Abstract
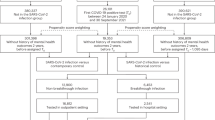
Previous studies on psychiatric patients infected with COVID-19 have reported a more severe course of disease and higher rates of mortality compared with the general population. This cohort study linked Israeli national databases including all individuals ever hospitalized for a psychiatric disorder (cases), and COVID-19 testing, infection, hospitalization, mortality, and vaccinations, between March 1st 2020 and March 31st 2021. Cases were 125,273 individuals aged 18 and above ever hospitalized in a psychiatric facility (ICD-10 F10-F69 or F90-F99), compared to the total population, n = 6,143,802. Compared with the total population, cases were less likely to be tested for COVID-19, 51.2% (95% CI: 50.8–51.7) vs 62.3% (95% CI 62.2–62.4) and had lower rates of confirmed COVID infection, 5.9% (95% CI: 5.8–6.1) vs 8.9% (95% CI: 8.9–8.9). Among those infected, risks for COVID-19 hospitalization, COVID-19 attributed mortality and all-cause mortality were higher for cases than the total population, adjusted odds ratios were 2.10; (95% CI: 1.96–2.25), 1.76; (95% CI: 1.54–2.01) and 2.02; (95% CI: 1.80–2.28), respectively. These risks were even higher for cases with non-affective psychotic disorders and bipolar disorder. Age adjusted rates of vaccination were lower in cases, 60.4% (95% CI: 59.9–60.8) vs 74.9% (95% CI: 74.8–75.0) in the total population, and particularly low for cases with non-affective psychotic disorders, 56.9% (95% CI: 56.3–57.6). This study highlights the need to increase testing for COVID-19 in individuals ever hospitalized for a psychiatric disorder, closely monitor those found positive, and to reach out to encourage vaccination.
Similar content being viewed by others
Introduction
Some [1, 2] but not all [3] studies have shown that, compared to controls or to the general population, individuals with a psychiatric disorder were more likely to be tested for COVID-19. Similarly, some [4,5,6,7] but not other [1, 3, 8] studies have shown that individuals with a psychiatric disorder were more likely to have a positive test result. If infected with COVID-19, individuals with a psychiatric disorder [3, 6, 7, 9,10,11,12], especially bipolar disorder [8] or schizophrenia [2, 13, 14], are at increased risk of suffering from a more severe course of illness and have higher rates of mortality. These studies were limited, in that some [7, 8] did not include entire populations, and others [2, 9] did not control for deaths unrelated to COVID-19 in individuals with a psychiatric disorders [3, 11, 12, 14] Many authors have recommended prioritization of COVID-19 vaccination for people with severe mental illness, and some but not all studies reported lower rates of vaccination in persons with psychiatric disorders [15, 16] compared with controls. To date, no studies have been published on rates of vaccination for COVID-19 of individuals with a history of hospitalization for a psychiatric disorder in an entire country.
The aim of this study was to compare rates of testing, infection, hospitalization, mortality, and vaccinations for COVID-19 between individuals with a history of hospitalization for a psychiatric disorder, and the general population.
Materials and methods
In Israel, the national psychiatric case register (NPCR) is mandated by law, and records all hospitalizations and discharges in any psychiatric inpatient facility in the country, using the patient’s unique identity number. In this study, we followed up a nation-wide cohort of all persons ever hospitalized before March 1st 2020 (the onset of COVID-19 in Israel), aged 18 and above on that date with a psychiatric disorder, defined as an ICD-10 diagnosis of F10-F69 or F90-F99. We looked specifically at persons from this cohort with a last discharge diagnosis of non-affective psychotic disorders (F20-F29), in particular schizophrenia (F20.0-F20.9), and with any affective disorder (F30-F39), in particular bipolar disorder (F30-F31). Where the last-discharge diagnosis was not available the diagnosis at the last admission was used.
Israel has national databases on COVID-19, including the results of all tests for COVID-19 using RT-PCR, data on COVID-19 hospitalization, death attributed to COVID-19, all-cause mortality, and data on vaccinations against COVID-19. Persons who tested positive for COVID-19 were further questioned for underlying diseases, and these data were recorded in the COVID-19 database. Data on psychiatric hospitalizations was merged with the COVID-19 databases using the unique identity number of each citizen in the country, utilizing data available until March 31, 2021 for testing, infection, hospitalization and vaccination, and until April 30, 2021 for death, to allow for follow up between hospitalization and death of at least one month.
