprazine, iloperidone, and zotepine in people with acute exacerbations. This uncertainty suggests that future research could easily change their results.
Dose-dependent EPS and the D2R therapeutic window
Our findings were generally consistent with previous reviews on dose-effects [22, 54, 55] and can be at least partially explained by the D2R therapeutic window of antipsychotics, which suggests that risk of EPS increases when D2R occupancies exceed 75–85% [8, 11,12,13,14, 17].
We found not only that the risk of EPS could increase abruptly when the occupancy of D2R exceeds 75–85%, but also the magnitude of OR was approximately 2 at antipsychotic doses corresponding to D2R occupancy of 75–85% (Fig. 3). On the other hand, antipsychotics with D2R occupancies below 80% at their clinically effective doses, may be associated with a negligible or small risk of EPS, as we found in our analysis for quetiapine and olanzapine (recommended dose up to 20 mg/d). Similar findings have also been observed for sertindole, clozapine, and lumateperone (recommended dose 60 mg/d) [8, 56, 57], although we could not estimate the D2R occupancy for these drugs due to the lack of usable data and/or readily available formulas (eAppendix 2) [11].
Although the D2R therapeutic window provides a good framework for understanding the relationship between antipsychotic doses and EPS, other potential mechanisms cannot be disregarded. These mechanisms could include protective effects of slow association or fast dissociation from the D2R7, 5-HT2AR and 5-HT2CR antagonism, and 5-HT1AR partial agonism [8, 18,19,20]. In particular, nondopaminergic mechanisms like 5-HT2AR antagonism have been proposed to potentially explain the lower risk of EPS for certain antipsychotics such as asenapine, iloperidone, and sertindole [20]. However, this theory has been challenged, e.g., amisulpride, a relatively selective D2R antagonist, seems to have a comparable risk to other antipsychotics that act as 5-HT2AR antagonists such as risperidone [8, 21]. Nevertheless, caution is necessary when interpreting the D2R occupancy curve of combined antipsychotics (Fig. 4) due to their variable receptor-binding profiles [6,7,8, 21]. Notably, there were differences among antipsychotics at higher doses despite similar D2R occupancies, such as between haloperidol 11 mg/d with OR = 4.7 and risperidone 16 mg/d with OR = 3.3 even though both had D2R occupancy of around 87% (Fig. 3).
Additionally, partial D2R agonists, i.e., aripiprazole, brexpiprazole and cariprazine, do not conform to the conventional D2R therapeutic window due to their unique pharmacological properties [8, 42, 58, 59]. Compared to D2R antagonists, these compounds have a low intrinsic activity on D2R, which may vary depending on the brain region, receptor sensitivity and cell systems [42, 60]. At clinical effective doses, partial agonists exhibit higher D2R occupancies beyond 80% exerting their antipsychotic effect, while still retaining some dopaminergic signalling resulting in a reduced risk of EPS [8, 42, 58, 59].
Accordingly, we found that aripiprazole did not cause EPS at D2R occupancy of 80% (OR = 1.05 at 3 mg/d), and the risk remained low even at higher occupancies (up to OR = 1.57 at 30 mg/d). The other partial agonists had a higher risk compared with aripiprazole even at doses with D2R occupancy of about 80% [61, 62], i.e., brexpiprazole (OR = 1.42 at 4 mg/d) and cariprazine (OR = 1.69 at 3 mg/d). Their higher risk of EPS can be potentially explained by their lower intrinsic activity compared with aripiprazole [63].
Implications to clinical practice
In our previous meta-analysis, we investigated the dose-response curves for the acute efficacy of antipsychotics and identified their near-maximal doses that achieve 95% of the maximum efficacy (ED95) [15]. Nonetheless, decisions concerning antipsychotic doses should consider potential side-effects, many of which are dose-dependent [22, 25, 64]. Hence, the present dose-response meta-analysis on extrapyramidal side-effects (EPS) can offer additional evidence-based information that can guide treatment decisions about antipsychotics for schizophrenia. To further facilitate the interpretation of the current analysis, we provided an overview of the EPS risk at the recommended and ED95 doses of antipsychotics in eAppendix 11 [15].
