Abstract
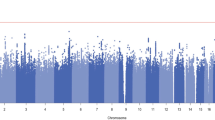
Clinical epidemiological studies have found high co-occurrence between suicide attempts (SA) and opioid use disorder (OUD). However, the patterns of correlation and causation between them are still not clear due to psychiatric confounding. To investigate their cross-phenotype relationship, we utilized raw phenotypes and genotypes from >150,000 UK Biobank samples, and genome-wide association summary statistics from >600,000 individuals with European ancestry. Pairwise association and a potential bidirectional relationship between OUD and SA were evaluated with and without controlling for major psychiatric disease status (e.g., schizophrenia, major depressive disorder, and alcohol use disorder). Multiple statistical and genetics tools were used to perform epidemiological association, genetic correlation, polygenic risk score prediction, and Mendelian randomizations (MR) analyses. Strong associations between OUD and SA were observed at both the phenotypic level (overall samples [OR = 2.94, P = 1.59 ×10−14]; non-psychiatric subgroup [OR = 2.15, P = 1.07 ×10−3]) and the genetic level (genetic correlation rg = 0.38 and 0.5 with or without conditioning on psychiatric traits, respectively). Consistently, increasing polygenic susceptibility to SA is associated with increasing risk of OUD (OR = 1.08, false discovery rate [FDR] =1.71 ×10−3), and similarly, increasing polygenic susceptibility to OUD is associated with increasing risk of SA (OR = 1.09, FDR = 1.73 ×10−6). However, these polygenic associations were much attenuated after controlling for comorbid psychiatric diseases. A combination of MR analyses suggested a possible causal association from genetic liability for SA to OUD risk (2-sample univariable MR: OR = 1.14, P = 0.001; multivariable MR: OR = 1.08, P = 0.001). This study provided new genetic evidence to explain the observed OUD-SA comorbidity. Future prevention strategies for each phenotype needs to take into consideration of screening for the other one.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All analyses were conducted using publicly available data. Complete genetic datasets for every analysis included in this study are available in the Supplement. The individual-level data publicly available summary-level data is available by application at https://www.ukbiobank.ac.uk/. For summary-level data, SA was accessed through ISGC dropbox link (upon request) or iPSYCH data repository (https://ipsych.dk/en/research/downloads). OUD and AUD were accessed through NCBI dbGaP for MVP (phs001672.v6.p1) [39]. MDD, BD, SCZ, ANX and PTSD were accessed at https://www.med.unc.edu/pgc/results-and-downloads/ and through MR Base at https://www.mrbase.org/. Code Availability: analyses were performed with standard tools, including GCTA (v 1.93.2), LDSC (v 1.0.1), and multiple R Packages (TwoSampleMR [v 0.5.5], MRPRESSO [v 1.0], MVMR [v 0.2], and MendelianRandomization [v 0.6.0]). The analysis code in R is available on request, and all data displayed in the figures are available in the Supplement. Supplementary information is available at MP’s website.
Change history
12 December 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41380-023-02341-3
References
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. 2019;394:1560–79.
Patten DK, Schultz BG, Berlau DJ. The Safety and Efficacy of Low-Dose Naltrexone in the Management of Chronic Pain and Inflammation in Multiple Sclerosis, Fibromyalgia, Crohn’s Disease, and Other Chronic Pain Disorders. Pharmacotherapy. 2018;38:382–9.
Wilkinson ST, Yarnell S, Radhakrishnan R, Ball SA, D’Souza DC. Marijuana Legalization: Impact on Physicians and Public Health. Annu Rev Med. 2016;67:453–66.
Blanco C, Volkow ND. Management of opioid use disorder in the USA: present status and future directions. Lancet. 2019;393:1760–72.
Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361:eaau1184.
Association. AP Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition). Washington, DC: American Psychiatric Association2013.
Ahmad FB RL, Sutton P. Provisional drug overdose death counts. In: Statistics NCfH (ed).2022.
Campbell G, Bruno R, Darke S, Shand F, Hall W, Farrell M, et al. Prevalence and Correlates of Suicidal Thoughts and Suicide Attempts in People Prescribed Pharmaceutical Opioids for Chronic Pain. Clin J Pain. 2016;32:292–301.
