Abstract
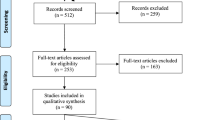
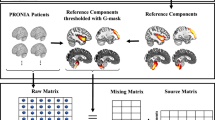
Leveraging ~10 years of prospective longitudinal data on 704 participants, we examined the effects of adolescent versus young adult cannabis initiation on MRI-assessed cortical thickness development and behavior. Data were obtained from the IMAGEN study conducted across eight European sites. We identified IMAGEN participants who reported being cannabis-naïve at baseline and had data available at baseline, 5-year, and 9-year follow-up visits. Cannabis use was assessed with the European School Survey Project on Alcohol and Drugs. T1-weighted MR images were processed through the CIVET pipeline. Cannabis initiation occurring during adolescence (14–19 years) and young adulthood (19–22 years) was associated with differing patterns of longitudinal cortical thickness change. Associations between adolescent cannabis initiation and cortical thickness change were observed primarily in dorso- and ventrolateral portions of the prefrontal cortex. In contrast, cannabis initiation occurring between 19 and 22 years of age was associated with thickness change in temporal and cortical midline areas. Follow-up analysis revealed that longitudinal brain change related to adolescent initiation persisted into young adulthood and partially mediated the association between adolescent cannabis use and past-month cocaine, ecstasy, and cannabis use at age 22. Extent of cannabis initiation during young adulthood (from 19 to 22 years) had an indirect effect on psychotic symptoms at age 22 through thickness change in temporal areas. Results suggest that developmental timing of cannabis exposure may have a marked effect on neuroanatomical correlates of cannabis use as well as associated behavioral sequelae. Critically, this work provides a foundation for neurodevelopmentally informed models of cannabis exposure in humans.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
United Nations Office on Drugs and Crime. World drug report 2018. New York, NY: United Nations publication; 2018.
Johnston LD,Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the future: national survey results on drug use 1975-2018: 2018 overview: key findings on adolescent drug use. Institute for Social Research, The University of Michigan. 2019. https://files.eric.ed.gov/fulltext/ED594190.pdf. Accessed 10 May 2021.
Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
Morin JG, Afzali MH, Bourque J, Stewart SH, Seguin JR, O’Leary-Barrett M, et al. A Population-Based Analysis of the Relationship Between Substance Use and Adolescent Cognitive Development. Am J Psychiatry. 2019;176:98–106.
Chye Y, Christensen E, Yucel M. Cannabis Use in Adolescence: A Review of Neuroimaging Findings. J Dual Diagn. 2020;16:83–105.
Lichenstein SD, Manco N, Cope LM, Egbo L, Garrison KA, Hardee J, et al. Systematic review of structural and functional neuroimaging studies of cannabis use in adolescence and emerging adulthood: evidence from 90 studies and 9441 participants. Neuropsychopharmacology. 2022;47:1000–28.
Buckner RL, Krienen FM. The evolution of distributed association networks in the human brain. Trends Cogn Sci. 2013;17:648–65.
Ducharme S, Albaugh MD, Nguyen TV, Hudziak JJ, Mateos-Perez JM, Labbe A, et al. Trajectories of cortical surface area and cortical volume maturation in normal brain development. Data Brief. 2015;5:929–38.
Ducharme S, Albaugh MD, Nguyen TV, Hudziak JJ, Mateos-Perez JM, Labbe A, et al. Trajectories of cortical thickness maturation in normal brain development-The importance of quality control procedures. Neuroimage. 2016;125:267–79.
Tamnes CK, Herting MM, Goddings AL, Meuwese R, Blakemore SJ, Dahl RE, et al. Development of the Cerebral Cortex across Adolescence: A Multisample Study of Inter-Related Longitudinal Changes in Cortical Volume, Surface Area, and Thickness. J Neurosci. 2017;37:3402–12.