Most antipsychotics have a hyperbolic relationship between dose and efficacy with a plateau at ED95 doses [15], yet their dose-response curves for EPS are almost linear. For example, aripiprazole doses above ~12 mg/d, and haloperidol and risperidone doses above 6 mg/d, are not more efficacious on average [15], but can increase the risk of EPS. However, dose-effects can differ among antipsychotics. Olanzapine, for instance, may have higher efficacy at higher doses [15], but also an increased risk of EPS beyond the maximum recommended dose of 20 mg/d. Sertindole, on the other hand, may not cause EPS across doses, although higher doses may be more efficacious [15]; the risk of QTc prolongation should not be overlooked [21]. Thus, dose-response curves can optimize benefit-risk evaluations and support shared-decision-making frameworks in selecting antipsychotic medications [65].
Additionally, the linear dose-response curves for EPS observed in most antipsychotics suggest that dose reduction could potentially mitigate these adverse events, which is in line with our previous Cochrane review on antipsychotic dose reduction [66].
Limitations
The analysis has certain limitations. First, we defined our primary outcome post-hoc as the number of participants receiving antiparkinsonian medications and used other proxies when data were not available. This decision was made in order to provide a comprehensive analysis and increase the power to estimate dose-response relationships. We gave preference to the use of antiparkinsonian medications as a measure of global EPS, as it was often used in previous analyses [21, 67]. We also prioritised dichotomous outcomes over scale-derived data due to skewness [67]. In a sensitivity analysis comparing dichotomous to scale-derived data (by estimating ORs from SMDs), we found that effect sizes were generally smaller for the latter (eAppendix 7). This could be potentially attributed to skewness (e.g., large SDs may dilute SMDs) and/or the transient nature of EPS during the study, resulting in small mean changes from baseline to endpoint [68]. A previous dose-response meta-analysis analysed only scale-derived data, which could also explain some of the differences in the findings with the current analysis [54].
Second, the term “EPS” is an umbrella term of heterogenous treatment-emergent movement disorders that could have different etiopathogeneses and require different treatments [1]. Our study primarily focused on parkinsonism and other movement disorders that could be treated with anticholinergic medications. Thus, the findings cannot be directly extrapolated to akathisia and tardive dyskinesia that have different pathogenetic mechanisms and need for distinct interventions [1]. For this reason, we conducted a separate dose-response meta-analysis on antipsychotic-induced akathisia, which revealed often but not always differing shapes of dose-response curves between akathisia and EPS [64]. This may also be relevant for antipsychotics like aripiprazole that have a clinically-important risk of akathisia, albeit a generally small risk of EPS [21]. In particular, we found that the risk of akathisia reached a plateau of OR = 1.8–2.0 at approximately 10–15 mg/d of aripiprazole [64], whereas the risk of EPS was trivial OR = 1.2–1.3 at these doses, but slightly increased up to OR = 1.57 at 30 mg/d (Fig. 2).
Third, we used on data from clinical trials in schizophrenia, and thus caution is needed in when extrapolating our findings to other conditions. For example, individuals with bipolar disorder may be more vulnerable to antipsychotic-induced EPS, even with aripiprazole and quetiapine [69], yet only a few clinical trials investigated fixed-doses of antipsychotics in this population [70]. In addition, there were limited data for patient subgroups that could be more sensitive to EPS, e.g., paediatric, first-episode and elderly patients.
Fourth, we analysed daily doses, which do not accurately reflect plasma concentrations, the subsequent receptor occupancy and clinical effects [10]. A high interpersonal variability can be expected, and thus, participant characteristics that could influence this relationship, e.g., age, sex, weight, pharmacogenetics, concomitant medications, and comorbidities, should be considered in the interpretation of the findings and future analysis with individual-participant-data is warranted. This limitation was taken into consideration in the estimation of the D2R occupancy (eAppendix 2) [11], and the confidence in the evidence was downrated accordingly (eAppendix 10).
