Abstract
Pre-existing mental disorders are linked to COVID-19-related outcomes. However, the findings are inconsistent and a thorough analysis of a broader spectrum of outcomes such as COVID-19 infection severity, morbidity, and mortality is required. We investigated whether the presence of psychiatric diagnoses and/or the use of antidepressants influenced the severity of the outcome of COVID-19. This retrospective cohort study evaluated electronic health records from the INSIGHT Clinical Research Network in 116,498 individuals who were diagnosed with COVID-19 between March 1, 2020, and February 23, 2021. We examined hospitalization, intubation/mechanical ventilation, acute kidney failure, severe sepsis, and death as COVID-19-related outcomes. After using propensity score matching to control for demographics and medical comorbidities, we used contingency tables to assess whether patients with (1) a history of psychiatric disorders were at higher risk of more severe COVID-19-related outcomes and (2) if use of antidepressants decreased the risk of more severe COVID-19 infection. Pre-existing psychiatric disorders were associated with an increased risk for hospitalization, and subsequent outcomes such as acute kidney failure and severe sepsis, including an increased risk of death in patients with schizophrenia spectrum disorders or bipolar disorders. The use of antidepressants was associated with significantly reduced risk of sepsis (p = 0.033), death (p = 0.026). Psychiatric disorder diagnosis prior to a COVID-19-related healthcare encounter increased the risk of more severe COVID-19-related outcomes as well as subsequent health complications. However, there are indications that the use of antidepressants might decrease this risk. This may have significant implications for the treatment and prognosis of patients with COVID-19.
Similar content being viewed by others
Introduction
Adverse mental health effects of the COVID-19 pandemic were emphasized early in the pandemic [1,2,3,4,5], whereas there is no consistent evidence on how preexisting mental disorders might influence COVID-19-related outcomes [6]. Schizophrenia spectrum disorders have been associated with an increased risk for mortality in patients with COVID-19 compared to anxiety or depression disorders [7,8,9], although mood disorders and sleep disturbances may also be associated with illness severity [10]. In addition, pre-existing mood, and attention-deficit hyperactivity disorders have been reported to increase the susceptibility of contracting COVID-19 [10, 11]. However, several meta-analyses and reviews tempered the impact of pre-existing psychiatric disorders on susceptibility of contracting COVID-19, but reported that pre-existing psychiatric disorders might be associated with increased risk for hospitalization and death after COVID-19 diagnosis [12,13,14]. These inconsistent findings limit the opportunity to provide effective and generalizable guidelines, in part because there has not been a clear and consistent definition of “severe” form of COVID-19, making it difficult to interpret these findings. Thus, in some studies, death, ICU admission, or invasive ventilation were considered severe forms of COVID-19 [15], whereas in other studies, hospitalization was considered an index of severity [16].
In addition, some beneficial effects of mental health medications, such as selective serotonin reuptake inhibitors, on the severity of COVID-19 disease outcomes have been recently documented [17]. Among heathy controls, such antidepressants have been suggested to have immune-modulatory effects, inhibiting the inflammatory response and reducing lung tissue damage [18]. However, findings were mixed regarding protective effects of antidepressants on COVID-19 infection and/or outcomes [19]. Given the frequency of psychotropic drug use in patients with preexisting psychiatric disorders, it is possible that antidepressants are an additional factor of importance that should be considered.
Our aim was therefore two-fold. First, we wanted to assess the risk of pre-existing mental disorders on COVID-19 related outcomes, i.e., severity, morbidity, and mortality. Second, we aimed to assess how antidepressants affected this risk among individuals with pre-existing mental disorders. To do so, we conducted a retrospective cohort study using electronic health record (EHR) data from the five largest private healthcare systems in New York City (NYC). NYC was an early epicenter of the COVID-19 pandemic and is characterized by a highly socio-demographically diverse population. We also examined the impact of specific psychiatric diagnoses, such as depression, anxiety disorders, schizophrenia spectrum disorders/bipolar disorders, attention deficit hyperactivity disorder (ADHD), personality disorders, sleep disorders as well as severe stress disorders (such as Post Traumatic Stress Disorder; PTSD). We conducted two separate analyses, including either a) individuals with a recent psychiatric diagnosis (within the year prior to the COVID-19-related encounter) to capture individuals with recent and possibly active psychiatric condition or b) individuals diagnosed anytime between 2011 and 2021.