Israel administered the Pfizer BNT162B2 vaccine, starting on 19 December 2021. The vaccinations were administered free-of-charge in easily accessible vaccination centers located all over the country to all members of the population aged 16 and above. We identified all citizens who had had two doses of vaccine by March 31, 2021, calculating their rate using those alive in the country on that date as the denominator.
Data analysis
Age-specific and age-adjusted percentages were calculated for testing, confirmed infection and vaccination, dividing the population into age groups of 18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84 and 85 and above, and using the Israeli population in 2019 as the standard population. Rates of COVID-19 hospitalization, COVID-19 attributed deaths and all-cause mortality as an age-adjusted percentage of those infected by COVID-19 over the study period were calculated. These rates were calculated for individuals with a history of hospitalization for a psychiatric disorder compared to the total population aged 18 and above on March 1st, 2020, using population estimates based on data from the Israeli Central Bureau of Statistics (CBS, https://www.cbs.gov.il). Hospitalization and mortality among those with a confirmed infection with COVID-19 were further compared between individuals with a history of hospitalization for a psychiatric disorder and the total population using two logistic regression models, one controlling for sex and age (grouped into 18–54, 55–64, 65–74, 75–84 and 85+) and the second with the addition of vaccination status (if fully vaccinated before COVID-19 diagnosis) and comorbid medical conditions, including heart disease, diabetes, hypertension, lung disease, liver disease, immunosuppression, cancer, asthma, kidney disease, cerebrovascular disease, dementia, digestive system diseases, thyroid disease, hypercholesterolemia and obesity.
In order to examine the additive effect of COVID-19 on all-cause-mortality, age-adjusted rates of all deaths in individuals with a history of hospitalization for a psychiatric disorder not infected with COVID-19 during the study period was calculated.
Finally, among individuals with a history of hospitalization for a psychiatric disorder, a multiple logistic regression model examined the effect of demographic and clinical factors on the likelihood of being tested for or infection with COVID-19, and of being vaccinated. Factors included in the model were sex, age, psychiatric diagnosis grouped into non-affective psychotic disorders, affective disorders or other psychiatric disorders; drug or alcohol abuse, suicide attempt before any psychiatric hospitalization, having at least one involuntary hospitalization, and the number of psychiatric hospitalizations.
This study was approved by the IRB of the Israeli Ministry of Health. The identity number was encrypted in order to protect the identity of the study participants.
Results
There were 125,273 individuals alive aged 18 and above on March 1st 2020, with a history of hospitalization for a psychiatric disorder.
Rates of COVID-19 testing
Compared with the total population, rates of having at least one COVID-19 PCR test were lower in individuals with a history of hospitalization for a psychiatric disorder for those aged under 65, and aged 85 and over, with no significant differences at ages 65–74, and higher rates of testing in the total population for persons aged 75–84. Sixty two point three percent (95% CI 62.2–62.4) of the total population had at least one COVID-19 test, compared to 51.2% (95% CI 50.8–51.7) of individuals with a history of hospitalization for a psychiatric disorder (age adjusted rates, Fig. 1A, and web supplement).
Age adjusted rates of COVID-19 confirmed infection, hospitalization and mortality (Table 1)
The confirmed infection rate with COVID-19 was lower among individuals with a history of hospitalization for a psychiatric disorder (5.9%; 95% CI 5.8–6.1) than in the total population (8.9%; 95% CI 8.9–8.9).
Among persons with a confirmed infection with COVID-19, the hospitalization rate in the total population was 8.8% (95% CI: 8.7–8.8), and was significantly higher among individuals with a history of hospitalization for a psychiatric disorder (15.1%, 95% CI 14.2–15.9), highest for schizophrenia (17.2%, 95% CI 15.5–19.0) and somewhat lower for bipolar disorder (12.5%, 95% CI 9.8–15.2). The mortality rate both for COVID-19 related deaths and all deaths was also higher in individuals with a history of hospitalization for a psychiatric disorder, 2.9% (95% CI 2.5–3.2) and 4.1% (95% CI 3.7–4.5), respectively, 1.6–1.7 times the rates in the total population (1.8%, 95% CI 1.8–1.9 and 2.4%, 95% CI 2.3–2.4, respectively).
