Abstract
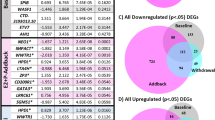
The estimated 20–30% of women who develop perimenopausal depression (PMD) are at an increased risk of cardiovascular and all-cause mortality. The therapeutic benefits of estradiol (E2) and symptom-provoking effects of E2-withdrawal (E2-WD) suggest that a greater sensitivity to changes in E2 at the cellular level contribute to PMD. We developed an in vitro model of PMD with lymphoblastoid cell lines (LCLs) derived from participants of a prior E2-WD clinical study. LCLs from women with past PMD (n = 8) or control women (n = 9) were cultured in three experimental conditions: at vehicle baseline, during E2 treatment, and following E2-WD. Transcriptome analysis revealed significant differences in transcript expression in PMD in all experimental conditions, and significant overlap in genes that were changed in PMD regardless of experimental condition. Of these, chemokine CXCL10, previously linked to cardiovascular disease, was upregulated in women with PMD, but most so after E2-WD (p < 1.55 × 10−5). CYP7B1, an enzyme intrinsic to DHEA metabolism, was upregulated in PMD across experimental conditions (F(1,45) = 19.93, p < 0.0001). These transcripts were further validated via qRT-PCR. Gene networks dysregulated in PMD included inflammatory response, early/late E2-response, and cholesterol homeostasis. Our results provide evidence that differential behavioral responsivity to E2-WD in PMD reflects intrinsic differences in cellular gene expression. Genes such as CXCL10, CYP7B1, and corresponding proinflammatory and steroid biosynthetic gene networks, may represent biomarkers and molecular targets for intervention in PMD. Finally, this in vitro model allows for future investigations into the mechanisms of genes and gene networks involved in the vulnerability to, and consequences of, PMD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63:375–82.
Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L. Hormones and menopausal status as predictors of depression in womenin transition to menopause. Arch Gen Psychiatry. 2004;61:62–70.
Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition. Arch Gen Psychiatry. 2006;63:385–90.
Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychological Med. 2011;41:1879–88.
Bromberger JT, Matthews KA, Schott LL, Brockwell S, Avis NE, Kravitz HM, et al. Depressive symptoms during the menopausal transition: The Study of Women’s Health Across the Nation (SWAN). J Affect Disord. 2007;103:267–72.
Wariso BA, Guerrieri GM, Thompson K, Koziol DE, Haq N, Martinez PE, et al. Depression during the menopause transition: impact on quality of life, social adjustment, and disability. Arch Women’s Ment Health. 2017;20:273–82.
Terauchi M, Hiramitsu S, Akiyoshi M, Owa Y, Kato K, Obayashi S, et al. Associations among depression, anxiety and somatic symptoms in peri- and postmenopausal women. J Obstet Gynaecol Res. 2013;39:1007–13.
Wassertheil-Smoller S, Shumaker S, Ockene J, Talavera GA, Greenland P, Cochrane B, et al. Depression and cardiovascular sequelae in postmenopausal women. Arch Intern Med. 2004;164:289–98.
Burger HG. The endocrinology of the menopause. Maturitas. 1996;23:129–36.
Freeman EW. Depression in the menopause transition: risks in the changing hormone milieu as observed in the general population. Women’s Midlife Health. 2015;1:2.
Daly, R. C., Danaceau, M. A., Rubinow, D. R., and Schmidt, P. J.: Concordant restoration of ovarian function and mood in perimenopausal depression. Am. J. Psychiatry. 2003 160:1842–6.
Tepper PG, Randolph JF, McConnell DS, Crawford SL, El Khoudary SR, Joffe H, et al. Trajectory clustering of estradiol and follicle-stimulating hormone during the menopausal transition among women in the Study of Women’s Health Across the Nation (SWAN). J Clin Endocrinol Metab. 2012;97:2872–80.
Santoro N, Brown JR, Adel T, Skurnick JH. Characterization of reproductive hormonal dynamics in the perimenopause. J Clin Endocrinol Metab. 1996;81:1495–501.
Schmidt PJ, Nieman L, Danaceau MA, Tobin MB, Roca CA, Murphy JH, et al. Estrogen replacement in perimenopause-related depression: a preliminary report. Am J Obstet Gynecol. 2000;183:414–20.
De Novaes Soares C, Almeida OP, Joffe H, Cohen LS. Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women. Arch Gen Psychiatry. 2001;58:529–34.
Gordon JL, Rubinow DR, Eisenlohr-Moul TA, Xia K, Schmidt PJ, Girdler SS. Efficacy of transdermal estradiol and micronized progesterone in the prevention of depressive symptoms in the menopause transition. JAMA Psychiatry. 2018;75:149–57.