Method
Study design
This retrospective cohort study used de-identified EHR data from the INSIGHT Clinical Research Network (CRN), which contains EHR data of over 12 million patients in New York City. These data repository was established in response to an initiative of PCORnet’s (National Patient-Centered Clinical Research Network). INSIGHT CRN provides a unique opportunity to study health care utilization and outcomes among patients of all insurance types, both inpatient and outpatient, and across multiple health care systems. We extracted EHR data from the five largest private healthcare systems in New York: Columbia University Irving Medical Center, Montefiore Medical Center, Mount Sinai Health System, NYU Langone Health, and Weill Cornell/NY-Presbyterian Medical Center. This secondary data analysis of de-identified data was exempted by the Columbia University Irving Medical Center and NYU Langone Health Institutional Review Boards. The preparation of the manuscript followed the statement for strengthening the reporting of observational studies in epidemiology [20].
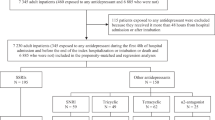
The study sample was limited to individuals who were 18 years and older and who had a COVID-19-related encounter between March 1, 2020, and February 23, 2021 (N = 116,498), defined by a positive reverse transcription-polymerase chain reaction (PCR) or the presence of at least one of the ICD codes shown in Supplementary Table 1.
Primary exposure
We defined patients with a pre-existing psychiatric disorder if they were diagnosed either a) in the year prior to the COVID-19 encounter or b) anytime between 2011 and 2021. We examined the impact of depression, anxiety, stress-related disorders, ADHD, schizophrenia spectrum disorders/bipolar disorders, personality disorders, and sleep disorders on COVID-19 related outcomes. To ensure readability, only the results related to the impact of a recent diagnosis (in the past year) will be presented in the main text and the results regarding the impact of psychiatric disorders diagnosed between 2011 and 2021 are presented in the Supplementary Information. Psychiatric diagnoses were classified into mutually exclusive diagnostic categories based on the International Statistical Classification of Diseases, Tenth Revision. Details on the included ICD-10 codes for each condition can be found in Supplementary Table 2.
Primary outcomes
We examined five COVID-19-related outcomes of severity, morbidity, and mortality: inpatient hospitalization (defined as any hospital admission during a COVID-19 encounter), intubation/mechanical ventilation, kidney failure, sepsis, and death. Because early readmissions after COVID-19 are common, death was defined as mortality experienced during a COVID-19 encounter, hospital stay or within 14 days after discharge from a COVID-19 encounter [21]. Furthermore, we examined subsequent medical sequelae, i.e., acute kidney failure and severe sepsis or septic shock within 28 days of a COVID-19 encounter. Hospitalization and intubation/mechanical ventilation were considered indicators of COVID-19-related severity, acute kidney failure and severe sepsis indicators of COVID-19-related morbidity, and death after a COVID-19 diagnosis as representative of COVID-19-related mortality. Not all included subjects with a COVID-19 diagnosis experienced a serious outcome, defined as hospitalization, intubation/mechanical ventilation, kidney failure, sepsis, and death, as shown in Table 1.
Demographic characteristics and medical comorbidities
We assessed the association of demographic characteristics and the presence of medical comorbidities from 2011 until 2021, which have been shown to increase the risk of more severe COVID-10 outcomes [22, 23].
We examined sex (male/female), age (0–17 years, 18–44 years, 45–64 years, 65–74 years, and 75 years and older), and race/ethnicity (non-Hispanic white, non-Hispanic Black, Hispanic/Latino, Asian/Pacific Islander, other/multiracial, and refused/missing) as relevant demographic characteristics. The category “other/multi-racial” included patients for whom race/ethnicity was coded as American Indian or Alaska Native, multiracial, or other.