All-cause mortality rates for individuals with a history of hospitalization for a psychiatric disorder with a confirmed infection with COVID-19 were over twice as high compared to persons with the same psychiatric diagnoses without COVID-19 (Table 1), particularly for males, 5.1% (95% CI 4.4–5.8), compared to 2.1% (95% CI 2.0–2.2) for those without COVID-19.
Rates of confirmed COVID-19 infection were slightly lower, and rates of hospitalization and mortality higher for males than females in all diagnostic groups.
Rate ratios with 95% CI are presented in the web supplement.
Effect of age on rates of confirmed COVID-19 infection, hospitalization and mortality
Confirmed COVID-19 infection rates were significantly higher in the total population compared to individuals with a history of hospitalization for a psychiatric disorder up to age 65; at ages 75–84 individuals with a history of hospitalization for a psychiatric disorder had higher rates of confirmed COVID-19 infection. In persons over age 85 there was no significant difference between the groups (Fig. 1B and web-supplement).
Hospitalizations and mortality rates attributed to COVID-19, and all-cause mortality rates were significantly higher in individuals with a history of hospitalization for a psychiatric disorder up to age 74; at age 75 and above there were no significant differences between individuals with a history of hospitalization for a psychiatric disorder and the total population (Fig. 2 and web-supplement).
Risk of hospitalization and mortality in individuals with confirmed COVID-19 infection
Among individuals with confirmed COVID-19 infection, the age and sex adjusted risks of hospitalization and all-cause mortality were over twice as high for individuals with a history of hospitalization for a psychiatric disorder compared to the total population, adjusted odd ratio (AOR) 2.10 (95% CI 1.96–2.25) and 2.02 (95% CI 1.80–2.28), respectively. Risk of death attributed to COVID-19 was also increased, to a somewhat lesser extent, AOR = 1.76 (95% CI 1.54–2.01). Risk for hospitalization and all-cause mortality was even higher amongst persons with schizophrenia, AOR = 2.43 (95% CI 2.16–27.3), and 2.42 (95% CI 2.00–2.94), respectively (Table 2). When vaccination status and underlying medical comorbidity were added to the model, the adjusted OR increased, reaching 2.52 (95% 2.24–2.84) and 2.69 (95% CI 2.21–3.27) for hospitalization and all-cause mortality amongst persons with schizophrenia.
Rates of COVID-19 vaccination
Individuals with a history of hospitalization for a psychiatric disorder were less likely to be vaccinated at all ages. Total age-adjusted vaccination rate was 74.9% (95% CI: 74.8–75.0) for the total population aged 18 and over, compared to 60.4% (95% CI: 59.9–60.8) for those with a history of hospitalization for a psychiatric disorder; 56.9% (95% CI: 56.3–57.6) for persons with non-affective psychotic disorders, and 66.5% (95% CI 65.3–67.7) for persons with affective disorders. Rates of vaccination were especially low in individuals with a history of hospitalization for a psychiatric disorder aged 85 and above, 48.3% (95% CI 46.5–50.1), particularly in persons with non-affective psychotic disorders, 37.2% (95% CI 34.4–39.9), compared to the rates of persons vaccinated in the total population, 80.4% (95% CI 80.2–80.6, Fig. 1C and web-supplement).
Risk for COVID-19 testing, confirmed infection and vaccination among individuals with a history of hospitalization for a psychiatric disorder
Table 3 shows the odds ratios and 95% CI from multiple logistic models predicting whether individuals with a history of hospitalization for a psychiatric disorder would be tested for COVID-19, be infected, or be vaccinated.
The chance of being tested for COVID-19 was lower for males, declined steadily with age, was lowest for those with non-affective psychotic disorders and for those who had at least one involuntary psychiatric hospitalization.
Compared to persons aged 18–24, risk of confirmed infection among individuals with a history of hospitalization for a psychiatric disorder was significantly lower in all other age groups. Persons with substance or alcohol abuse reported at any psychiatric hospitalization had lowest risk for confirmed infection.
Older, compared with younger individuals with a history of hospitalization for a psychiatric disorder were more likely to be vaccinated; persons with affective disorders were more likely and persons with non-affective psychotic disorders were less likely to be vaccinated. Persons with drug/alcohol abuse recorded at any psychiatric hospitalization had lower rates of vaccination, AOR = 0.79 (95% CI 0.77–0.82), and 0.78 (95% CI 0.74–0.81), respectively, as did those with a history of at least one involuntary hospitalization, AOR = 0.67 (95% CI 0.65–0.69).
