Abstract
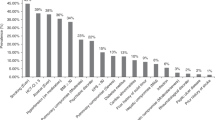
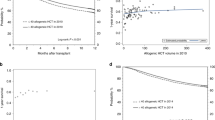
Racial and socioeconomic disparities impact outcomes after chemotherapy and limit access to allogeneic hematopoietic cell transplantation (HCT) in acute myeloid leukemia (AML), yet studies have yielded mixed results on the influence of disparities on post-HCT outcomes. Therefore, we studied 1024 adults with AML who underwent allogeneic HCT between 5/2006 and 10/2021 at a single large university-affiliated cancer center. Collected data included non-biologic and demographic characteristics (including race/ethnicity, marital status, distance traveled, and household size), transplant- and disease-related characteristics, and area-level and individual-level socioeconomic factors (i.e., area deprivation index and occupational status). After multivariable adjustment, no socioeconomic- or non-biologic factors were associated with non-relapse mortality (NRM), overall survival (OS), relapse-free survival (RFS), or relapse except being married (associated with improved NRM: hazard ratio [HR] = 0.7 [0.50–0.97]) and having no insurance (associated with worse OS: HR = 1.49 [1.05–2.12] and RFS: HR = 1.41 [1.00–1.98]). Despite a relatively racially homogenous cohort, Asian race was associated with improved NRM (HR = 0.47 [0.23–0.93]) and American Indian/Alaskan Native race was associated with higher relapse risk (HR = 2.45 [1.08–5.53]). In conclusion, in our retrospective analysis, socioeconomic-, demographic-, and non-biologic factors had limited impact on post-HCT outcomes in AML patients allografted in morphologic remission. Further research is needed to investigate disparities among HCT-eligible patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Original, de-identified data can be obtained via contacting the corresponding author (rwalter@fredhutch.org).
References
Döhner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood. 2022;140:1345–77.
Shimony S, Stahl M, Stone RM. Acute myeloid leukemia: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98:502–26.
DiNardo CD, Erba HP, Freeman SD, Wei AH. Acute myeloid leukaemia. Lancet. 2023;401:2073–86.
Byrne MM, Halman LJ, Koniaris LG, Cassileth PA, Rosenblatt JD, Cheung MC. Effects of poverty and race on outcomes in acute myeloid leukemia. Am J Clin Oncol. 2011;34:297–304.
Patel MI, Ma Y, Mitchell BS, Rhoads KF. Understanding disparities in leukemia: a national study. Cancer Causes Control. 2012;23:1831–7.
Patel MI, Ma Y, Mitchell BS, Rhoads KF. Age and genetics: how do prognostic factors at diagnosis explain disparities in acute myeloid leukemia? Am J Clin Oncol. 2015;38:159–64.
Borate UM, Mineishi S, Costa LJ. Nonbiological factors affecting survival in younger patients with acute myeloid leukemia. Cancer. 2015;121:3877–84.
Master S, Munker R, Shi Z, Mills G, Shi R. Insurance status and other non-biological factors predict outcomes in acute myelogenous leukemia: analysis of data from the National Cancer Database. Anticancer Res. 2016;36:4915–21.
Halpern AB, Culakova E, Walter RB, Lyman GH. Association of risk factors, mortality, and care costs of adults with acute myeloid leukemia with admission to the intensive care unit. JAMA Oncol. 2017;3:374–81.
Jabo B, Morgan JW, Martinez ME, Ghamsary M, Wieduwilt MJ. Sociodemographic disparities in chemotherapy and hematopoietic cell transplantation utilization among adult acute lymphoblastic and acute myeloid leukemia patients. PLoS One. 2017;12:e0174760.
Ho G, Jonas BA, Li Q, Brunson A, Wun T, Keegan THM. Early mortality and complications in hospitalized adult Californians with acute myeloid leukaemia. Br J Haematol. 2017;177:791–9.