Furthermore, the findings on D2R occupancy were based on only seven antipsychotics (Figs. 3 and 4) due to the lack of usable EPS data and/or formulas from Lako et al 2013 [11] to estimate the D2R occupancy for the other antipsychotics. Thus, we could not estimate the D2R occupancy for the newer compounds, such as cariprazine, brexpiprazole, lumateperone and lurasidone, as well as for potential “outlier” medications with low D2R occupancy risk of EPS, such as sertindole and clozapine. As a result, we had to downrate the confidence in the evidence due to indirectness (eAppendix 10).
Additionally, we a priori excluded first-generation antipsychotics except for haloperidol, which is the “gold standard” active comparator in antipsychotic trials [71]. Although first-generation antipsychotics could have been relevant to this analysis, given their generally higher risk of EPS [21], they are of limited importance in current clinical practice and have been inadequately examined, mainly in older clinical trials that often employed flexible-dosing schedules, which are ineligible for this analysis [71,72,73]. The reporting quality of adverse events in these earlier trials is also often inconsistent and inadequate [74,75,76], which may result in the available data on EPS not being presented in a way that allows for dose-response analysis.
Last, it is suggested that long-acting injections may have a lower risk of EPS [68], yet there were no clear differences in our analyses, which was however based on sparse data for the different formulations.
Conclusion
This dose-response meta-analysis quantified the relationship between antipsychotic doses and the risk of EPS in schizophrenia. The risk of EPS increased with higher doses of antipsychotics, albeit with varying degrees across medications. Notably, quetiapine and sertindole exhibited no association with EPS even at high doses, and there were no usable data for clozapine.
The dose-response curves for antipsychotic-induced EPS, along with those for efficacy and other side-effects, can inform the decision-making about antipsychotic treatment for schizophrenia. Nevertheless, participant characteristics that could influence dose-response relationships should be considered in the interpretation of the findings and their impact should be further elucidated in future research.
Furthermore, our analysis used clinical trial data to quantify the relationship between D2R occupancy and the risk of EPS, and provided additional insights into the current therapeutic window for EPS.
References
Stahl SM, Sy S, Maguire GA. How and when to treat the most common adverse effects of antipsychotics: Expert review from research to clinical practice. Acta Psychiatr Scand. 2021;143:172–80.
Novick D, Haro JM, Bertsch J, Haddad PM. Incidence of extrapyramidal symptoms and tardive dyskinesia in schizophrenia: thirty-six-month results from the European schizophrenia outpatient health outcomes study. J Clin Psychopharmacol. 2010;30:531–40.
DiBonaventura M, Gabriel S, Dupclay L, Gupta S, Kim E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry. 2012;12:20.
Joshi YB, Thomas ML, Braff DL, Green MF, Gur RC, Gur RE, et al. Anticholinergic medication burden–associated cognitive impairment in schizophrenia. Am J Psychiatry. 2021;178:838–47.
Ginovart N, Kapur S. Role of dopamine D(2) receptors for antipsychotic activity. Handb Exp Pharm. 2012;212:27–52.
Siafis S, Davis JM, Leucht S. Antipsychotic drugs: from 'major tranquilizers' to Neuroscience-based-Nomenclature. Psychol Med. 2021;51:522–4.
Sykes DA, Moore H, Stott L, Holliday N, Javitch JA, Lane JR, et al. Extrapyramidal side effects of antipsychotics are linked to their association kinetics at dopamine D2 receptors. Nat Commun. 2017;8:763.
Kaar SJ, Natesan S, McCutcheon R, Howes OD. Antipsychotics: mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacology. 2020;172:107704.
