Abstract
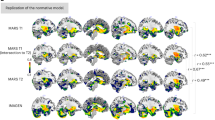
Childhood maltreatment is a leading risk factor for psychopathology, though it is unclear why some develop risk averse disorders, such as anxiety and depression, and others risk-taking disorders including substance abuse. A critical question is whether the consequences of maltreatment depend on the number of different types of maltreatment experienced at any time during childhood or whether there are sensitive periods when exposure to particular types of maltreatment at specific ages exert maximal effects. Retrospective information on severity of exposure to ten types of maltreatment during each year of childhood was collected using the Maltreatment and Abuse Chronology of Exposure scale. Artificial Intelligence predictive analytics were used to delineate the most important type/time risk factors. BOLD activation fMRI response to threatening versus neutral facial images was assessed in key components of the threat detection system (i.e., amygdala, hippocampus, anterior cingulate, inferior frontal gyrus and ventromedial and dorsomedial prefrontal cortices) in 202 healthy, unmedicated, participants (84 M/118 F, 23.2 ± 1.7 years old). Emotional maltreatment during teenage years was associated with hyperactive response to threat whereas early childhood exposure, primarily to witnessing violence and peer physical bullying, was associated with an opposite pattern of greater activation to neutral than fearful faces in all regions. These findings strongly suggest that corticolimbic regions have two different sensitive period windows of enhanced plasticity when maltreatment can exert opposite effects on function. Maltreatment needs to be viewed from a developmental perspective in order to fully comprehend its enduring neurobiological and clinical consequences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All anonymized data used in these analyses have been deposited on Zenodo (https://doi.org/10.5281/zenodo. 5271714 and zenodo.7340449) and are open source.
Code availability
The R code for determining significant type/time risk factors using random forest regression with conditional inference trees has been deposited on Zenodo (https://doi.org/10.5281/zenodo.5273055) and made open source as has the R code used to generate the supplementary tables (https://doi.org/10.5281/zenodo.7340449). The remaining code is included in the supplement as R Markdown files.
References
Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:113–23.
Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37:268–77.
Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111:564–72.
Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci. 2016;17:652–66.
Teicher MH. Scars that won’t heal: the neurobiology of child abuse. Sci Am. 2002;286:68–75.
Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31:183–91.
Khan A, McCormack HC, Bolger EA, McGreenery CE, Vitaliano G, Polcari A, et al. Childhood maltreatment, depression, and suicidal ideation: critical importance of parental and peer emotional abuse during developmental sensitive periods in males and females. Front Psychiatry. 2015;6:42.
McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–24.
Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. J Abnorm Psychol. 2007;116:176–87.
McLaughlin KA, Sheridan MA, Tibu F, Fox NA, Zeanah CH, Nelson CA 3rd. Causal effects of the early caregiving environment on development of stress response systems in children. Proc Natl Acad Sci USA 2015;112:5637–42.
Schalinski I, Teicher MH, Rockstroh B. Early neglect is a key determinant of adult hair cortisol concentration and is associated with increased vulnerability to trauma in a transdiagnostic sample. Psychoneuroendocrinology. 2019;108:35–42.
Pechtel P, Lyons-Ruth K, Anderson CM, Teicher MH. Sensitive periods of amygdala development: the role of maltreatment in preadolescence. Neuroimage 2014;97:236–44.
Teicher MH, Anderson CM, Ohashi K, Khan A, McGreenery CE, Bolger EA, et al. Differential effects of childhood neglect and abuse during sensitive exposure periods on male and female hippocampus. Neuroimage. 2018;169:443–52.
Herzog JI, Thome J, Demirakca T, Koppe G, Ende G, Lis S, et al. Influence of severity of type and timing of retrospectively reported childhood maltreatment on female amygdala and hippocampal volume. Sci Rep. 2020;10:1903.
Luby JL, Tillman R, Barch DM. Association of timing of adverse childhood experiences and caregiver support with regionally specific brain development in adolescents. JAMA Netw Open. 2019;2:e1911426.