Paulson K, Brazauskas R, Khera N, He N, Majhail N, Akpek G, et al. Inferior access to allogeneic transplant in disadvantaged populations: a Center for International Blood and Marrow Transplant Research analysis. Biol Blood Marrow Transpl. 2019;25:2086–90.
Mock J, Meyer C, Mau LW, Nguyen C, Arora P, Heron C, et al. Barriers to access to hematopoietic cell transplantation among patients with acute myeloid leukemia in Virginia. Transpl Cell Ther. 2021;27:869.e1–869.e9.
Hong S, Brazauskas R, Hebert KM, Ganguly S, Abdel-Azim H, Diaz MA, et al. Community health status and outcomes after allogeneic hematopoietic cell transplantation in the United States. Cancer. 2021;127:609–18.
Abraham IE, Rauscher GH, Patel AA, Pearse WB, Rajakumar P, Burkart M, et al. Structural racism is a mediator of disparities in acute myeloid leukemia outcomes. Blood. 2022;139:2212–26.
Baker KS, Davies SM, Majhail NS, Hassebroek A, Klein JP, Ballen KK, et al. Race and socioeconomic status influence outcomes of unrelated donor hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2009;15:1543–54.
Fu S, Rybicki L, Abounader D, Andresen S, Bolwell BJ, Dean R, et al. Association of socioeconomic status with long-term outcomes in 1-year survivors of allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 2015;50:1326–30.
Blue BJ, Brazauskas R, Chen K, Hashmi S, Lehmann LE, Wood WA, et al. Racial and socioeconomic disparities in long-term outcomes in ≥1 year allogeneic hematopoietic cell transplantation survivors: a CIBMTR analysis. Blood. 2021;138:3929.
Edgren JL, Ephraim A, Palmer JP, Kazemi M, MacKenzie T, Lansiga NF, et al. Impact of area deprivation index on clinical outcomes of adults with acute myeloid leukemia at a rural academic medical center. J Clin Oncol. 2023;41:e18615.
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140:1200–28.
Paras G, Morsink LM, Othus M, Milano F, Sandmaier BM, Zarling LC, et al. Conditioning intensity and peritransplant flow cytometric MRD dynamics in adult AML. Blood. 2022;139:1694–706.
Zarling LC, Othus M, Sandmaier BM, Milano F, Schoch G, Davis C, et al. Utility of the Treatment-Related Mortality (TRM) score to predict outcomes of adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Leukemia. 2022;36:1563–74.
Rodriguez-Arboli E, Orvain C, Othus M, Walter RB. Significance of measurable residual disease in adults with secondary acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 2022;57:1732–4.
Orvain C, Byelykh M, Othus M, Sandmaier BM, Schoch G, Davis C, et al. Relationship between pretransplantation nutritional status and outcome in adults with acute myelogenous leukemia undergoing allogeneic hematopoietic cell transplantation. Transpl Cell Ther. 2022;28:846.e1–846.e9.
Orvain C, Wilson JA, Fang M, Sandmaier BM, Rodríguez-Arbolí E, Wood BL, et al. Relative impact of residual cytogenetic abnormalities and flow cytometric measurable residual disease on outcome after allogeneic hematopoietic cell transplantation in adult acute myeloid leukemia. Haematologica. 2023;108:420–32.
Rodríguez-Arbolí E, Othus M, Orvain C, Zarling LC, Sandmaier BM, Milano F, et al. Contribution of measurable residual disease status to prediction accuracy of relapse and survival in adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Haematologica. 2023;108:273–7.
Orvain C, Rodríguez-Arbolí E, Othus M, Sandmaier BM, Deeg HJ, Appelbaum FR, et al. Association between prior cytotoxic therapy, antecedent hematologic disorder, and outcome after allogeneic hematopoietic cell transplantation in adult acute myeloid leukemia. Cancers. 2023;15:352.
