Abstract
Therapy after failing response milestones in CML is controversial. Risks associated with comorbidities, drug toxicities or transplantation may preclude switching to another tyrosine kinase inhibitor (TKI) or other treatments. No information on long-term survival of failing patients is available. To systematically analyse survival after reaching, or not reaching, response milestones, 1342 patients from CML-study IV with newly diagnosed CML in chronic phase and regular molecular tests were studied. Landmark survival analyses were done by <0.1%, 0.1–1%, >1–10% and >10% BCR::ABL1IS at 3, 6, 12 and 24 months up to 14 years. 10- to 12-year survival of patients who failed the failure milestones (>10% BCR::ABL1IS at 6 months, >1% BCR::ABL1IS at 12 months) ranged around 80%, 10% less than in responding patients. These results suggest revision of milestones. Age (more or less than 60 years) had no major impact on survival differences, but on hazard ratios and CML-specific survival. Switching to alternative therapies, which was observed in 26.9% of the patients, did not change the main results. The data show that TKI-treated patients not reaching failure milestones still may derive benefit from continuing TKI-treatment and provide a basis for individualised decisions, if failing patients are confronted with risks of alternative treatments.
Similar content being viewed by others
Introduction
Controversies in CML management have surfaced regarding treatment after failing response milestones. Response milestones, since their definition and first publication by the European LeukemiaNet (ELN) in 2006 [1,2,3], have been a cornerstone for therapeutic decisions in CML-patients treated with tyrosine kinase inhibitors (TKI). Patients who reach less than 10% BCR::ABL1 by 3 months have high probabilities of a normal life expectancy [4, 5]. Also patients reaching response milestones at later times may still have excellent survival perspectives. Patients failing milestones (>10% BCR::ABL1 by 6 months, >1% BCR::ABL1 by 12 months or later) have a worse prognosis and are generally switched to an alternative TKI. In some patients switching may be problematic due to risks associated with drug toxicities, comorbidities or transplantation [6, 7]. In these patients, long-term observations have suggested that survival of patients failing milestones at 6 or 12 months and not switching TKI treatment was indeed worse than in patients who reached the milestones, but less than expected [8]. In CML-study IV, the difference of survival (OS) at 10 years between patients reaching, or not reaching, the warning milestone 1% BCR::ABL1 at 6 months was 6.4% across all treatment arms [9]. This implies that survival of patients not reaching, or failing, milestones may still be at a level permitting continuation of TKI-treatment, if there are concerns regarding risks of alternative treatments. It is the purpose of this analysis to follow up on these observations by systematically comparing TKI-treated CML patients in chronic phase (CP) who met, or did not meet, the various response milestones and quantifying their long-term survival.
Patients and methods
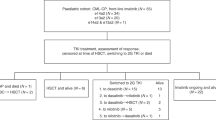
CML-study IV [9] is a randomised 5-arm study comparing newly diagnosed patients with CML in CP treated with imatinib 400 mg/day versus imatinib in combination with low-dose cytarabine or with interferon alpha simultaneously or consecutively versus imatinib 800 mg/day (n = 1536). Recruitment was from July 2002 through March 2012. Patients were followed for up to 14 years. No experimental arm turned out to be superior to standard imatinib at 400 mg/day, but the study showed high rates of stable deep molecular responses across study arms [10, 11]. For this analysis, only patients were selected who received imatinib as initial treatment and had regular molecular tests done (n = 1342).
In 372 patients (26.9%), imatinib, as foreseen in the study-protocol in the case of resistance or intolerance, was switched to another therapy, mostly to dasatinib and nilotinib. Seven patients were switched to bosutinib, 5 to ponatinib and 58 to more than one TKI. Seventy-eight patients were transplanted in first CP. Censoring at the time of switching did not change the main results of this analysis.
Definitions and end points: Definitions followed the ELN-recommendations [3]. OS was defined as the time between diagnosis and death resulting from any cause. Death unrelated to CML was defined as death without prior progression and unrelated to CML-therapy. Death due to CML was stratified according to the European treatment and outcome study-long-term-survival score [12]. All living patients were censored at the time of their last visit.