Zhu J, Lowen SB, Anderson CM, Ohashi K, Khan A, Teicher MH. Association of prepubertal and postpubertal exposure to childhood maltreatment with adult amygdala function. JAMA Psychiatry. 2019;76:843–53.
Lyons-Ruth K, Pechtel P, Yoon SA, Anderson CM, Teicher MH. Disorganized attachment in infancy predicts greater amygdala volume in adulthood. Behav Brain Res. 2016;308:83–93.
Lupien SJ, Parent S, Evans AC, Tremblay RE, Zelazo PD, Corbo V, et al. Larger amygdala but no change in hippocampal volume in 10-year-old children exposed to maternal depressive symptomatology since birth. Proc Natl Acad Sci USA 2011;108:14324–9.
Tottenham N, Hare TA, Quinn BT, McCarry TW, Nurse M, Gilhooly T, et al. Prolonged institutional rearing is associated with atypically large amygdala volume and difficulties in emotion regulation. Dev Sci. 2010;13:46–61.
Edmiston EE, Wang F, Mazure CM, Guiney J, Sinha R, Mayes LC, et al. Corticostriatal-limbic gray matter morphology in adolescents with self-reported exposure to childhood maltreatment. Arch Pediatr Adolesc Med. 2011;165:1069–77.
Korgaonkar MS, Antees C, Williams LM, Gatt JM, Bryant RA, Cohen R, et al. Early exposure to traumatic stressors impairs emotional brain circuitry. PLoS One. 2013;8:e75524.
Van Dam NT, Rando K, Potenza MN, Tuit K, Sinha R. Childhood maltreatment, altered limbic neurobiology, and substance use relapse severity via trauma-specific reductions in limbic gray matter volume. JAMA Psychiatry. 2014;71:917–25.
Hanson JL, Nacewicz BM, Sutterer MJ, Cayo AA, Schaefer SM, Rudolph KD, et al. Behavioral problems after early life stress: contributions of the hippocampus and amygdala. Biol Psychiatry. 2015;77:314–23.
Glahn DC, Lovallo WR, Fox PT. Reduced amygdala activation in young adults at high risk of alcoholism: studies from the Oklahoma family health patterns project. Biol Psychiatry. 2007;61:1306–9.
Lozier LM, Cardinale EM, VanMeter JW, Marsh AA. Mediation of the relationship between callous-unemotional traits and proactive aggression by amygdala response to fear among children with conduct problems. JAMA Psychiatry. 2014;71:627–36.
Stein MB, Goldin PR, Sareen J, Zorrilla LT, Brown GG. Increased amygdala activation to angry and contemptuous faces in generalized social phobia. Arch Gen Psychiatry. 2002;59:1027–34.
Tottenham N, Hertzig ME, Gillespie-Lynch K, Gilhooly T, Millner AJ, Casey BJ. Elevated amygdala response to faces and gaze aversion in autism spectrum disorder. Soc Cogn Affect Neurosci. 2014;9:106–17.
Stevens JS, Kim YJ, Galatzer-Levy IR, Reddy R, Ely TD, Nemeroff CB, et al. Amygdala reactivity and anterior cingulate habituation predict posttraumatic stress disorder symptom maintenance after acute civilian trauma. Biol Psychiatry. 2017;81:1023–9.
Garrett AS, Carrion V, Kletter H, Karchemskiy A, Weems CF, Reiss A. Brain activation to facial expressions in youth with PTSD symptoms. Depress Anxiety. 2012;29:449–59.
Zhu J, Lowen SB, Anderson CM, Ohashi K, Khan A, Teicher MH. Association of prepubertal and postpubertal exposure to childhood maltreatment with adult amygdala function. JAMA Psychiatry. 2019;76:843–53.
Teicher MH, Parigger A. The ‘Maltreatment and Abuse Chronology of Exposure’ (MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One. 2015;10:e0117423.