Curtin SCWM, Hedegaard H Increase in suicide in the United States, 1999–2014. NCHS data brief, vol. no 241. Hyattsville, MD: National Center for Health Statistics 2016.
Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2016;3:646–59.
WISQARS CfDCaPs. Centers for Disease Control and Prevention’s Web-based Injury Statistics Query and Reporting System. Web-based Injury Statistics Query and Reporting System. cdc.gov, 2019.
Santaella-Tenorio J, Martins SS, Cerda M, Olfson M, Keyes KM. Suicidal ideation and attempts following nonmedical use of prescription opioids and related disorder. Psychol Med. 2022;52:372–8.
Sampasa-Kanyinga H, Bakwa-Kanyinga F, Chaput JP, Hamilton HA, Elton-Marshall T, Colman I. Nonmedical use of prescription opioids, psychological distress, and suicidality among adolescents. Soc Psychiatry Psychiatr Epidemiol. 2021;56:783–91.
Rizk MM, Herzog S, Dugad S, Stanley B. Suicide Risk and Addiction: The Impact of Alcohol and Opioid Use Disorders. Curr Addict Rep. 2021;8:1–14.
Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76:S11–19.
Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112:1193–201.
Ashrafioun L, Bishop TM, Conner KR, Pigeon WR. Frequency of prescription opioid misuse and suicidal ideation, planning, and attempts. J Psychiatr Res. 2017;92:1–7.
Davis MA, Lin LA, Liu H, Sites BD. Prescription Opioid Use among Adults with Mental Health Disorders in the United States. J Am Board Fam Med. 2017;30:407–17.
Simon GE, Johnson E, Lawrence JM, Rossom RC, Ahmedani B, Lynch FL, et al. Predicting Suicide Attempts and Suicide Deaths Following Outpatient Visits Using Electronic Health Records. Am J Psychiatry 2018;175:951–60.
Oquendo MA, Volkow ND. Suicide: A Silent Contributor to Opioid-Overdose Deaths. N. Engl J Med. 2018;378:1567–9.
Bohnert ASB, Ilgen MA. Understanding Links among Opioid Use, Overdose, and Suicide. N. Engl J Med. 2019;380:71–79.
Ehrich E, Turncliff R, Du Y, Leigh-Pemberton R, Fernandez E, Jones R, et al. Evaluation of opioid modulation in major depressive disorder. Neuropsychopharmacology. 2015;40:1448–55.
Strawbridge RJ, Ward J, Ferguson A, Graham N, Shaw RJ, Cullen B, et al. Identification of novel genome-wide associations for suicidality in UK Biobank, genetic correlation with psychiatric disorders and polygenic association with completed suicide. EBioMedicine. 2019;41:517–25.
Ruderfer DM, Walsh CG, Aguirre MW, Tanigawa Y, Ribeiro JD, Franklin JC, et al. Significant shared heritability underlies suicide attempt and clinically predicted probability of attempting suicide. Mol Psychiatry. 2020;25:2422–30.
Lim KX, Rijsdijk F, Hagenaars SP, Socrates A, Choi SW, Coleman JRI, et al. Studying individual risk factors for self-harm in the UK Biobank: A polygenic scoring and Mendelian randomisation study. PLoS Med. 2020;17:e1003137.
Mullins N, Kang J, Campos AI, Coleman JRI, Edwards AC, Galfalvy H, et al. Dissecting the Shared Genetic Architecture of Suicide Attempt, Psychiatric Disorders, and Known Risk Factors. Biol Psychiatry. 2022;91:313–27.
Zhou H, Rentsch CT, Cheng Z, Kember RL, Nunez YZ, Sherva RM, et al. Association of OPRM1 Functional Coding Variant With Opioid Use Disorder: A Genome-Wide Association Study. JAMA Psychiatry. 2020;77:1072–80.
Sweeting M, De Angelis D, Ades A, Hickman M. Estimating the prevalence of ex-injecting drug use in the population. Stat Methods Med Res. 2009;18:381–95.
Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hajebi A, Radgoodarzi R, Mojtabai R, et al. Epidemiology of illicit drug use disorders in Iran: prevalence, correlates, comorbidity and service utilization results from the Iranian Mental Health Survey. Addiction. 2016;111:1836–47.
Santiago Rivera OJ, Havens JR, Parker MA, Anthony JC. Risk of Heroin Dependence in Newly Incident Heroin Users. JAMA Psychiatry. 2018;75:863–4.
Frei O, Holland D, Smeland OB, Shadrin AA, Fan CC, Maeland S, et al. Bivariate causal mixture model quantifies polygenic overlap between complex traits beyond genetic correlation. Nat Commun. 2019;10:2417.
Rosoff DB, Smith GD, Lohoff FW. Prescription Opioid Use and Risk for Major Depressive Disorder and Anxiety and Stress-Related Disorders: A Multivariable Mendelian Randomization Analysis. JAMA Psychiatry. 2021;78:151–60.
Andrews SJ, Fulton-Howard B, O’Reilly P, Marcora E, Goate AM, collaborators of the Alzheimer’s Disease Genetics C. Causal Associations Between Modifiable Risk Factors and the Alzheimer’s Phenome. Ann Neurol. 2021;89:54–65.
McClelland KI, Davies TH. Understanding Links among Opioid Use, Overdose, and Suicide. N Engl J Med. 2019;380:1379–80.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Reich D, Price AL, Patterson N. Principal component analysis of genetic data. Nat Genet. 2008;40:491–2.
Manichaikul A, Mychaleckyj JC, Rich SS, Daly K, Sale M, Chen WM. Robust relationship inference in genome-wide association studies. Bioinformatics. 2010;26:2867–73.
Erlangsen A, Appadurai V, Wang Y, Turecki G, Mors O, Werge T, et al. Genetics of suicide attempts in individuals with and without mental disorders: a population-based genome-wide association study. Mol Psychiatry. 2020;25:2410–21.
Colbert SMC, Hatoum AS, Shabalin A, Li QS, Coon H, Nelson EC, et al. Exploring the genetic overlap of suicide-related behaviors and substance use disorders. Am J Med Genet B Neuropsychiatr Genet. 2021;186:445–55.
Zhu Z, Zheng Z, Zhang F, Wu Y, Trzaskowski M, Maier R, et al. Causal associations between risk factors and common diseases inferred from GWAS summary data. Nat Commun. 2018;9:224.
Volkow ND, Jones EB, Einstein EB, Wargo EM. Prevention and Treatment of Opioid Misuse and Addiction: A Review. JAMA Psychiatry. 2019;76:208–16.
Polimanti R, Walters RK, Johnson EC, McClintick JN, Adkins AE, Adkins DE, et al. Leveraging genome-wide data to investigate differences between opioid use vs. opioid dependence in 41,176 individuals from the Psychiatric Genomics Consortium. Mol Psychiatry. 2020;25:1673–87.
Howard DM, Adams MJ, Clarke TK, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci. 2019;22:343–52.
International HapMap C. The International HapMap Project. Nature. 2003;426:789–96.
Choi SW, O’Reilly PF. PRSice-2: Polygenic Risk Score software for biobank-scale data. Gigascience. 2019;8:giz082.
Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet. 2006;38:904–9.
Coombes BJ, Ploner A, Bergen SE, Biernacka JM. A principal component approach to improve association testing with polygenic risk scores. Genet Epidemiol. 2020;44:676–86.
Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc Ser B (Methodol). 1995;57:289–300.
Brion MJ, Shakhbazov K, Visscher PM. Calculating statistical power in Mendelian randomization studies. Int J Epidemiol. 2013;42:1497–501.
Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat Commun. 2017;8:1826.
Bulik-Sullivan BK, Loh PR, Finucane HK, Ripke S, Yang J, Schizophrenia Working Group of the Psychiatric Genomics C. et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015;47:291–5.
Macfarlane GJ, Beasley M, Jones GT, Stannard C. The epidemiology of regular opioid use and its association with mortality: Prospective cohort study of 466 486 UK biobank participants. EClinicalMedicine. 2020;21:100321.