The chance for an individual with a history of hospitalization for a psychiatric disorder to be tested for COVID-19, have a confirmed infection or to be vaccinated increased significantly with number of hospitalizations, particularly for testing (Table 3).
Discussion
This study on the entire population of Israel examined the effect of COVID-19 on all individuals with a history of hospitalization for a psychiatric disorder compared to the total population, finding that individuals with a history of hospitalization for a psychiatric disorder, particularly those with non-affective psychotic disorders, were less likely to be tested for COVID-19 and had fewer confirmed COVID-19 infections. Those infected were more likely to be hospitalized and to die. Individuals with a history of hospitalization for a psychiatric disorder, particularly those with non-affective psychotic disorders, had lower rates of vaccination compared with the total population.
Testing for COVID-19
Compared to the total population (62%), the percentage of individuals with a history of hospitalization for a psychiatric disorder that were tested for COVID-19 at least once was lower (51%), particularly persons with non-affective psychotic disorders (49%). This finding might be caused by lack of initiative in mentally ill persons, particularly males with non-affective psychotic disorders, who typically have higher levels of negative symptoms [17], are less active socially and have less contact with verified cases, hence are less often referred to testing. This result differs from a previous study of Tzur Bitan in Israel [2], which reported more testing for COVID-19 in persons with schizophrenia (30.2% vs. 22.1% in the control group). That study was based on data from the largest HMO in the country, providing health care to approximately half of the population, but used data until October 2020, covering the first wave of COVID-19 in Israel, during which testing was relatively limited. The data in this current study includes the next two, larger waves, when massive testing was done in Israel, which might explain the higher rate of testing in the total population. Data on testing in the UK-Biobank also found higher rates of testing for COVID-19 in psychiatric patients, but those data are from the beginning of the pandemic (April 2020) and are not population-based. In addition, the Biobank study and the previous Israeli study included individuals who had been hospitalized, but also included data from primary care physicians on individuals who have never been hospitalized for a psychiatric disorder and might be presumed to be less severely ill, hence more aware of the importance of being tested. The higher probability of testing in those with more psychiatric hospitalizations may reflect the policy of testing all individuals before admission to psychiatric facilities, and repeat testing in hospitalized individuals in cases of suspected exposure to individuals with COVID-19.
Rates of confirmed COVID-19 infection
Previous authors have hypothesized that persons with mental illness live socially isolated lives [11, 18], thus having less contact and less exposure to infection. The results of the current study, comparing rates of confirmed infection with COVID-19 in individuals with a history of hospitalization for a psychiatric disorder with the total population, were in accord with this hypothesis, finding lower rates of infection among individuals with a history of hospitalization for a psychiatric disorder, especially in patients who reported abusing drugs or alcohol. Similar findings were reported in the UK population-based study [1] and in the study on the large HMO in Israel [2]. A population-based study from South Korea reported no difference in rates of confirmed COVID-19 infection between psychiatric patients and the general population, while a large study from the US found that people with mental disorders had higher rates of confirmed COVID-19 infection [3, 7]. However, the latter two studies included persons with who had not been hospitalized in psychiatric facilities, many of whom presumably had less severe psychopathology.
Hospitalization and mortality
Among persons with confirmed infection with COVID-19, individuals with a history of hospitalization for a psychiatric disorder were twice as likely to be hospitalized or to die from any cause, compared with the total population. The adjusted mortality risk was highest in persons with non-affective psychotic or bipolar disorders. This is similar to the twofold higher mortality in individuals with a history of hospitalization for a psychiatric disorder unrelated to COVID-19, reported all over the world, and in Israel [19,20,21]. The risk for COVID-19 attributed deaths was also increased, but somewhat less than for all-cause mortality, presumably reflecting the high risk of mortality from COVID-19 in all persons infected, with or without a history of hospitalization for a psychiatric disorder. In persons over age 75, there was no significant difference in mortality between persons with confirmed infection with COVID-19 with or without a history of hospitalization for a psychiatric disorder. This may be due to the high excess mortality during the COVID-19 pandemic found in this age group [22], which appears to overshadow the increased risk for mortality in individuals with a history of hospitalization for a psychiatric disorder.