Hariri AR, Tessitore A, Mattay VS, Fera F, Weinberger DR. The amygdala response to emotional stimuli: a comparison of faces and scenes. Neuroimage. 2002;17:317–23.
LeDoux JE, Brown R. A higher-order theory of emotional consciousness. Proc Natl Acad Sci USA 2017;114:E2016–E25.
LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry. 2016;173:1083–93.
LeDoux JE. Synaptic self: how our brains become who we are. Harmondsworth, England: Viking Penguin; 2002.
Mujica-Parodi LR, Cha J, Gao J. From anxious to reckless: a control systems approach unifies prefrontal-limbic regulation across the spectrum of threat detection. Front Syst Neurosci. 2017;11:18.
Herringa RJ, Birn RM, Ruttle PL, Burghy CA, Stodola DE, Davidson RJ, et al. Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proc Natl Acad Sci USA 2013;110:19119–24.
Herringa RJ, Burghy CA, Stodola DE, Fox ME, Davidson RJ, Essex MJ. Enhanced prefrontal-amygdala connectivity following childhood adversity as a protective mechanism against internalizing in adolescence. Biol Psychiatry Cogn Neurosci Neuroimaging. 2016;1:326–34.
Teicher MH, Samson JA. Childhood maltreatment and psychopathology: a case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry. 2013;170:1114–33.
Maroun M. Stress reverses plasticity in the pathway projecting from the ventromedial prefrontal cortex to the basolateral amygdala. Eur J Neurosci. 2006;24:2917–22.
Wolf RC, Herringa RJ. Prefrontal-amygdala dysregulation to threat in pediatric posttraumatic stress disorder. Neuropsychopharmacology. 2016;41:822–31.
Williams LM, Phillips ML, Brammer MJ, Skerrett D, Lagopoulos J, Rennie C, et al. Arousal dissociates amygdala and hippocampal fear responses: evidence from simultaneous fMRI and skin conductance recording. Neuroimage. 2001;14:1070–9.
Strobl C, Boulesteix A-L, Zeileis A, Hothorn T. Bias in random forest variable importance measures: illustrations, sources and a solution. BMC Bioinform. 2007;8:1–21.
Tomoda A, Polcari A, Anderson CM, Teicher MH. Reduced visual cortex gray matter volume and thickness in young adults who witnessed domestic violence during childhood. PLoS One. 2012;7:e52528.
Schalinski I, Teicher MH, Nischk D, Hinderer E, Muller O, Rockstroh B. Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry. 2016;16:295.
McCrory EJ, Gerin MI, Viding E. Annual research review: childhood maltreatment, latent vulnerability and the shift to preventative psychiatry—the contribution of functional brain imaging. J Child Psychol Psychiatry. 2017;58:338–57.
McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–91.
Sheridan MA, McLaughlin KA. Dimensions of early experience and neural development: deprivation and threat. Trends Cogn Sci. 2014;18:580–5.
Gee DG, Gabard-Durnam LJ, Flannery J, Goff B, Humphreys KL, Telzer EH, et al. Early developmental emergence of human amygdala-prefrontal connectivity after maternal deprivation. Proc Natl Acad Sci USA 2013;110:15638–43.
Keding TJ, Heyn SA, Russell JD, Zhu X, Cisler J, McLaughlin KA, et al. Differential patterns of delayed emotion circuit maturation in abused girls with and without internalizing psychopathology. Am J Psychiatry. 2021;178:1026–36.
Yang TT, Simmons AN, Matthews SC, Tapert SF, Bischoff-Grethe A, Frank GK, et al. Increased amygdala activation is related to heart rate during emotion processing in adolescent subjects. Neurosci Lett. 2007;428:109–14.
Critchley HD, Rotshtein P, Nagai Y, O’Doherty J, Mathias CJ, Dolan RJ. Activity in the human brain predicting differential heart rate responses to emotional facial expressions. Neuroimage. 2005;24:751–62.
Iffland B, Klein F, Rosner R, Renneberg B, Steil R, Neuner F. Cardiac reactions to emotional words in adolescents and young adults with PTSD after child abuse. Psychophysiology. 2020;57:e13470.