Kolk SM, Rakic P. Development of prefrontal cortex. Neuropsychopharmacology. 2022;47:41–57.
Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron. 2010;67:728–34.
Shaw P, Gilliam M, Liverpool M, Weddle C, Malek M, Sharp W, et al. Cortical development in typically developing children with symptoms of hyperactivity and impulsivity: support for a dimensional view of attention deficit hyperactivity disorder. Am J Psychiatry. 2011;168:143–51.
Shaw P, Kabani NJ, Lerch JP, Eckstrand K, Lenroot R, Gogtay N, et al. Neurodevelopmental trajectories of the human cerebral cortex. J Neurosci. 2008;28:3586–94.
O’Shea M, McGregor IS, Mallet PE. Repeated cannabinoid exposure during perinatal, adolescent or early adult ages produces similar longlasting deficits in object recognition and reduced social interaction in rats. J Psychopharmacol. 2006;20:611–21.
Leweke FM, Schneider M. Chronic pubertal cannabinoid treatment as a behavioural model for aspects of schizophrenia: effects of the atypical antipsychotic quetiapine. Int J Neuropsychopharmacol. 2011;14:43–51.
Rubino T, Realini N, Braida D, Alberio T, Capurro V, Vigano D, et al. The depressive phenotype induced in adult female rats by adolescent exposure to THC is associated with cognitive impairment and altered neuroplasticity in the prefrontal cortex. Neurotox Res. 2009;15:291–302.
Rubino T, Vigano D, Realini N, Guidali C, Braida D, Capurro V, et al. Chronic delta 9-tetrahydrocannabinol during adolescence provokes sex-dependent changes in the emotional profile in adult rats: behavioral and biochemical correlates. Neuropsychopharmacology. 2008;33:2760–71.
Lee HL, Jung KM, Fotio Y, Squire E, Palese F, Lin L, et al. Frequent low-dose Δ9-tetrahydrocannabinol in adolescence disrupts microglia homeostasis and disables responses to microbial infection and social stress in young adulthood. Biol Psychiatry. 2022;92:845–60.
Rubino T, Parolaro D. Long lasting consequences of cannabis exposure in adolescence. Mol Cell Endocrinol. 2008;286:S108–13.
Albaugh MD, Ottino-Gonzalez J, Sidwell A, Lepage C, Juliano A, Owens MM, et al. Association of Cannabis Use During Adolescence With Neurodevelopment. JAMA Psychiatry. 2021;78:1–11. https://doi.org/10.1016/j.biopsych.2022.04.017. [Epub ahead of print].
Owens MM, Albaugh MD, Allgaier N, Yuan D, Robert G, Cupertino RB, et al. Bayesian causal network modeling suggests adolescent cannabis use accelerates prefrontal cortical thinning. Transl Psychiatry. 2022;12:188.
Hibell B, Andersson B, Bjarnason T, Ahlström S, Balakireva O, Kokkevi A, et al. The ESPAD report 2003: alcohol and other drug use among students in 35 european countries. Swedish Council for Information on Alcohol and Other Drugs; 2004. http://www.espad.org/sites/espad.org/files/The_2003_ESPAD_report.pdf.
Shevlin M, Smith GW. The factor structure and concurrent validity of the alcohol use disorder identification test based on a nationally representative UK sample. Alcohol Alcohol. 2007;42:582–7.
Bradley KA, McDonell MB, Bush K, Kivlahan DR, Diehr P, Fihn SD. The AUDIT alcohol consumption questions: reliability, validity, and responsiveness to change in older male primary care patients. Alcoholism Clin Exp Res. 1998;22:1842–9.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Int Med. 1998;158:1789–95.
Sobell LC, Toneatto T, Sobell MB, Leo GI, Johnson L. Alcohol abusers’ perceptions of the accuracy of their self-reports of drinking: implications for treatment. Addict Behav. 1992;17:507–11.