Similar findings have been reported in several studies on schizophrenia and affective disorders, and confirmed in meta-analyses [10,11,12]. Those papers compared rates of mortality in persons with a psychiatric disorder with a confirmed infection with COVID-19, with persons without these diagnoses, controlling for potential confounders, and found, as we did, an approximately twofold increased risk of death. Our data expands on those findings, and add greater precision by directly comparing mortality in individuals with a history of hospitalization for a psychiatric disorder who did or did not have a confirmed infection with COVID-19, finding rates of mortality in those with a confirmed infection with COVID-19 to be over double those of the non-infected.
The data reported here cannot explain these high mortality rates in individuals with a history of hospitalization for a psychiatric disorder infected with COVID-19. Possible mechanisms that have been suggested include barriers to care, which are probably not the case, as universal insurance coverage ensures equal access to medical care and hospitalization to all citizens in Israel. These findings are not due to anti-psychotic treatment, which has recently been shown not to cause mortality in patients with a psychiatric disorder infected with COVID-19 [23]. These data cannot relate to other proposed mechanisms, such as social determinants of health, and immunological disturbances [10, 18].
Vaccinations
To the best of our knowledge, this is the first report on vaccinations for COVID-19 in individuals with a history of hospitalization for a psychiatric disorder from an entire population, showing considerably lower rates, 60% compared to 75% in the total population, with the lowest rates in persons with non-affective psychotic disorders, 57%. There are little data published on vaccination for COVID-19 of persons with psychiatric disorders. One study from the UK described trends and variations in vaccine coverage, and mentioned that persons with a psychiatric disorder were less likely to be vaccinated compared to the general population (89.5% vs. 94.7%) [24]. The study conducted in the largest HMO in Israel focused on vaccination rates for persons with schizophrenia and also reported lower rates of vaccination [15], while a study from Belgium on psychiatric inpatients reported rates of vaccine acceptance [16] similar to the general population.
Risk for non-vaccination was particularly increased in individuals with a history of hospitalization for a psychiatric disorder aged 85 and older, particularly those with non-affective psychotic disorders, of whom only 37% were vaccinated, compared with 80% in persons that age in the total population. The reasons for these particularly low rates of vaccination in elderly individuals with a history of hospitalization for a psychiatric disorder are not clear. Other risk factors for non-vaccination in individuals with a history of hospitalization for a psychiatric disorder include use of alcohol or drugs, and a history of involuntary admission, perhaps indicating that the more severely ill persons are less likely to be vaccinated. On the other hand, as the number of hospitalizations increased, so did the chances of being vaccinated. This is probably because in January 2021 all patients hospitalized in psychiatric hospitals were vaccinated, including persons chronically hospitalized, many of whom had large numbers of previous hospitalizations compared to the majority of persons with a psychiatric disorder who live in the community.
It is important to mention that Israel was the first country in the world to vaccinate on a large scale, and there was much uncertainty both regarding the effectiveness and potential side-effects of the vaccine, factors which greatly impacted vaccine acceptance in the general population [25], and probably caused hesitancy in the individuals with a history of hospitalization for a psychiatric disorder reported here. The vaccine hesitancy reported here might be attributed to lack of awareness related to cognitive impairment, lack of motivation and low levels of activity. In a minority of patients, paranoia might be a factor [26, 27]. The lower vaccination rate for COVID-19 in individuals with a history of hospitalization for a psychiatric disorder is consistent with the literature regarding other preventive vaccines. For example, rates of vaccination for influenza in persons with mental illness are as low as 25% [28, 29].
It is important to understand these findings in the context of the Israeli health and mental health system. Based on the National Health Insurance Law, all citizens receive free medical and psychiatric care, with nominal payment for clinical visits and medication and no hospitalization charge. Those services are administered by four official health insurance organizations that compete and receive payment from the government for each patient. These disparities in treatment and morbidity disparities in a country that allows full access to medical treatment for individuals with a psychiatric disorder raise significant concerns regarding even greater disparities in countries with less accessible health systems.