Kenakin T. Principles: receptor theory in pharmacology. Trends Pharm Sci. 2004;25:186–92.
Hiemke C, Bergemann N, Clement HW, Conca A, Deckert J, Domschke K, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: Update 2017. Pharmacopsychiatry. 2018;51:9–62.
Lako IM, van den Heuvel ER, Knegtering H, Bruggeman R, Taxis K. Estimating dopamine D2 receptor occupancy for doses of 8 antipsychotics: a meta-analysis. J Clin Psychopharmacol. 2013;33:675–81.
Uchida H, Takeuchi H, Graff-Guerrero A, Suzuki T, Watanabe K, Mamo DC. Dopamine D2 receptor occupancy and clinical effects: a systematic review and pooled analysis. J Clin Psychopharmacol. 2011;31:497–502.
Kapur S, Zipursky R, Jones C, Remington G, Houle S. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157:514–20.
Farde L, Nordström AL, Wiesel FA, Pauli S, Halldin C, Sedvall G. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry. 1992;49:538–44.
Leucht S, Crippa A, Siafis S, Patel MX, Orsini N, Davis JM. Dose-response meta-analysis of antipsychotic drugs for acute schizophrenia. Am J Psychiatry. 2020;177:342–53.
Leucht S, Bauer S, Siafis S, Hamza T, Wu H, Schneider-Thoma J, et al. Examination of dosing of antipsychotic drugs for relapse prevention in patients with stable schizophrenia: a meta-analysis. JAMA Psychiatry. 2021;78:1238–48.
de Greef R, Maloney A, Olsson-Gisleskog P, Schoemaker J, Panagides J. Dopamine D2 occupancy as a biomarker for antipsychotics: quantifying the relationship with efficacy and extrapyramidal symptoms. Aaps j. 2011;13:121–30.
Nguyen TT, Pariente A, Montastruc JL, Lapeyre-Mestre M, Rousseau V, Rascol O, et al. An original pharmacoepidemiological-pharmacodynamic method: application to antipsychotic-induced movement disorders. Br J Clin Pharm. 2017;83:612–22.
Olten B, Bloch MH. Meta regression: Relationship between antipsychotic receptor binding profiles and side-effects. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;84:272–81.
Sykes DA, Lochray J, Comfort HM, Jain P, Charlton SJ. Exploring the kinetic selectivity of antipsychotics for dopamine D2 and 5-HT2A receptors: implications for the prevalence of EPS and receptor occupancy. bioRxiv 2021:2021–11.
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394:939–51.
Yoshida K, Takeuchi H. Dose-dependent effects of antipsychotics on efficacy and adverse effects in schizophrenia. Behav Brain Res. 2021;402:113098.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Schneider-Thoma J, Efthimiou O, Bighelli I, Dörries C, Huhn M, Krause M, et al. Second-generation antipsychotic drugs and short-term somatic serious adverse events: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6:753–65.
Wu H, Siafis S, Hamza T, Schneider-Thoma J, Davis JM, Salanti G, et al. Antipsychotic-induced weight gain: dose-response meta-analysis of randomized controlled trials. Schizophr Bull. 2022;48:643–54.
Younis IR, Gopalakrishnan M, Mathis M, Mehta M, Uppoor R, Zhu H, et al. Association of end point definition and randomized clinical trial duration in clinical trials of schizophrenia medications. JAMA Psychiatry. 2020;77:1064–71.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Wiley and Sons: Chichester, UK, 2011.
Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol. 2002;31:140–9.
Whiting-O'Keefe QE, Henke C, Simborg DW. Choosing the correct unit of analysis in Medical Care experiments. Med Care. 1984;22:1101–14.
Shokraneh F, Adams CE. Cochrane Schizophrenia group’s study-based register of randomized controlled trials: development and content analysis. Schizophrenia Bull Open. 2020;1:sgaa061.
Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19.
Corporation M. Microsoft Access. https://office.microsoft.com/access 2019.