Stefanis NC, Hanssen M, Smirnis NK, Avramopoulos DA, Evdokimidis IK, Stefanis CN, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. 2002;32:347–58.
Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–6.
Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–45.
Sherif T, Rioux P, Rousseau ME, Kassis N, Beck N, Adalat R, et al. CBRAIN: a web-based, distributed computing platform for collaborative neuroimaging research. Front Neuroinform. 2014;8:54.
Diggle P. Analysis of longitudinal data. 2nd ed. Oxford; New York: Oxford University Press; 2002. xv, p. 379.
Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. Oxford; New York: Oxford University Press; 2003. xx, p. 644.
Ducharme S, Albaugh MD, Hudziak JJ, Botteron KN, Nguyen TV, Truong C, et al. Anxious/depressed symptoms are linked to right ventromedial prefrontal cortical thickness maturation in healthy children and young adults. Cereb Cortex. 2014;24:2941–50.
Vijayakumar N, Mills KL, Alexander-Bloch A, Tamnes CK, Whittle S. Structural brain development: A review of methodological approaches and best practices. Dev Cogn Neurosci. 2018;33:129–48.
Walhovd KB, Fjell AM, Giedd J, Dale AM, Brown TT. Through Thick and Thin: a Need to Reconcile Contradictory Results on Trajectories in Human Cortical Development. Cereb Cortex. 2017;27:1472–81.
Worsley KJ, Taylor JE, Tomaiuolo F, Lerch J. Unified univariate and multivariate random field theory. Neuroimage. 2004;23:S189–95.
Andrews DS, Avino TA, Gudbrandsen M, Daly E, Marquand A, Murphy CM, et al. In Vivo Evidence of Reduced Integrity of the Gray-White Matter Boundary in Autism Spectrum Disorder. Cereb Cortex. 2017;27:877–87.
Ecker C, Ginestet C, Feng Y, Johnston P, Lombardo MV, Lai MC, et al. Brain surface anatomy in adults with autism: the relationship between surface area, cortical thickness, and autistic symptoms. JAMA Psychiatry. 2013;70:59–70.
Hong SJ, Bernhardt BC, Schrader DS, Bernasconi N, Bernasconi A. Whole-brain MRI phenotyping in dysplasia-related frontal lobe epilepsy. Neurology. 2016;86:643–50.
Valk SL, Bernhardt BC, Trautwein FM, Bockler A, Kanske P, Guizard N, et al. Structural plasticity of the social brain: Differential change after socio-affective and cognitive mental training. Sci Adv. 2017;3:e1700489.
The jamovi project. jamovi 2021 [Version 1.6:[https://www.jamovi.org.
Sahin MD, Aybek EC. Jamovi: An Easy to Use Statistical Software for the Social Scientists. Int J Assess Tools E. 2019;6:670–92.
Cheng J, Cheng NF, Guo Z, Gregorich S, Ismail AI, Gansky SA. Mediation analysis for count and zero-inflated count data. Stat Methods Med Res. 2018;27:2756–74.
RStudio Team. RStudio: Integrated Development for R. Boston, MA: RStudio, PBC; 2020.
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R Package for Causal Mediation Analysis. J Stat Softw. 2014;59:1–38.
Qiu L, Yan H, Zhu R, Yan J, Yuan H, Han Y, et al. Correlations between exploratory eye movement, hallucination, and cortical gray matter volume in people with schizophrenia. BMC Psychiatry. 2018;18:226.
van Erp TGM, Walton E, Hibar DP, Schmaal L, Jiang W, Glahn DC, et al. Cortical Brain Abnormalities in 4474 Individuals With Schizophrenia and 5098 Control Subjects via the Enhancing Neuro Imaging Genetics Through Meta Analysis (ENIGMA) Consortium. Biol Psychiatry. 2018;84:644–54.