Ockene JK. Symptom experience after discontinuing use of estrogen plus progestin. JAMA. 2005;294:183–93.
Ness J, Aronow WS, Beck G. Menopausal symptoms after cessation of hormone replacement therapy. Maturitas. 2006;53:356–61.
Schmidt PJ, Murphy JH, Haq N, Danaceau MA, St. Clair LS. Basal plasma hormone levels in depressed perimenopausal women. Psychoneuroendocrinology. 2002;27:907–20.
Schmidt PJ, Ben Dor R, Martinez PE, Guerrieri GM, Harsh VL, Thompson K, et al. Effects of estradiol withdrawal on mood in women with past perimenopausal depression: A randomized clinical trial. JAMA Psychiatry. 2015;72:714–26.
Dubey N, Hoffman JF, Schuebel K, Yuan Q, Martinez PE, Nieman LK et al. The ESC/E(Z) complex, an effector of response to ovarian steroids, manifests an intrinsic difference in cells from women with premenstrual dysphoric disorder. Mol Psychiatry. 2017;22:1172–84
Steinberg EM, Rubinow DR, Bartko JJ, Fortinsky PM, Haq N, Thompson K et al. A cross-sectional evaluation of perimenopausal depression. J Clin Psychiatry. 2008;69:973–80.
Oh HM, Oh JM, Choi SC, Kim SW, Han WC, Kim TH, et al. An efficient method for the rapid establishment of Epstein-Barr virus immortalization of human B lymphocytes. Cell Prolif. 2003;36:191–7.
Berthois Y, Katzenellenbogen JA, Katzenellenbogen BS. Phenol red in tissue culture media is a weak estrogen: implications concerning the study of estrogen-responsive cells in culture. Proc Natl Acad Sci. 1986;83:2496–500.
Welshons WV, Wolf MF, Murphy CS, Jordan VC. Estrogenic activity of phenol red. Mol Cell Endocrinol. 1988;57:169–78.
Milo GE MW, Powell JE, Blakeslee JR, Yohn DS. Effects of steroid hormones in fetal bovine serum on plating and cloning of human cells in vitro. In Vitro 1976;12:23–30.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodol). 1995;57:289–300.
Wang M, Zhao Y, Zhang B. Efficient test and visualization of multi-set intersections. Sci Rep. 2015;5:16923.
Turner SD. qqman: an R package for visualizing GWAS results using Q-Q and manhattan plots. bioRxiv 2014:005165.
Liberzon A, Birger C, Thorvaldsdottir H, Ghandi M, Mesirov JP, Tamayo P. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Syst 2015;1:417–25.
Chen EY, Tan CM, Kou Y, Duan Q, Wang Z, Meirelles GV, et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinforma. 2013;14:128.
Duan Q, Flynn C, Niepel M, Hafner M, Muhlich JL, Fernandez NF, et al. LINCS canvas browser: interactive web app to query, browse and interrogate LINCS L1000 gene expression signatures. Nucleic Acids Res. 2014;42:W449–60.
Ménard C, Hodes GE, Russo SJ. Pathogenesis of depression: insights from human and rodent studies. Neuroscience. 2016;321:138–62.
Hodes GE, Kana V, Menard C, Merad M, Russo SJ. Neuroimmune mechanisms of depression. Nat Neurosci. 2015;18:1386–93.
Altara R, Mallat Z, Booz GW, Zouein FA. The CXCL10/CXCR3 axis and cardiac inflammation: implications for immunotherapy to treat infectious and noninfectious diseases of the heart. J Immunol Res. 2016;2016:4396368.
Altara R, Manca M, Hessel MH, Gu Y, Van Vark LC, Akkerhuis KM, et al. CXCL10 is a circulating inflammatory marker in patients with advanced heart failure: a pilot study. J Cardiovascular Transl Res. 2016;9:302–14.
van den Borne P, Quax PH, Hoefer IE, Pasterkamp G. The multifaceted functions of CXCL10 in cardiovascular disease. Biomed Res Int. 2014;2014:893106.
Le Thuc O, Stobbe K, Cansell C, Nahon JL, Blondeau N, Rovere C. Hypothalamic inflammation and energy balance disruptions: spotlight on chemokines. Front Endocrinol (Lausanne). 2017;8:197.
Rotondi M, Chiovato L, Romagnani S, Serio M, Romagnani P. Role of chemokines in endocrine autoimmune diseases. Endocr Rev. 2007;28:492–520.
Bronger H, Kraeft S, Schwarz-Boeger U, Cerny C, Stockel A, Avril S, et al. Modulation of CXCR3 ligand secretion by prostaglandin E2 and cyclooxygenase inhibitors in human breast cancer. Breast Cancer Res. 2012;14:R30.