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59:7–10.
Bakbergenuly I, Hoaglin DC, Kulinskaya E. Pitfalls of using the risk ratio in meta-analysis. Res Synth Methods. 2019;10:398–419.
Doi SA, Furuya-Kanamori L, Xu C, Chivese T, Lin L, Musa OAH, et al. The Odds Ratio is "portable" across baseline risk but not the Relative Risk: Time to do away with the log link in binomial regression. J Clin Epidemiol. 2022;142:288–93.
Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19:3127–31.
Hasselblad V, Hedges LV. Meta-analysis of screening and diagnostic tests. Psychological Bull. 1995;117:167.
da Costa BR, Rutjes AW, Johnston BC, Reichenbach S, Nüesch E, Tonia T, et al. Methods to convert continuous outcomes into odds ratios of treatment response and numbers needed to treat: meta-epidemiological study. Int J Epidemiol. 2012;41:1445–59.
Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat—Simul Comput®. 2010;39:860–4.
Crippa A, Discacciati A, Bottai M, Spiegelman D, Orsini N. One-stage dose–response meta-analysis for aggregated data. Stat Methods Med Res. 2019;28:1579–96.
Crippa A, Orisini N. Multivariate dose-response meta-analysis: the dosresmeta R package. J Stat Softw, Code Snippets. 2016;72:1–15.
Grunder G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60:974–7.
de Greef R, Maloney A, Olsson-Gisleskog P, Schoemaker J, Panagides J. Dopamine D2 occupancy as a biomarker for antipsychotics: quantifying the relationship with efficacy and extrapyramidal symptoms. AAPS J. 2011;13:121–30.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Team RC. R: a language and environment for statistical computing. Version 4.0. 3. Vienna, Austria. 2020.
Puech A, Fleurot O. Rein W. Amisulpride, an atypical antipsychotic, in the treatment of acute episodes of schizophrenia: a dose-ranging study vs. haloperidol. Acta PsychiatrScand. 1998;98:65–72.
Krause M, Zhu Y, Huhn M, Schneider-Thoma J, Bighelli I, Nikolakopoulou A, et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: a systematic review and meta-analysis. Eur Arch psychiatry Clin Neurosci. 2018;268:625–39.
Meltzer HY, Share DB, Jayathilake K, Salomon RM, Lee MA. Lurasidone improves psychopathology and cognition in treatment-resistant schizophrenia. J Clin Psychopharmacol. 2020;40:240.
Kinon BJ, Volavka J, Stauffer V, Edwards SE, Liu-Seifert H, Chen L, et al. Standard and higher dose of olanzapine in patients with schizophrenia or schizoaffective disorder: a randomized, double-blind, fixed-dose study. J Clin Psychopharmacol. 2008;28:392–400.
Lecrubier Y, Quintin P, Bouhassira M, Perrin E, Lancrenon S. The treatment of negative symptoms and deficit states of chronic schizophrenia: olanzapine compared to amisulpride and placebo in a 6-month double-blind controlled clinical trial. Acta Psychiatr Scandinavica. 2006;114:319–27.
Honer WG, MacEwan GW, Gendron A, Stip E, Labelle A, Williams R, et al. A randomized, double-blind, placebo-controlled study of the safety and tolerability of high-dose quetiapine in patients with persistent symptoms of schizophrenia or schizoaffective disorder. J Clin Psychiatry. 2012;73:13–20.
Lindenmayer JP, Citrome L, Khan A, Kaushik S, Kaushik S. A randomized, double-blind, parallel-group, fixed-dose, clinical trial of quetiapine at 600 versus 1200 mg/d for patients with treatment-resistant schizophrenia or schizoaffective disorder. J Clin Psychopharmacol. 2011;31:160–8.
Sabe M, Zhao N, Crippa A, Kaiser S. Antipsychotics for negative and positive symptoms of schizophrenia: dose-response meta-analysis of randomized controlled acute phase trials. npj Schizophrenia. 2021;7:1–11.