Furthermore, we examined the following medical comorbidities, informed by prior research on COVID-19-related risk factors for mortality and morbidity: [7, 9, 10] cardiovascular disorders (including heart failure, acute myocardial infarction, congestive heart failure, ischemic heart disease, and cardiac dysrhythmia); chronic kidney disease; pain disorders (including chronic pain, chronic fatigue, fibromyalgia, and post-viral fatigue); diabetes; obesity; and respiratory disorders (including emphysema, chronic obstructive pulmonary disease, and asthma). The respective ICD-9 and ICD-10 codes can be found in the Supplementary Table 3 and a list of the examined antidepressant medication can be found in Supplementary Table 4.
Statistical analysis
We used propensity score matching analysis to match our cohort of patients with pre-existing psychiatric disorders, either in the year prior to the COVID encounter or from 2011-2021, with patients without pre-existing psychiatric disorders using demographic characteristics and medical comorbidities listed above. Each psychiatric disorder was modeled separately. The entire pool of participants without pre-existing psychiatry disorders was always considered in the matching process. To illustrate the process, we use an example where the psychiatric disorder of interest is depression, and the outcome is whether a person was hospitalized following their COVID encounter. The propensity score was calculated using logistic regression implemented by the function LogisticRegression using scikit-learn (version 1.0.1). In our example, we would fit a logistic regression model to fit demographic/medical comorbidity variables to the presence of a psychological disorder, i.e., depression. A nearest neighbor search was performed using scikit-learn to identify matching candidates. A caliper of 1/4th the standard deviation of the logit propensity score was used to assure that the matched candidates were suitably similar to each other [24,25,26]. Note that the matching was not unique with respect to the candidates for matching (i.e., non-depressed group in the example); this was done to ensure robustness in matching of individuals with rare demographic/comorbidity presentation. A K = 10 nearest neighbors algorithm with a radius equal to the caliper and Euclidean distance metric was fit to the data frame logit propensity score columns. Returning to the example, individuals would be matched to another individual who belongs to the opposite group (depressed vs non-depressed) with the nearest probability of presenting the psychiatric disorder, based on the logistic regression model using their demographic/comorbidity characteristics. After the cohort of interest and their respective matched pairs were calculated (in this step, all individuals below 18 were excluded), a 2 by 2 contingency table of the groups (depressed vs non-depressed) versus the outcome indicator (a variable denoting if an individual was ever hospitalized during a COVID encounter) was constructed. Using the statsmodels (version 0.10.1) contingency table summary function, the odds ratios for this contingency table were calculated [27]. To illustrate the impact of such analytical plan, we first report the unadjusted results, i.e., the odds ratios before propensity matching, to compare with the adjusted results.
The same procedure was used to compare our cohort of patients with preexisting psychiatric disorders who were taking antidepressants at the time of the COVID-19 encounter with patients with preexisting psychiatric disorders and not taking such medications based on demographic characteristics and medical comorbidities.
The number of patients included in each comparison to compute the odds ratios after the propensity score matching can be found in Supplementary Table 5. All analyses were conducted using Python version 3.7.4.
Results
Descriptive statistics on the sample characteristics are presented in Table 1. 14,486 individuals were diagnosed with a recent psychiatric diagnosis and 19,407 individuals were diagnosed with a psychiatric disorder between 2011 and 2021. We identified a total of 19,093 recent psychiatric diagnoses within the year prior to the COVID-19 encounter. 32.9% (N = 6290) were depressive disorders, 33% (N = 6305) sleep disorders, 10.1% (N = 1934) anxiety disorders, 2.7% (N = 514) severe stress disorders, 10.2% (N = 1932) schizophrenia spectrum disorders /bipolar disorders, 10% (N = 1906) ADHD and 1.1% (N = 212) personality disorders diagnoses.
Prior to adjusting for demographic characteristic and medical comorbidities, patients with psychiatric diagnoses in the past year had significantly higher risk of every COVID-19 outcome (hospitalization, intubation/mechanical ventilation, acute kidney failure, severe sepsis, and death). Even after adjusting for demographic characteristics and medical comorbidities, we found that being diagnosed with a psychiatric disorder in the year prior to COVID-19 diagnosis was associated with an increased risk for COVID-19-related hospitalization and acute kidney failure (Table 2).