Wilkins NJ, Clayton H, Jones CM, Brown M. Current Prescription Opioid Misuse and Suicide Risk Behaviors Among High School Students. Pediatrics. 2021;147:e2020030601.
Mullins N, Bigdeli TB, Borglum AD, Coleman JRI, Demontis D, Mehta D, et al. GWAS of Suicide Attempt in Psychiatric Disorders and Association With Major Depression Polygenic Risk Scores. Am J Psychiatry. 2019;176:651–60.
Miller JN, Black DW. Bipolar Disorder and Suicide: a Review. Curr Psychiatry Rep. 2020;22:6.
Willsey AJ, Morris MT, Wang S, Willsey HR, Sun N, Teerikorpi N, et al. The Psychiatric Cell Map Initiative: A Convergent Systems Biological Approach to Illuminating Key Molecular Pathways in Neuropsychiatric Disorders. Cell. 2018;174:505–20.
Sokolowski M, Wasserman D. Genetic origins of suicidality? A synopsis of genes in suicidal behaviours, with regard to evidence diversity, disorder specificity and neurodevelopmental brain transcriptomics. Eur Neuropsychopharmacol. 2020;37:1–11.
Mann JJ, Rizk MM. A Brain-Centric Model of Suicidal Behavior. Am J Psychiatry. 2020;177:902–16.
Sullivan PF, Agrawal A, Bulik CM, Andreassen OA, Borglum AD, Breen G, et al. Psychiatric Genomics: An Update and an Agenda. Am J Psychiatry. 2018;175:15–27.
Yang J, Lee SH, Goddard ME, Visscher PM. GCTA: a tool for genome-wide complex trait analysis. Am J Hum Genet. 2011;88:76–82.
Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47:1236–41.
Sanderson E, Davey Smith G, Windmeijer F, Bowden J. An examination of multivariable Mendelian randomization in the single-sample and two-sample summary data settings. Int J Epidemiol. 2019;48:713–27.
O’Loughlin J, Casanova F, Jones SE, Hagenaars SP, Beaumont RN, Freathy RM, et al. Using Mendelian Randomisation methods to understand whether diurnal preference is causally related to mental health. Mol Psychiatry. 2021;26:6305–16.
Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–9.
Ackerman JP, McBee-Strayer SM, Mendoza K, Stevens J, Sheftall AH, Campo JV, et al. Risk-sensitive decision-making deficit in adolescent suicide attempters. J Child Adolesc Psychopharmacol. 2015;25:109–13.
Bridge JA, Reynolds B, McBee-Strayer SM, Sheftall AH, Ackerman J, Stevens J, et al. Impulsive aggression, delay discounting, and adolescent suicide attempts: effects of current psychotropic medication use and family history of suicidal behavior. J Child Adolesc Psychopharmacol. 2015;25:114–23.
Lutz PE, Courtet P, Calati R. The opioid system and the social brain: implications for depression and suicide. J Neurosci Res. 2020;98:588–600.
Gustafsson PE, Linander I, Mosquera PA. Embodying pervasive discrimination: a decomposition of sexual orientation inequalities in health in a population-based cross-sectional study in Northern Sweden. Int J Equity Health. 2017;16:22.
Anestis MD, Soberay KA, Gutierrez PM, Hernandez TD, Joiner TE. Reconsidering the link between impulsivity and suicidal behavior. Pers Soc Psychol Rev. 2014;18:366–86.
Kang S, Nakanishi Y, Kioi Y, Okuzaki D, Kimura T, Takamatsu H, et al. Semaphorin 6D reverse signaling controls macrophage lipid metabolism and anti-inflammatory polarization. Nat Immunol. 2018;19:561–70.
Biernacki MA, Foster KA, Woodward KB, Coon ME, Cummings C, Cunningham TM, et al. CBFB-MYH11 fusion neoantigen enables T cell recognition and killing of acute myeloid leukemia. J Clin Invest. 2020;130:5127–41.
Forrest MP, Hill MJ, Quantock AJ, Martin-Rendon E, Blake DJ. The emerging roles of TCF4 in disease and development. Trends Mol Med. 2014;20:322–31.