Walter RB, Sandmaier BM, Othus M, Orvain C, Rodríguez-Arbolí E, Oshima MU, et al. Comparison of reduced intensity and nonmyeloablative conditioning for adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation in first or second remission. Bone Marrow Transpl. 2023;58:377–85.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Ganzeboom HBG, de Graaf PM, Treiman DJ. A standard international socio-economic index of occupational status. Soc Sci Res. 1992;21:1–56.
Hovanec J, Siemiatycki J, Conway DI, Olsson A, Stucker I, Guida F, et al. Lung cancer and socioeconomic status in a pooled analysis of case-control studies. PLoS One. 2018;13:e0192999.
Goldstein JS, Nastoupil LJ, Han X, Jemal A, Ward E, Flowers CR. Disparities in survival by insurance status in follicular lymphoma. Blood. 2018;132:1159–66.
Colton MD, Goulding D, Beltrami A, Cost C, Franklin A, Cockburn MG, et al. A U.S. population-based study of insurance disparities in cancer survival among adolescents and young adults. Cancer Med. 2019;8:4867–74.
Salem ME, Puccini A, Trufan SJ, Sha W, Kadakia KC, Hartley ML, et al. Impact of sociodemographic disparities and insurance status on survival of patients with early-onset colorectal cancer. Oncologist. 2021;26:e1730–e1741.
Majhail NS, Omondi NA, Denzen E, Murphy EA, Rizzo JD. Access to hematopoietic cell transplantation in the United States. Biol Blood Marrow Transpl. 2010;16:1070–5.
Srour SA, Machiorlatti M, Pierson NT, Bhutta UZ, Cherry M, Selby GB, et al. Impact of health care insurance status on treatment outcomes of acute myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2017;17:450–.e2.
Bade R, Banaszak LG, Osman F, Cabral P, Hassan A, Stepanovic A, et al. Neighborhood disadvantage, insurance status, and molecular profiling of patients with acute myeloid leukemia. Leuk Res. 2023;131:107326.
Albano JD, Ward E, Jemal A, Anderson R, Cokkinides VE, Murray T, et al. Cancer mortality in the United States by education level and race. J Natl Cancer Inst. 2007;99:1384–94.
Pan J, Ghimire S, Halloran M, Xu A, Zhan T, Keiffer G, et al. Socioeconomic influences on the treatment and outcomes of patients with acute myeloid leukemia: experience from an urban academic center. Blood. 2020;136:24.
Breems DA, Van Putten WLJ, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KBJ, Mellink CHM, et al. Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype. J Clin Oncol. 2008;26:4791–7.
Morsink LM, Othus M, Bezerra ED, Wood BL, Fang M, Sandmaier BM, et al. Impact of pre-transplant measurable residual disease on outcome of allogeneic hematopoietic cell transplantation in adult monosomal karyotype AML. Leukemia. 2020;34:1577–87.
Medeiros BC, Dunn TJ, Kohrt H, Coutre S, Gotlib J, Liedtke M, et al. Impact of distance to treatment center on the outcome of AML. Blood. 2010;116:4742.
Joshua TV, Rizzo JD, Zhang MJ, Hari PN, Kurian S, Pasquini M, et al. Access to hematopoietic stem cell transplantation: effect of race and sex. Cancer. 2010;116:3469–76.
Landry I. Racial disparities in hematopoietic stem cell transplant: a systematic review of the literature. Stem Cell Investig. 2021;8:24.
Bashey A, Zhang X, Morris LE, Holland HK, Bachier-Rodriguez L, Solomon SR, et al. Improved access to HCT with reduced racial disparities through integration with leukemia care and haploidentical donors. Blood Adv. 2023;7:3816–23.
Mukherjee A, Gooley T, Mielcarek M, Sandmaier BM, Doney K, Oshima MU, et al. Outcomes after hematopoietic cell transplantation among non-English- compared to English-speaking recipients. Bone Marrow Transpl. 2022;57:440–4.
Stubbins RJ, Stamenkovic M, Roy C, Rodrigo J, Chung S, Kuchenbauer FC, et al. Incidence and socioeconomic factors in older adults with acute myeloid leukaemia: real-world outcomes from a population-based cohort. Eur J Haematol. 2022;108:437–45.