Koten K, Hirohata S, Miyoshi T, Ogawa H, Usui S, Shinohata R, et al. Serum interferon-gamma-inducible protein 10 level was increased in myocardial infarction patients, and negatively correlated with infarct size. Clin Biochem. 2008;41:30–7.
Xanthou G, Duchesnes CE, Williams TJ, Pease JE. CCR3 functional responses are regulated by both CXCR3 and its ligands CXCL9, CXCL10 and CXCL11. Eur J Immunol. 2003;33:2241–50.
Evans J, Salamonsen LA. Decidualized human endometrial stromal cells are sensors of hormone withdrawal in the menstrual inflammatory cascade. Biol Reprod. 2014;14:1–12.
Kanda N, Watanabe S. 17beta-estradiol inhibits the production of interferon-induced protein of 10 kDa by human keratinocytes. J Invest Dermatol. 2003;120:411–9.
Cerciat M, Unkila M, Garcia-Segura LM, Arevalo MA. Selective estrogen receptor modulators decrease the production of interleukin-6 and interferon-gamma-inducible protein-10 by astrocytes exposed to inflammatory challenge in vitro. Glia. 2010;58:93–102.
Sentman CL, Meadows SK, Wira CR, Eriksson M. Recruitment of uterine NK cells: induction of CXC chemokine ligands 10 and 11 in human endometrium by estradiol and progesterone. J Immunol. 2004;173:6760–6.
Muller C, Hennebert O, Morfin R. The native anti-glucocorticoid paradigm. J Steroid Biochem Mol Biol. 2006;100:95–105.
Rose KA, Stapleton G, Dott K, Kieny MP, Best R, Schwarz M, et al. Cyp7b, a novel brain cytochrome P450, catalyzes the synthesis of neurosteroids 7 -hydroxy dehydroepiandrosterone and 7 -hydroxy pregnenolone. Proc Natl Acad Sci. 1997;94:4925–30.
Pak TR, Chung WC, Hinds LR, Handa RJ. Estrogen receptor-beta mediates dihydrotestosterone-induced stimulation of the arginine vasopressin promoter in neuronal cells. Endocrinology. 2007;148:3371–82.
Handa RJ, Pak TR, Kudwa AE, Lund TD, Hinds L. An alternate pathway for androgen regulation of brain function: activation of estrogen receptor beta by the metabolite of dihydrotestosterone, 5alpha-androstane-3beta,17beta-diol. Horm Behav. 2008;53:741–52.
Maninger N, Wolkowitz OM, Reus VI, Epel ES, Mellon SH. Neurobiological and neuropsychiatric effects of dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEAS). Front Neuroendocrinol. 2009;30:65–91.
Schmidt PJ, Daly RC, Bloch M, Smith MJ, Danaceau MA, Simpson St. Clair L, et al. Dehydroepiandrosterone monotherapy in midlife-onset major and minor depression. Arch Gen Psychiatry. 2005;62:154–62.
Dor RB, Marx CE, Shampine LJ, Rubinow DR, Schmidt PJ. DHEA metabolism to the neurosteroid androsterone: a possible mechanism of DHEA’s antidepressant action. Psychopharmacology. 2015;232:3375–83.
Tang W, Eggertsen G, Chiang JY, Norlin M. Estrogen-mediated regulation of CYP7B1: a possible role for controlling DHEA levels in human tissues. J Steroid Biochem Mol Biol. 2006;100:42–51.
Morrison MF, Freeman EW, Lin H, Sammel MD. Higher DHEA-S (dehydroepiandrosterone sulfate) levels are associated with depressive symptoms during the menopausal transition: results from the PENN Ovarian Aging Study. Arch Women’s Ment Health. 2011;14:375–82.
Martin C, Bean R, Rose K, Habib F, Seckl J. cyp7b1 catalyses the 7alpha-hydroxylation of dehydroepiandrosterone and 25-hydroxycholesterol in rat prostate. Biochemical J. 2001;355:509–15.
Martin C, Ross M, Chapman KE, Andrew R, Bollina P, Seckl JR, et al. CYP7B generates a selective estrogen receptor β agonist in human prostate. J Clin Endocrinol Metab. 2004;89:2928–35.
Howard DM, Adams MJ, Clarke TK, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci. 2019;22:343–52.
Nagel M, Jansen PR, Stringer S, Watanabe K, de Leeuw CA, Bryois J, et al. Meta-analysis of genome-wide association studies for neuroticism in 449,484 individuals identifies novel genetic loci and pathways. Nat Genet. 2018;50:920–7.
Baselmans BML, Jansen R, Ip HF, van Dongen J, Abdellaoui A, van de Weijer MP, et al. Multivariate genome-wide analyses of the well-being spectrum. Nat Genet. 2019;51:445–51.