The strengths of this study are the large nationwide database including all individuals with a history of hospitalization for a psychiatric disorder, which was merged with nationwide databases on all COVID-19 tests, confirmed infection, hospitalization, mortality and vaccinations in the entire country, enabling direct comparison of these variables between individuals with a history of hospitalization for a psychiatric disorder and the total population. Study limitations include the fact that individuals with a psychiatric disorder were identified based on having been hospitalized at least once during their lifetime in a psychiatric facility, hence does not include information about outpatients who have never been hospitalized, including the majority of individuals with affective disorders, drug and alcohol abuse, anxiety and personality disorders, However, at least for schizophrenia, a previous study [30] found that 93% of all persons with schizophrenia will be hospitalized at some point of their lives. Furthermore, the diagnoses in the hospitalization registry are clinician-based and are not research diagnoses. However, a study comparing the clinical diagnoses in the registry with research diagnoses reported agreement in 87–89% of the cases [31]. We also did not have medical data for the total population to enable adjustment for these factors. When analyzing outcomes of infected persons we adjusted for medical comorbidity but those data were based on self-report and not on medical records, and therefore may not be complete or accurate. Lastly, we reported on testing and risk of confirmed infection with COVID-19 but do not have data on infected individuals who are asymptomatic and are not tested. This might be more common in individuals with a history of hospitalization for a psychiatric disorder, who might be less aware of their symptoms or less likely to come in to be tested when symptomatic.
Conclusions
Despite these limitations, this study highlights the need to increase testing for COVID-19 in individuals with a history of hospitalization for a psychiatric disorder, and closely monitor those found positive for potential medical complications. Efforts must be made to reach-out to vaccinate persons with individuals with a history of hospitalization for a psychiatric disorder, particularly older males with schizophrenia who are both least likely to be vaccinated, and are at highest risk for mortality.
References
van der Meer D, Pinzón-Espinosa J, Lin BD, Tijdink JK, Vinkers CH, Guloksuz S et al. Associations between psychiatric disorders, COVID-19 testing probability and COVID-19 testing results: findings from a population-based study. BJPsych Open. 2020;6:e87.
Tzur Bitan D, Krieger I, Kridin K, Komantscher D, Scheinman Y, Weinstein O, et al. COVID-19 prevalence and mortality among schizophrenia patients: a large-scale retrospective cohort study. Schizophrenia Bull. 2021;47:1211–7.
Lee SW, Yang JM, Moon SY, Yoo IK, Ha EK, Kim SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020;7:1025–31.
Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–40.
Yang H, Chen W, Hu Y, Chen Y, Zeng Y, Sun Y, et al. Pre-pandemic psychiatric disorders and risk of COVID-19: a UK Biobank cohort analysis. Lancet Healthy Longev. 2020;1:e69–e79.
Liu L, Ni S-Y, Yan W, Lu Q-D, Zhao Y-M, Xu Y-Y, et al. Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: A systematic review, meta-analysis and call for action. EClinicalMedicine. 2021;40:101111.
Wang Q, Xu R, Volkow ND. Increased risk of COVID‐19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20:124–30.
Egede C, Dawson AZ, Walker RJ, Garacci E, Campbell JA, Egede LE. Relationship between mental health diagnoses and COVID-19 test positivity, hospitalization, and mortality in Southeast Wisconsin. Psychol Med. 2021:1–26.
Nemani K, Conderino S, Marx J, Thorpe LE, Goff DC. Association between antipsychotic use and COVID-19 mortality among people with serious mental illness. JAMA Psychiatry. 2021;78:1391–3.
Vai B, Mazza MG, Delli Colli C, Foiselle M, Allen B, Benedetti F et al. Mental disorders and risk of Covid-19 related mortality, hospitalization and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8:P797-812.
Fond G, Nemani K, Etchecopar-Etchart D, Loundou A, Goff DC, Lee SW, et al. Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78:1208–17.
Ceban F, Nogo D, Carvalho IP, Lee Y, Nasri F, Xiong J, et al. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78:1079–91.
Toubasi AA, AbuAnzeh RB, Tawileh HBA, Aldebei RH, Alryalat SAS. A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. 2021;299:113856.
De Hert M, Mazereel V, Stroobants M, De Picker L, Van Assche K, Detraux J. COVID-19-related mortality risk in people with severe mental illness: a systematic and critical review. Front Psychiatry. 2021;12:798554.
Bitan DT, Kridin K, Cohen AD, Weinstein O. COVID-19 hospitalisation, mortality, vaccination, and postvaccination trends among people with schizophrenia in Israel: a longitudinal cohort study. Lancet Psychiatry. 2021;8:901–8.
Mazereel V, Vanbrabant T, Desplenter F, De Hert M. COVID-19 vaccine uptake in patients with psychiatric disorders admitted to or residing in a university psychiatric hospital. Lancet Psychiatry. 2021;8:860–1.
Grossman LS, Harrow M, Rosen C, Faull R, Strauss GP. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr psychiatry. 2008;49:523–9.