Zeng J, Wang Y, Luo Z, Chang LC, Yoo JS, Yan H, et al. TRIM9-Mediated Resolution of Neuroinflammation Confers Neuroprotection upon Ischemic Stroke in Mice. Cell Rep. 2019;27:549–560.e546
Millner AJ, Lee MD, Hoyt K, Buckholtz JW, Auerbach RP, Nock MK. Are suicide attempters more impulsive than suicide ideators? Gen Hosp Psychiatry. 2020;63:103–10.
Beurel E, Jope RS. Inflammation and lithium: clues to mechanisms contributing to suicide-linked traits. Transl Psychiatry. 2014;4:e488.
Romero C, Werme J, Jansen PR, Gelernter J, Stein MB, Levey D, et al. Exploring the genetic overlap between twelve psychiatric disorders. Nat Genet. 2022;54:1795–802.
Trubetskoy V, Pardinas AF, Qi T, Panagiotaropoulou G, Awasthi S, Bigdeli TB, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. 2022;604:502–8.
Mullins N, Forstner AJ, O’Connell KS, Coombes B, Coleman JRI, Qiao Z, et al. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet. 2021;53:817–29.
Deak JD, Zhou H, Galimberti M, Levey DF, Wendt FR, Sanchez-Roige S, et al. Genome-wide association study in individuals of European and African ancestry and multi-trait analysis of opioid use disorder identifies 19 independent genome-wide significant risk loci. Mol Psychiatry. 2022;27:3970–9.
Lee PH, Feng YA, Smoller JW. Pleiotropy and Cross-Disorder Genetics Among Psychiatric Disorders. Biol Psychiatry. 2021;89:20–31.
Sullivan MD, Howe CQ. Opioid therapy for chronic pain in the United States: promises and perils. Pain. 2013;154:S94–S100.
Denny JC, Collins FS. Precision medicine in 2030-seven ways to transform healthcare. Cell. 2021;184:1415–9.
Holmes MV, Ala-Korpela M, Smith GD. Mendelian randomization in cardiometabolic disease: challenges in evaluating causality. Nat Rev Cardiol. 2017;14:577–90.
Richesson RL, Marsolo KS, Douthit BJ, Staman K, Ho PM, Dailey D, et al. Enhancing the use of EHR systems for pragmatic embedded research: lessons from the NIH Health Care Systems Research Collaboratory. J Am Med Inf Assoc. 2021;28:2626–40.
Acknowledgements
This research was made possible by previous studies from PGC, MVP, iPSYCH, the developers of the MRC-IEU UK Biobank, and researchers from ISGC (especially Dr. Niamh Mullins), who provided the latest European-ancestry statistics on SA. We acknowledge their contributing studies and the participants in those studies, without whom this effort would not be possible. We thank Dr. Lisa Matero for providing insights on clinical implication of this genetic study.
Funding
This study was financially supported by the National Nature Science Foundation of China (Grant NO.82171499 to QW), Science and Technology Project of Sichuan Province (2023YFS0030 to QW) and Chinese National Programs for Brain Science and Brain-like Intelligence Technology-China Depression Cohort Study (2021ZD0200700 to QW). BKA is supported by NIH Award (OT2OD026550). HG is supported by Mentored Scientist Grant in Henry Ford Health (A20067). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
QW and HG have full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analyses. Concept and design: All authors. Acquisition, analysis, or interpretation of data: YH, DC, QW, HG. Drafting of the manuscript: YH, QW, HG. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: YH, DC, ML, QW, HG. Obtained funding: QW, HG. Administrative, technical, or material support: QW, HG. Supervision: QW, HG, PCS.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the statement in the Funding information section was incorrectly given as ‘This study was financially supported by the National Nature Science Foundation of China (Grant No. 81771446 to QW)’ and should have read ‘This study was financially supported by the National Nature Science Foundation of China (Grant No. 82171499 to QW and No. 81771446 to QW)’.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, Y., Chen, D., Levin, A.M. et al. Cross-phenotype relationship between opioid use disorder and suicide attempts: new evidence from polygenic association and Mendelian randomization analyses. Mol Psychiatry 28, 2913–2921 (2023). https://doi.org/10.1038/s41380-023-02124-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02124-w