Wannan CMJ, Cropley VL, Chakravarty MM, Bousman C, Ganella EP, Bruggemann JM, et al. Evidence for Network-Based Cortical Thickness Reductions in Schizophrenia. Am J Psychiatry. 2019;176:552–63.
Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9:947–57.
Albaugh MD, Owens MM, Garavan H. Association of Alcohol With Cortical Thickness in Adolescents-Reply. JAMA Psychiatry. 2021;78:1284–5.
Chung WW, Hudziak JJ. The Transitional Age Brain: “The Best of Times and the Worst of Times”. Child Adolesc Psychiatr Clin N Am. 2017;26:157–75.
Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;1:286–93.
Fergusson DM, Boden JM, Horwood LJ. The developmental antecedents of illicit drug use: evidence from a 25-year longitudinal study. Drug Alcohol Depend. 2008;96:165–77.
Nkansah-Amankra S, Minelli M. “Gateway hypothesis” and early drug use: Additional findings from tracking a population-based sample of adolescents to adulthood. Prev Med Rep. 2016;4:134–41.
Grant JD, Lynskey MT, Scherrer JF, Agrawal A, Heath AC, Bucholz KK. A cotwin-control analysis of drug use and abuse/dependence risk associated with early-onset cannabis use. Addict Behav. 2010;35:35–41.
Castellanos-Ryan N, Pingault JB, Parent S, Vitaro F, Tremblay RE, Seguin JR. Adolescent cannabis use, change in neurocognitive function, and high-school graduation: A longitudinal study from early adolescence to young adulthood. Dev Psychopathol. 2017;29:1253–66.
Ferland JN, Ellis RJ, Betts G, Silveira MM, de Firmino JB, Winstanley CA, et al. Long-Term Outcomes of Adolescent THC Exposure on Translational Cognitive Measures in Adulthood in an Animal Model and Computational Assessment of Human Data. JAMA Psychiatry. 2023;80:66–76.
Sideli L, Quigley H, La Cascia C, Murray RM. Cannabis Use and the Risk for Psychosis and Affective Disorders. J Dual Diagn. 2020;16:22–42.
Livne O, Shmulewitz D, Sarvet AL, Wall MM, Hasin DS. Association of Cannabis Use-Related Predictor Variables and Self-Reported Psychotic Disorders: U.S. Adults, 2001-2002 and 2012-2013. Am J Psychiatry. 2022;179:36–45.
Di Forti M, Quattrone D, Freeman TP, Tripoli G, Gayer-Anderson C, Quigley H, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry. 2019;6:427–36.
Murray RM, Hall W. Will Legalization and Commercialization of Cannabis Use Increase the Incidence and Prevalence of Psychosis? JAMA Psychiatry. 2020;77:777–8.
Raznahan A, Lerch JP, Lee N, Greenstein D, Wallace GL, Stockman M, et al. Patterns of coordinated anatomical change in human cortical development: a longitudinal neuroimaging study of maturational coupling. Neuron. 2011;72:873–84.
Lebel C, Gee M, Camicioli R, Wieler M, Martin W, Beaulieu C. Diffusion tensor imaging of white matter tract evolution over the lifespan. Neuroimage. 2012;60:340–52.
Bethlehem RAI, Seidlitz J, White SR, Vogel JW, Anderson KM, Adamson C, et al. Brain charts for the human lifespan. Nature. 2022;604:525–33.
Nelson CA 3rd, Gabard-Durnam LJ. Early Adversity and Critical Periods: Neurodevelopmental Consequences of Violating the Expectable Environment. Trends Neurosci. 2020;43:133–43.
Gee DG, Casey BJ. The Impact of Developmental Timing for Stress and Recovery. Neurobiol Stress. 2015;1:184–94.