Nearly all past psychiatric conditions were associated with an increased risk of being hospitalized during a COVID-19 encounter (Table 3). Individuals with sleep disorders were the only group of patients with preexisting psychiatric conditions who were not at increased risk of being hospitalized during a COVID-19-related encounter. A diagnosis of schizophrenia spectrum disorders/ bipolar disorder was associated with the highest likelihood of being hospitalized, suffering from acute kidney failure or severe sepsis, or dying after a COVID-19 encounter.
Concurrent antidepressant use among individuals with a psychiatric disorder during a hospital admission was a protective factor against sepsis and death (Table 2).
Results for the impact of psychiatric disorders diagnosed between 2011 and 2021 are presented Supplementary Table 6–8.
Discussion
In this retrospective cohort study of 116,498 patients with confirmed COVID-19 diagnosis, psychiatric disorders within the year prior to the COVID-19 encounter were associated with an increased risk of hospitalization and subsequent outcomes such as acute kidney failure, intubation/mechanical ventilation, and severe sepsis after controlling for demographic variables and medical comorbidities.
Through careful propensity score matching, we intended to isolate the effect of a preexisting psychiatric disorder on well-defined COVID-19 outcomes. This helped us account for an important limitation pointed out in a recent meta-analysis of the confounding effect of medical comorbidities in assessing the potential vulnerability of psychiatric populations to COVID-19 outcomes [7].
First, almost all preexisting psychiatric disorders within the past year represented an increased risk for hospitalization, except for sleep disorders. This was also the case for most of the psychiatric disorders diagnosed between 2011 and 2021, such as anxiety, depression, ADHD, personality disorders, reaction to stress, and schizophrenia spectrum disorders/bipolar disorders. However, with the exception of bipolar disorder, we did not find an association between the other mood-related psychiatric diagnoses and increased risk of death compared with previous studies [13].
Second, we highlighted that patients suffering from schizophrenia spectrum disorders /bipolar disorder were at the highest risk for severity (hospitalization), morbidity (acute kidney failure and severe sepsis), and death. This corroborates previous findings, which also reported an increased risk of mortality associated with schizophrenia diagnosis [7,8,9, 28] and bipolar disorder [16]. The fact that this effect remained significant even after adjusting for demographic and medical comorbidities further supports the independent effect that psychiatric disorders may have on COVID-19 morbidity. This is in contrast to some authors suggestions that the increased risk of COVID-19-related mortality among individuals with psychiatric disorders may be explained by the greater number of other medical comorbidities in this population, but not by the underlying psychiatric disorder [29].
A combination of potential delays in treatment-seeking, reduced access to care, biological factors related to their psychiatric illness or treatment, and immune dysregulation have been hypothesized as possible contributors to the association between psychiatric disorders and worse COVID-19 outcome [7]. While the underlying reason for this association remains unclear, the hypothesis that a pre-existing psychiatric disorder may influence the susceptibility and/or severity of infectious diseases (including respiratory virus infections) has been discussed for a longer time [30,31,32]. It has been discussed whether psychiatric disorders could also be associated with an elevated risk of COVID-19, possibly through similar mechanisms as those leading to other infections [33]. Specifically, previous stressors may enhance neuroimmune signaling, leading to elevated symptoms of fatigue following an inflammatory stimulus [34, 35].
Interestingly, a recent systematic review and meta-analysis described that preexisting psychiatric disorders not only increase the likelihood of severe COVID-19-related outcomes, but may also be associated with an increased risk of developing mental health outcomes after COVID-19 infection [36].
Third, we observed a protective effect of the use of antidepressant medication during the COVID-19 encounter among individuals with psychiatric diagnoses on multiple outcomes (sepsis, death and on a trend level intubation/mechanical ventilation). Our results corroborate and deepen previous cohort studies which showed that antidepressants were associated with less severe outcomes as they significantly reduced the risk of intubation or death [18, 19]. We performed a direct comparison of the sole impact of psychiatric disorders on COVID-19 outcome, and in a second step the effect of antidepressant medication on those outcomes. However, the specific mechanisms of action (i.e., serotonin transporter, sigma-1 receptor, and acid sphingomyelinase) of antidepressant on COVID-19 could be multiple and are not defined yet [37]. Through a variety of processes, a potential anti-inflammatory effect of these drugs has been hypothesized [38, 39].