Portnoy J, Cui N, Raine A, Frazier A, Rudo-Hutt AS, Liu J. Autonomic nervous system activity and callous-unemotional traits in physically maltreated youth. Child Abus Negl. 2020;101:104308.
Sharman LS, Dingle GA, Vingerhoets A, Vanman EJ. Using crying to cope: physiological responses to stress following tears of sadness. Emotion. 2020;20:1279–91.
Hubel DH, Wiesel TN. Early exploration of the visual cortex. Neuron. 1998;20:401–12.
Berardi N, Pizzorusso T, Maffei L. Critical periods during sensory development. Curr Opin Neurobiol. 2000;10:138–45.
Erzurumlu RS, Gaspar P. Development and critical period plasticity of the barrel cortex. Eur J Neurosci. 2012;35:1540–53.
Laham BJ, Gould E. How stress influences the dynamic plasticity of the brain’s extracellular matrix. Front Cell Neurosci. 2021;15:814287.
Baldwin JR, Reuben A, Newbury JB, Danese A. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76:584–93.
Edwards F, Wakefield S, Healy K, Wildeman C. Contact with Child Protective Services is pervasive but unequally distributed by race and ethnicity in large US counties. Proc Natl Acad Sci USA 2021;118:e2106272118.
Luby JL, Baram TZ, Rogers CE, Barch DM. Neurodevelopmental optimization after early-life adversity: cross-species studies to elucidate sensitive periods and brain mechanisms to inform early intervention. Trends Neurosci. 2020;43:744–51.
Teicher MH, Gordon JB, Nemeroff CB. Recognizing the importance of childhood maltreatment as a critical factor in psychiatric diagnoses, treatment, research, prevention, and education. Mol Psychiatry. 2021;27:1331–8.
Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31:968–80.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15:273–89.
Acknowledgements
This work was supported by the National Institutes of Health grants (Grant Nos. MH-091391, MH-113077, DA-017846, HD-0794841 [to MHT]), ANS Research Foundation ([to MHT]), National Natural Science Foundation of China (Grant No. 32000755 [to JZ]) and Natural Science Foundation of Zhejiang Province (Grant No. LQ21C090008 [to JZ]). Cynthia E. McGreenery and Elizabeth Bolger, MA, Developmental Biopsychiatry Research Program, McLean Hospital, Belmont, Massachusetts, assisted with recruitment and assessment of study participants and Michael Rohan, Ph.D., and Gordana Vitaliano, MD, Ph.D., Brain Imaging Center, McLean Hospital, Belmont, Massachusetts, provided technical and clinical support. All of these individuals received compensation for their help.
Author information
Authors and Affiliations
Contributions
MHT conceived the idea and was responsible for funding acquisition and project administration. MHT, JZ, K0, and AK were responsible for the methodology. Data were collected by AK, CMA, and KO and were curated by CMA, KO, and JZ. Formal analyses and visualizations were performed by JZ and MHT, and software was written by MHT, JZ, and KO. The original draft was written by MHT and JZ. All the other authors reviewed and edited the final drafts.
Corresponding authors
Ethics declarations
Competing interests
MHT created the MACE scale used to collect data on type and timing of exposure to maltreatment used in this study. However, there is no financial conflict as this scale was placed into the public domain and it is fully available and free to use. The other authors declare that they have no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, J., Anderson, C.M., Ohashi, K. et al. Potential sensitive period effects of maltreatment on amygdala, hippocampal and cortical response to threat. Mol Psychiatry 28, 5128–5139 (2023). https://doi.org/10.1038/s41380-023-02002-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02002-5
This article is cited by
-
Effects of childhood maltreatment and major depressive disorder on functional connectivity in hippocampal subregions
Brain Imaging and Behavior (2024)
-
The neurobiological effects of childhood maltreatment on brain structure, function, and attachment
European Archives of Psychiatry and Clinical Neuroscience (2024)