Takeuchi H, MacKenzie NE, Samaroo D, Agid O, Remington G, Leucht S. Antipsychotic dose in acute schizophrenia: a meta-analysis. Schizophrenia Bull. 2020;46:1439–58.
Kasper S, Tauscher J, Küfferle B, Barnas C, Hesselmann B, Asenbaum S, et al. Sertindole and dopamine D2 receptor occupancy in comparison to risperidone, clozapine and haloperidol - a 123I-IBZM SPECT study. Psychopharmacol (Berl). 1998;136:367–73.
Vanover KE, Davis RE, Zhou Y, Ye W, Brašić JR, Gapasin L, et al. Dopamine D(2) receptor occupancy of lumateperone (ITI-007): a Positron Emission Tomography Study in patients with schizophrenia. Neuropsychopharmacology. 2019;44:598–605.
Kegeles LS, Slifstein M, Frankle WG, Xu X, Hackett E, Bae SA, et al. Dose-occupancy study of striatal and extrastriatal dopamine D2 receptors by aripiprazole in schizophrenia with PET and [18 F]fallypride. Neuropsychopharmacology. 2008;33:3111–25.
Hart XM, Schmitz CN, Gründer G. Molecular imaging of dopamine partial agonists in humans: implications for clinical practice. Front Psychiatry. 2022;13:832209.
de Bartolomeis A, Tomasetti C, Iasevoli F. Update on the mechanism of action of aripiprazole: translational insights into antipsychotic strategies beyond dopamine receptor antagonism. CNS Drugs. 2015;29:773–99.
Girgis RR, Forbes A, Abi-Dargham A, Slifstein M. A positron emission tomography occupancy study of brexpiprazole at dopamine D(2) and D(3) and serotonin 5-HT(1 A) and 5-HT(2 A) receptors, and serotonin reuptake transporters in subjects with schizophrenia. Neuropsychopharmacology. 2020;45:786–92.
Girgis RR, Slifstein M, D’Souza D, Lee Y, Periclou A, Ghahramani P, et al. Preferential binding to dopamine D3 over D2 receptors by cariprazine in patients with schizophrenia using PET with the D3/D2 receptor ligand [(11)C]-( + )-PHNO. Psychopharmacol (Berl). 2016;233:3503–12.
Mohr P, Masopust J, Kopeček M. Dopamine receptor partial agonists: Do they differ in their clinical efficacy? Front Psychiatry. 2021;12:781946.
Wu H, Siafis S, Wang D, Burschinski A, Schneider-Thoma J, Priller J, et al. Antipsychotic-induced akathisia in adults with acute schizophrenia: A systematic review and dose-response meta-analysis. Eur Neuropsychopharmacol. 2023;72:40–9.
Siafis S, Bursch N, Müller K, Schmid L, Schuster F, Waibel J, et al. Evidence-based shared-decision-making assistant (SDM-assistant) for choosing antipsychotics: protocol of a cluster-randomized trial in hospitalized patients with schizophrenia. BMC Psychiatry. 2022;22:406.
Rodolico A, Siafis S, Bighelli I, Samara MT, Hansen WP, Salomone S, et al. Antipsychotic dose reduction compared to dose continuation for people with schizophrenia. Cochrane Database Syst Rev. 2022;11:Cd014384.
Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Kissling W, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. 2012;38:167–77.
Gopal S, Liu Y, Alphs L, Savitz A, Nuamah I, Hough D. Incidence and time course of extrapyramidal symptoms with oral and long-acting injectable paliperidone: a posthoc pooled analysis of seven randomized controlled studies. Neuropsychiatr Dis Treat. 2013;9:1381–92.
Gao K, Kemp DE, Ganocy SJ, Gajwani P, Xia G, Calabrese JR. Antipsychotic-induced extrapyramidal side effects in bipolar disorder and schizophrenia: a systematic review. J Clin Psychopharmacol. 2008;28:203–9.