Strengths and limitations
INSIGHT aggregated EHR from the five largest private hospital systems in NYC serving diverse patient populations, which strengthens the generalizability of our findings. We used propensity score matching to control for the influence of demographic information and medical comorbidities. Furthermore, we included a broad range of psychiatric conditions, examined different observation periods, and examined the impact of antidepressant medication on COVID-19 severity, morbidity, and mortality. Because this is an observational study and EHR data were analyzed, the presence of information may be biased because patients with greater access to care and contact with a particular healthcare system will have more complete medical records. No information was available on health insurance status or other proxies for social determinants of health, such as socioeconomic status, to examine their potential impact. Furthermore, individuals with psychiatric disorders may be less likely to seek medical care, particularly if there are systemic barriers to accessing care. In addition, EHR data is not collected for research purposes, rather for clinical and billing purposes. This could be challenging because psychiatric diagnoses are based on patient reports and clinician observations that may not be well captured in billing codes. Moreover, we did not have access to data from the NYC public hospital system, and thus the data is not representative of the NYC population as a whole. For instance, the obesity rates observed in this study are lower than those previously reported in the US/New York (10% compared to 27.6% according to the New York State Behavioral Risk Factor Surveillance System [40]).
Other possible limitations are that the accuracy of clinical psychiatric diagnoses is solely extracted from the EHR and cannot be validated. Systematic coding of diagnoses has been shown to improve only in recent years [41] as EMRs have become more widely used, and more slowly in mental health care than in other medical settings [42]. This may be due to concerns about the collection of sensitive information, standardization of mental health data, and the risk of negatively impacting therapeutic relationships [43]. In addition, to maximize the sample, we classified some psychiatric disorders into broad categories that may have within-category differences in the risk associated with particular diagnoses.
Furthermore, it should be noted that we examined COVID-19-related outcomes over a period when medical knowledge about the treatment of COVID-19 has changed over time. Unfortunately, we do not have access to information on different strains/subtypes of the virus or potential superimposed acute conditions that could affect COVID-19 outcomes. Although our study design should reduce the potential impact of such aspects, we cannot exclude a possible impact even though we studied COVID-19-related outcomes in a large cohort and over a long period of time. Lastly, since NYC was an early epicenter of the COVID-19 pandemic, PCR testing was not widely available at that time. To avoid sampling bias and include all relevant subjects, participants were required to have a positive PCR test or at least one of the ICD codes described in Supplementary Table 1.
Conclusion
The results of the present study suggest that individuals with pre-existing psychiatric disorders (both recent and long-standing) may be more susceptible to severe forms of COVID-19 outcomes even after carefully controlling for relevant demographic characteristics and medical comorbidities. However, there is evidence that the use of antidepressants may reduce this risk. We were able to corroborate and extend previous findings by examining the impact of antidepressant medication intake in this population. Targeted early interventions to prevent medical complications such as acute kidney failure, or severe sepsis might should be considered for this vulnerable population.
References
Brooks SK. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–20.
Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51:201–11.
Sacco DL, Probst MA, Schultebraucks K, Greene MC, Chang BP. Evaluation of emergency department visits for mental health complaints during the COVID‐19 pandemic. J Am Coll Emerg Physicians Open. 2022;3:12728.
Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383:510–2.
Santomauro DF. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–12.
De Hert M, Mazereel V, Stroobants M, De Picker L, Van Assche K, Detraux J. COVID-19-related mortality risk in people with severe mental illness: a systematic and critical review. Front Psychiatry. 2022;12:798554.
Ceban F, Nogo D, Carvalho IP, Lee Y, Nasri F, Xiong J, et al. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78:1079.
Maripuu M, Bendix M, Öhlund L, Widerström M, Werneke U. Death associated with coronavirus (COVID-19) infection in individuals with severe mental disorders in Sweden during the early months of the outbreak—an exploratory cross-sectional analysis of a population-based register study. Front Psychiatry. 2021;11:609579.