Bradley CJ, Dahman B, Jin Y, Shickle LM, Ginder GD. Acute myeloid leukemia: how the uninsured fare. Cancer. 2011;117:4772–8.
Al-Ameri A, Anand A, Abdelfatah M, Kanaan Z, Hammonds T, Haller N, et al. Outcome of acute myeloid leukemia and high-risk myelodysplastic syndrome according to health insurance status. Clin Lymphoma Myeloma Leuk. 2014;14:509–13.
Huang LW, Sheng Y, Andreadis C, Logan AC, Mannis GN, Smith CC, et al. Functional status as measured by geriatric assessment predicts inferior survival in older allogeneic hematopoietic cell transplantation recipients. Biol Blood Marrow Transpl. 2020;26:189–96.
Zheng Z, Zhu Y, Li X, Hu W, Jiang J. Impact of marital status during diagnosis on cancer-caused specific survival in acute myeloid leukemia patients: a case-control and population-based study. Oncotarget. 2017;8:62666–80.
Dhakal P, Lyden E, Muir KLE, Al-Kadhimi ZS, Maness LJ, Gundabolu K, et al. Effects of distance from academic cancer center on overall survival of acute myeloid leukemia: retrospective analysis of treated patients. Clin Lymphoma Myeloma Leuk. 2020;20:e685–e690.
Morsink LM, Sandmaier BM, Othus M, Palmieri R, Granot N, Bezerra ED, et al. Conditioning intensity, pre-transplant flow cytometric measurable residual disease, and outcome in adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Cancers. 2020;12:2339.
Isaac KM, Reed DR, Desai RP, Williams E, Balkrishnan R, Keng MK, et al. Epidemiology of acute myeloid leukemia in Virginia: excellent survival outcomes for patients in rural Appalachia. Cancer Rep. 2021;4:e1354.
Conway DI, Hovanec J, Ahrens W, Ross A, Holcatova I, Lagiou P, et al. Occupational socioeconomic risk associations for head and neck cancer in Europe and South America: individual participant data analysis of pooled case-control studies within the INHANCE Consortium. J Epidemiol Community Health. 2021;75:779–87.
Auletta JJ, Sandmaier BM, Jensen E, Majhail NS, Knutson J, Nemecek E, et al. The ASTCT-NMDP ACCESS initiative: a collaboration to address and sustain equal outcomes for all across the hematopoietic cell transplantation and cellular therapy ecosystem. Transpl Cell Ther. 2022;28:802–9.
Acknowledgements
Research reported in this publication was supported by the National Cancer Institute/National Institutes of Health (NCI/NIH; Bethesda, MD, USA) via grants P01-CA078902, P01-CA018029, and P30-CA015704. RBW acknowledges support from the José Carreras/E. Donnall Thomas Endowed Chair for Cancer Research.
Funding
This work was supported by grants P01-CA078902, P01-CA018029, and P30-CA015704 from the National Cancer Institute/National Institutes of Health (NCI/NIH).
Author information
Authors and Affiliations
Contributions
CD and RSB contributed to the collection and assembly of data. MO conducted statistical analyses and participated in data interpretation and drafting of the manuscript. FM, BMS, and FRA contributed to the provision of study material, patient recruitment, and acquisition of data. RBW conceptualized and designed this study and participated in data analysis and interpretation and drafting of the final manuscript and oversaw all aspects of data collection. DJO conceptualized, collected, classified, extracted the data, helped design the study, and participated in data analysis, interpretation, and drafting of the manuscript. All authors revised the manuscript critically and gave final approval to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Olivieri, D.J., Othus, M., Orvain, C. et al. Impact of socioeconomic disparities on outcomes in adults undergoing allogeneic hematopoietic cell transplantation for acute myeloid leukemia. Leukemia 38, 865–876 (2024). https://doi.org/10.1038/s41375-024-02172-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-024-02172-3