Yu C-L, Carvalho AF, Thompson T, Tsai T-C, Tseng P-T, Hsu C-W, et al. Comparison of antipsychotic dose equivalents for acute bipolar mania and schizophrenia. BMJ Ment Health. 2023;26:e300546.
Leucht S, Huhn M, Davis JM. Should ‘typical’, first-generation antipsychotics no longer be generally used in the treatment of schizophrenia? Eur Arch Psychiatry Clin Neurosci. 2021;271:1411–3.
Davis JM, Chen N. Dose response and dose equivalence of antipsychotics. J Clin Psychopharmacol. 2004;24:192–208.
Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:927–42.
Brunoni AR, Tadini L, Fregni F. Changes in clinical trials methodology over time: a systematic review of six decades of research in psychopharmacology. PLoS One. 2010;5:e9479.
Pope A, Adams C, Paton C, Weaver T, Barnes TR. Assessment of adverse effects in clinical studies of antipsychotic medication: survey of methods used. Br J Psychiatry. 2010;197:67–72.
Thornley B, Adams C. Content and quality of 2000 controlled trials in schizophrenia over 50 years. Bmj. 1998;317:1181–4.
Acknowledgements
We thank Jing Tian and Mengchang Qin for helping out the study selection. We thank all the authors of the included studies. We thank SanofiAventis (amisulpride), Merck (asenapine), BristolMyersSquibb (aripiprazole), Novartis (clozapine, iloperidone), Sunovion Pharmaceuticals (lurasidone), EliLilly (olanzapine), AstraZeneca (quetiapine), Janssen/Johnson&Johnson (paliperidone and risperidone, information on haloperidol could not be obtained), ROVI (risperidone ISM), Lundbeck (sertindole) and Astellas (zotepine) for replying to our letters regarding their respective compounds.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
SS: design of the review, selection of the studies, data extraction, risk of bias and quality assessments, analysis and interpretation of data, writing the first draft of the review; HW: design of the review, selection of the studies, data extraction, risk of bias and quality assessments, analysis and interpretation of data, writing the first draft review; NN: selection of studies, interpretation of data; DW: data extraction, risk of bias assessments; AB: study selection, Access database support; HT: interpretation of data; JS: design of the review, Access database management; JD: interpretation of data, providing supervision; SL: design of the review, selection of the studies, data extraction, risk of bias and quality assessments, interpretation of data, writing the first draft of the review, providing supervision. All authors critically reviewed and revised the manuscript and approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
In the past 3 years, SL has received honoraria as advisor and/or for lectures and/or for educational material from Alkermes, Angelini, Apsen, Eisai, Gedeon Richter, Janssen, Karuna, Kynexis, Lundbeck, Medichem, Medscape, Merck Sharpp and Dome, Mitshubishi, Neurotorium, NovoNordisk, Otsuka, Recordati, Roche, Rovi, Sanofi Aventis, TEVA. HT has received grants from Daiichi Sankyo and Novartis Pharma; speaker’s fees from EA Pharma, Eisai, Kyowa, Janssen, Lundbeck, Meiji Seika Pharma, MSD, Otsuka, Sumitomo Pharma, Takeda, and Yoshitomiyakuhin; and consulting fees from Janssen, Mitsubishi Tanabe Pharma, Ono, and Sumitomo Pharma. NN has received speaker fees from Meiji Seika Pharma, Otsuka, Eisai, and Sumitomo Pharma, and manuscript fees from Sumitomo Pharma. All the other authors have no conflict of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Siafis, S., Wu, H., Wang, D. et al. Antipsychotic dose, dopamine D2 receptor occupancy and extrapyramidal side-effects: a systematic review and dose-response meta-analysis. Mol Psychiatry 28, 3267–3277 (2023). https://doi.org/10.1038/s41380-023-02203-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02203-y