Acknowledgements
This work received support from the following sources: the European Union-funded FP6 Integrated Project IMAGEN (Reinforcement-related behavior in normal brain function and psychopathology) (LSHM-CT- 2007–037286), the Horizon 2020 funded ERC Advanced Grant ‘STRATIFY’ (Brain network based stratification of reinforcement-related disorders) (695313), Human Brain Project (HBP SGA 2, 785907, and HBP SGA 3, 945539), the Medical Research Council Grant ‘c-VEDA’ (Consortium on Vulnerability to Externalizing Disorders and Addictions) (MR/N000390/1), the National Institute of Health (NIH) (R01DA049238, A decentralized macro and micro gene-by-environment interaction analysis of substance use behavior and its brain biomarkers), the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, the Bundesministeriumfür Bildung und Forschung (BMBF grants 01GS08152; 01EV0711; Forschungsnetz AERIAL 01EE1406A, 01EE1406B; Forschungsnetz IMAC-Mind 01GL1745B), the Deutsche Forschungsgemeinschaft (DFG grants SM 80/7–2, SFB 940, TRR 265, NE 1383/14-1), the Medical Research Foundation and Medical Research Council (grants MR/R00465X/1 and MR/S020306/1), the National Institutes of Health (NIH) funded ENIGMA (grants 5U54EB020403-05 and 1R56AG058854-01). Further support was provided by grants from: – the ANR (ANR-12-SAMA-0004, AAPG2019 – GeBra), the Eranet Neuron (AF12-NEUR0008-01 – WM2NA; and ANR-18-NEUR00002-01 – ADORe), the Fondation de France (00081242), the Fondation pour la Recherche Médicale (DPA20140629802), the Mission Interministérielle de Lutte-contre-les-Drogues-et-les-Conduites-Addictives (MILDECA), the Assistance-Publique-Hôpitaux-de-Paris and INSERM (interface grant), Paris Sud University IDEX 2012, the Fondation de l’Avenir (grant AP-RM-17-013), the Fédération pour la Recherche sur le Cerveau; the National Institutes of Health, Science Foundation Ireland (16/ERCD/3797), U.S.A. (Axon, Testosterone and Mental Health during Adolescence; R01 MH085772-01A1), and by NIH Consortium grant U54 EB020403, supported by a cross-NIH alliance that funds Big Data to Knowledge Centres of Excellence. ImagenPathways “Understanding the Interplay between Cultural, Biological and Subjective Factors in Drug Use Pathways” is a collaborative project supported by the European Research Area Network on Illicit Drugs (ERANID). This paper is based on independent research commissioned and funded in England by the National Institute for Health Research (NIHR) Policy Research Programme (project ref. PR-ST-0416-10001). The views expressed in this article are those of the authors and not necessarily those of the national funding agencies or ERANID. Dr Albaugh is supported by K08 MH121654-01A1 and a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation. Drs Albaugh and Garavan had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the paper; and decision to submit the paper for publication.
Author information
Authors and Affiliations
Consortia
Contributions
MA conceived and performed the analysis, interpreted the results, and wrote the paper. AP and HG supervised the project, interpreted the results, and edited the paper. CL and PR assisted in the storage and processing of neuroimaging data. The rest of the authors contributed to the data acquisition and sharing and edited the paper.
Corresponding author
Ethics declarations
Competing interests
Dr TB has served as an advisor or consultant to Bristol-Myers Squibb, Desitin Arzneimittel, Eli Lilly, Medice, Novartis, Pfizer, Shire, UCB, and Vifor Pharma; he has received conference attendance support, conference support, or speaking fees from Eli Lilly, Janssen McNeil, Medice, Novartis, Shire, and UCB; and he is involved in clinical trials conducted by Eli Lilly, Novartis, and Shire; the present work is unrelated to these relationships. The other authors report no biomedical financial interests or potential competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Albaugh, M.D., Owens, M.M., Juliano, A. et al. Differential associations of adolescent versus young adult cannabis initiation with longitudinal brain change and behavior. Mol Psychiatry 28, 5173–5182 (2023). https://doi.org/10.1038/s41380-023-02148-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02148-2