Vai B, Mazza MG, Delli Colli C, Foiselle M, Allen B, Benedetti F, et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8:797–812.
Liu L, Ni S-Y, Yan W, Lu Q-D, Zhao Y-M, Xu Y-Y, et al. Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: a systematic review, meta-analysis and call for action. eClinicalMedicine. 2021;40:101111.
Dai X, Shao Y, Ren L, Tao W, Wang Y. Risk factors of COVID-19 in subjects with and without mental disorders. J Affect Disord. 2022;297:102–11.
Barcella CA, Polcwiartek C, Mohr GH. Severe mental illness is associated with increased mortality and severe course of COVID-19. Acta Psychiatr Scand. 2021;144:82–91.
Toubasi AA, AbuAnzeh RB, Tawileh HBA. A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. 2021;299:113856.
Chen S, Fernandez-Egea E, Jones PB. Longer-term mortality following SARS-CoV-2 infection in people with severe mental illness: retrospective case-matched study. BJPsych Open. 2021;7:e201.
Lee SW, Yang JM, Moon SY, Yoo IK, Ha EK, Kim SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020;7:1025–31.
Luykx JJ, Lin BD. Are psychiatric disorders risk factors for COVID-19 susceptibility and severity? a two-sample, bidirectional, univariable, and multivariable Mendelian Randomization study. Transl Psychiatry. 2021;11:210.
Nakhaee H, Bayati R, Rahmanian M, Jolfayi AG, Zangiabadian M, Rakhshanderou S. The effect of antidepressants on severity of COVID-19 in hospitalized patients: a systematic review and meta-analysis. Psychiatry Clin Psychol. 2022;17:e0267423.
Hoertel N, Sánchez-Rico M, Vernet R, Beeker N, Jannot A-S, Neuraz A, et al. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Mol Psychiatry. 2021;26:5199–212.
Diez‐Quevedo C, Iglesias‐González M, Giralt‐López M, Rangil T, Sanagustin D, Moreira M, et al. Mental disorders, psychopharmacological treatments, and mortality in 2150 COVID‐19 Spanish inpatients. Acta Psychiatr Scand. 2021;143:526–34.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7.
Huang C-W. Disease-specific factors associated with readmissions or mortality after hospital discharge in COVID-19 patients: a retrospective cohort study. J Gen Intern Med. 2022;37:3973–8.
Gao Y, Ding M, Dong X, Zhang J, Kursat Azkur A, Azkur D, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy 2021;76:428–55.
Li J, Huang DQ, Zou B, Yang H, Hui WZ, Rui F, et al. Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J Med Virol. 2021;93:1449–58.
Lunt M. Selecting an appropriate caliper can be essential for achieving good balance with propensity score matching. Am J Epidemiol. 2014;179:226–35.
Cochran WG, Rubin DB. Controlling bias in observational studies: a review. Sankhyā. Indian J Stat. 1973;Series A, 35:417–46.
Austin PC. Optimal caliper widths for propensity‐score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Pirracchio R, Resche-Rigon M, Chevret S. Evaluation of the Propensity score methods for estimating marginal odds ratios in case of small sample size. BMC Med Res Methodol. 2012;12:70.
Nemani K, Li C, Olfson M, Blessing EM, Razavian N, Chen J, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78:380.
Hoertel N, Sánchez-Rico M, de la Muela P, Abellán M, Blanco C, Leboyer M, et al. Risk of death in individuals hospitalized for COVID-19 with and without psychiatric disorders: an observational multicenter study in France. Biol Psychiatry Glob Open Sci. 2022;3:56–67.
Müller N. Infectious diseases and mental health. Comorb Ment Phys Disord. 2014;179:99–113.
Maalouf O, Daigneault I, Dargan S, McDuff P, Frappier JY. Relationship between child sexual abuse, psychiatric disorders and infectious diseases: a matched-cohort study. J Child Sex Abus. 2020;29:749–68.
Song H, Fall K, Fang F, Erlendsdóttir H, Lu D, Mataix-Cols D, et al. Stress related disorders and subsequent risk of life threatening infections: population based sibling controlled cohort study. BMJ. 2019;367:5784.