Slowik A, Lammerding L, Hoffmann S, Beyer C. Brain inflammasomes in stroke and depressive disorders: Regulation by oestrogen. J Neuroendocrinol. 2018;30. https://doi.org/10.1111/jne.12482.
Pfeilschifter J, Köditz R, Pfohl M, Schatz H. Changes in proinflammatory cytokine activity after menopause. Endocr Rev. 2002;23:90–119.
Dulos J, Verbraak E, Bagchus WM, Boots AM, Kaptein A. Severity of murine collagen-induced arthritis correlates with increased CYP7B activity: enhancement of dehydroepiandrosterone metabolism by interleukin-1beta. Arthritis Rheum 2004;50:3346–53.
Zare N, Khalifeh S, Khodagholi F, Shahamati SZ, Motamedi F, Maghsoudi N. Geldanamycin Reduces Abeta-Associated Anxiety and Depression, Concurrent with Autophagy Provocation. J Mol Neurosci 2015;57:317–24.
Binder EB. The role of FKBP5, a co-chaperone of the glucocorticoid receptor in the pathogenesis and therapy of affective and anxiety disorders. Psychoneuroendocrinology. 2009;34:S186–95.
Criado-Marrero M, Rein T, Binder EB, Porter JT, Koren J, 3rd., Blair LJ. Hsp90 and FKBP51: complex regulators of psychiatric diseases. Philos Trans R Soc Lond B Biol Sci 2018;373.
Tsai YC, Leu SY, Chen SY, Kung CW, Lee YM, Liu YP, et al. 17-DMAG, an Hsp90 inhibitor, ameliorates ovariectomy-induced obesity in rats. Life Sci. 2019;232:116672.
Dome P, Tombor L, Lazary J, Gonda X, Rihmer Z. Natural health products, dietary minerals and over-the-counter medications as add-on therapies to antidepressants in the treatment of major depressive disorder: a review. Brain Res Bull. 2019;146:51–78.
Abd-Rabo MM, Georgy GS, Saied NM, Hassan WA. Involvement of the serotonergic system and neuroplasticity in the antidepressant effect of curcumin in ovariectomized rats: Comparison with oestradiol and fluoxetine. Phytother Res. 2019;33:387–96.
Bhat A, Mahalakshmi AM, Ray B, Tuladhar S, Hediyal TA, Manthiannem E et al. Benefits of curcumin in brain disorders. Biofactors 2019;45:666–89.
Miodownik C, Lerner V, Kudkaeva N, Lerner PP, Pashinian A, Bersudsky Y, et al. Curcumin as add-on to antipsychotic treatment in patients with chronic schizophrenia: a randomized, double-blind, placebo-controlled study. Clin Neuropharmacol. 2019;42:117–22.
Ng QX, Koh SSH, Chan HW, Ho CYX. Clinical use of curcumin in depression: a meta-analysis. J Am Med Dir Assoc. 2017;18:503–8.
Caliskan M, Cusanovich DA, Ober C, Gilad Y. The effects of EBV transformation on gene expression levels and methylation profiles. Hum Mol Genet. 2011;20:1643–52.
Richards M, Rubinow DR, Daly RC, Schmidt PJ. Premenstrual symptoms and perimenopausal depression. Am J Psychiatry. 2006;163:133–7.
Honigberg MC, Zekavat SM, Aragam K, et al. Association of Premature Natural and Surgical Menopause With Incident Cardiovascular Disease. JAMA. 2019; https://doi.org/10.1001/jama.2019.19191. Online ahead of print.
Acknowledgements
We would like to thank Alan Meyers, Cheryl Marietta, Longina Akhtar, Allison Goff, and Maria Mazzu of NIH/NIAAA for their technical assistance and expertise in conducting this study. We would also like to thank Karla Thompson, Kai Shi, and Linda Schenkel of NIH/NIMH for their clinical support and data management. This research was supported by the Intramural Research Program of the NIMH and NIAAA NIH; NIMH Protocols 03-M-0175 (NCT00060736), 88-M-0131 (NCT00001231); NIMH Project ZIA MH002537; NIAAA Project ZIA AA000301.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rudzinskas, S., Hoffman, J.F., Martinez, P. et al. In vitro model of perimenopausal depression implicates steroid metabolic and proinflammatory genes. Mol Psychiatry 26, 3266–3276 (2021). https://doi.org/10.1038/s41380-020-00860-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-00860-x
This article is cited by
-
Intrinsically dysregulated cellular stress signaling genes and gene networks in postpartum depression
Molecular Psychiatry (2023)
-
The association between depression during perimenopause and progression of chronic conditions and multimorbidity: results from a Chinese prospective cohort
Archives of Women's Mental Health (2023)