Fond G, Pauly V, Leone M, Llorca P-M, Orleans V, Loundou A, et al. Disparities in intensive care unit admission and mortality among patients with schizophrenia and COVID-19: a national cohort study. Schizophrenia Bull. 2021;47:624–34.
Health Mo. Mental Health in Israel. Statistical Abstract of Israel. 2019; 70. https://www.gov.il/he/Departments/publications/reports/mtl-yearbook-2019.
Health Mo. Mental Health in Israel. Statistical Abstract of Israel. 2021; 72. https://www.gov.il/he/Departments/publications/reports/mtl-yearbook-2021.
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–41.
Haklai Z, Aburbeh M, Goldberger N, Gordon E-S. Excess mortality during the COVID-19 pandemic in Israel, March–November 2020: when, where, and for whom? Isr J Health Policy Res. 2021;10:1–7.
Nemani K, Li C, Olfson M, Blessing EM, Razavian N, Chen J, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78:380–6.
Curtis HJ, Inglesby P, Morton CE, MacKenna B, Walker AJ, Morley J et al. Trends and clinical characteristics of COVID-19 vaccine recipients: a federated analysis of 57.9 million patients’ primary care records in situ using OpenSAFELY. Br J Gen Pract. 2021;72:e51–e62.
Gurwitz D. COVID-19 vaccine hesitancy: lessons from Israel. Vaccine. 2021;39:3785–6.
Payberah E, Payberah D, Sarangi A, Gude J. COVID-19 vaccine hesitancy in patients with mental illness: strategies to overcome barriers—a review. J Egypt Public Health Assoc. 2022;97:1–6.
Batty GD, Deary IJ, Altschul D. Pre-pandemic mental and physical health as predictors of COVID-19 vaccine hesitancy: evidence from a UK-wide cohort study. Ann Med. 2022;54:274–82.
Miles LW, Williams N, Luthy KE, Eden L. Adult vaccination rates in the mentally ill population: an outpatient improvement project. J Am Psychiatr Nurses Assoc. 2020;26:172–80.
Lorenz RA, Norris MM, Norton LC, Westrick SC. Factors associated with influenza vaccination decisions among patients with mental illness. Int J Psychiatry Med. 2013;46:1–13.
Weiser M, Werbeloff N, Dohrenwend BP, Levav I, Yoffe R, Davidson M. Do psychiatric registries include all persons with schizophrenia in the general population? A population-based longitudinal study. Schizophrenia Res. 2012;135:187–91.
Weiser M, Kanyas K, Malaspina D, Harvey PD, Glick I, Goetz D, et al. Sensitivity of ICD-10 diagnosis of psychotic disorders in the Israeli National Hospitalization Registry compared with RDC diagnoses based on SADS-L. Compr Psychiatry. 2005;46:38–42.
Author information
Authors and Affiliations
Contributions
NG Analyzed the data. TBL contributed to writing the protocol obtaining regulatory approval, and commented on the paper. ZH contributed to writing the protocol obtaining regulatory approval, and commented on the paper. RY contributed to writing the protocol obtaining regulatory approval, and commented on the paper. MD Commented on the final manuscript. ES contributed to writing the protocol obtaining regulatory approval, and commented on the paper. LL commented on the final manuscript. TE brought in the first draft of the paper and commented on the final manuscript, MW conceived the study, obtained IRP approval, commented on the manuscript, and takes full responsibility for the entire project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Goldberger, N., Bergman-Levy, T., Haklai, Z. et al. COVID-19 and severe mental illness in Israel: testing, infection, hospitalization, mortality and vaccination rates in a countrywide study. Mol Psychiatry 27, 3107–3114 (2022). https://doi.org/10.1038/s41380-022-01562-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-022-01562-2
This article is cited by
-
The anxiety response of patients with severe psychiatric disorders to the recent public health crisis
BMC Psychiatry (2024)
-
Long-term consequences of COVID-19 on mental health and the impact of a physically active lifestyle: a narrative review
Annals of General Psychiatry (2023)
-
The COVID-19 Israeli tapestry: the intersectionality health equity challenge
Israel Journal of Health Policy Research (2023)
-
Comparison of attitudes toward the coronavirus disease vaccine, fear of coronavirus disease, and perception regarding causes of coronavirus disease between patients with serious mental illness and healthy controls
Journal of Public Health (2023)
-
COVID-19-Impfung für Menschen mit schweren psychischen Erkrankungen
Der Nervenarzt (2023)