Yang H, Chen W, Hu Y, Chen Y, Zeng Y, Sun Y, et al. Pre-pandemic psychiatric disorders and risk of COVID-19: a UK Biobank cohort analysis. Lancet Healthy Longev. 2020;1:e69–e79.
Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc Natl Acad Sci USA 2003;100:9090–5.
Miller GE, Chen E, Sze J, Marin T, Arevalo JMG, Doll R, et al. A functional genomic fingerprint of chronic stress in humans: blunted glucocorticoid and increased NF-κB signaling. Biol Psychiatry. 2008;64:266–72.
Yuan K. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. 2022;27:1–9.
Hashimoto Y, Suzuki T, Hashimoto K. Mechanisms of action of fluvoxamine for COVID-19: a historical review. Mol Psychiatry. 2021;27:1898–907.
Meikle CKS, Creeden JF, McCullumsmith C, Worth RG. SSRIs: applications in inflammatory lung disease and implications for COVID‐19. Neuropsychopharmacol Rep. 2021;41:325–35.
Hamed MGM, Hagag RS. The possible immunoregulatory and anti-inflammatory effects of selective serotonin reuptake inhibitors in coronavirus disease patients. Med Hypotheses. 2020;144:110140.
New York State Behavioral Risk Factor Surveillance System. Prevalence of obesity among New York State Adults by county, BRFSS 2018. Centers for Disease Control and Prevention (CDC); 2021.
Smoller JW. The use of electronic health records for psychiatric phenotyping and genomics. Am J Med Genet Part B: Neuropsychiatr Genet. 2018;177:601–12.
Zurynski Y. Implementation of electronic medical records in mental health settings: scoping review. JMIR Ment Health. 2021;8:30564.
Kariotis TC, Prictor M, Chang S, Gray K. Impact of electronic health records on information practices in mental health contexts: scoping review. J Med Internet Res. 2022;24:30405.
Acknowledgements
This work was conducted through use of data from the INSIGHT Clinical Research Network and supported in-part by the Patient-Centered Outcomes Research Institute (PCORI) PCORnet grant to the INSIGHT Clinical Research Network (grant # RI-CRN-2020-004).
Author information
Authors and Affiliations
Contributions
KS, BFH, NK, BA, CA, BDR, HAL, DMM, and FRL substantially contributed to the design of the study and developed the study concept. KS, WB, CB, TC, and ZK developed the data analytical plan and performed data analysis. KS wrote the first draft of the manuscript and all co-authors reviewed and revised the manuscript critically for important intellectual content. All co-authors approved the version of the manuscript to be published.
Corresponding author
Ethics declarations
Competing interests
This publication was supported by the National Center for Advancing Translational Sciences (UL1TR001873). KSs received support from the National Institute of Mental Health (R01MH129856) and the National Heart, Lung, and Blood Institute (R01HL156134). BA received support from the National Institute on Drug Abuse (T32 DA007233). BFH received support from the National Institute on Drug Abuse (T32DA037801). FRL receives grant support from the NIDA, NCATS, SAMHSA, US World Meds and research support from Aelis Pharmaceuticals. She also receives medication from Indivior for research and royalties from APA publishing. In addition, FRL served as a nonpaid member of a Scientific Advisory Board for Alkermes, Indivior, Novartis, Teva, and US WorldMeds and is a consultant to Major League Baseball. DM received support from the National Institute on Drug Abuse (K24 DA050087). HAP is employed by Columbia University, New York State Office of Mental Health/Research, Foundation for Mental Hygiene, and RAND Corporation (Adjunct Staff). All research and training projects funded by not for profit or public sources. He has served on clinical advisory committees for AbleTo, Cerebral and Magellan Studio. NK is involved in ongoing opioid litigation. All other authors report no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schultebraucks, K., Blekic, W., Basaraba, C. et al. The impact of preexisting psychiatric disorders and antidepressant use on COVID-19 related outcomes: a multicenter study. Mol Psychiatry 28, 2462–2468 (2023). https://doi.org/10.1038/s41380-023-02049-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02049-4