Cytogenetic and molecular analyses: Cytogenetic and molecular diagnostics were performed as described [4, 9, 13]. Testing for residual BCR::ABL1IS transcripts was done using quantitative reverse-transcription polymerase chain reaction with defined conversion factors for equivalence of tests according to International Scale (IS). The nomenclature followed the HGNC-recommendations [14]. Testing was restricted to patients expressing e13a2 and/or e14a2 transcripts. Equivalence of cytogenetic and molecular tests has been shown [15].
Statistical evaluations: Landmark analyses were carried out for four time points (3, 6, 12, and 24 months) to estimate conditional overall survival. Thus, all results have to be interpreted under the condition of still being alive at the respective landmark and therefore ignoring early mortality before the landmark. We performed two sensitivity analyses: Firstly, patients were censored at the time of treatment switch. This was done to assess the stability of the results presented here. Secondly, age was included as a metrical covariate into the models (instead of a dichotomisation at the 60 years cut-off). P values less than 0.05 were considered significant. This analysis was not specified in the study protocol; therefore, it must be seen as exploratory. All analyses were done in R 4.2.2 (R foundation). Landmark curves were estimated using the survival package. The differences between the conditional survival probabilities were plotted using the rms package.
Results
Response levels ≤0.1%, >0.1–1%, >1–10% and, >10% BCR::ABL1IS
To systematically analyse survival after reaching, or not reaching, response milestones, molecular and survival data from CML-study IV were used. Molecular tests were done in a total of 1342 imatinib-treated patients, of these in 805 patients at 3, in 891 at 6, in 861 at 12, and in 755 at 24 months after diagnosis. Of particular interest was the survival of patients who failed the failure milestones 10% BCR::ABL1IS at 6 months and 1% BCR::ABL1IS at 12 months. In clinical practice, the intermediary levels between >0.1% and 1% and between >1% and 10% BCR::ABL1IS may also be of interest.
Landmark survival analyses were carried out according to response levels of ≤0.1%, >0.1–1%, >1–10% and >10% BCR::ABL1 at 3, 6, 12 and 24 months (Fig. 1). Conditional survival after failing molecular response milestones was evaluated. Censoring for switching therapy did not change the main results (data not shown).
Patients reaching 0.1% and 1% BCR::ABL1IS at 3, 6, 12 and 24 months had a 10-year OS of close to 90%. Patients not reaching 10% BCR::ABL1IS at 3 and 6 months had a 10-year survival of 80% despite significant inferiority compared with patients reaching 0.1% and 1%. Patients not reaching 10% BCR::ABL1IS at 12 months had a marked increase in survival inferiority confirmed at 24 months. 10-year OS dropped to 55%. Likewise, 10-year survival of patients failing >1-10% remained stable around 90% until 12 months, but dropped to 60% at 24 months.
Whereas survival after reaching, or not reaching, >0.1–1% BCR::ABL1IS was not much different from survival after reaching 0.1% BCR::ABL1IS at all time points, survival after reaching, or not reaching, >1–10% BCR::ABL1 requires a more differentiated look. Landmark analyses up to month 12 show a survival similar to 1% BCR::ABL1IS. The landmark analysis at month 24 shows a survival similar to 1% BCR::ABL1IS up to year 6 when survival drops to the level of >10% BCR::ABL1IS.
Patients not reaching 10% BCR::ABLIS at 3 and 6 months had a significantly inferior conditional OS compared to those reaching 1% or 0.1% BCR::ABLIS, but a 10-year OS of about 80%. At the 12-months landmark, inferiority of conditional OS compared to patients with lower BCR::ABLIS levels increased markedly and 10-year OS dropped to 55%. The data suggest >10% BCR::ABLIS at 12 months as a more meaningful failure milestone compared to the 3- and 6-months landmarks which rather are warning milestones.
As the ELN recommendations use dichotomisations, we had a closer look on those (Fig. 2a) and the resulting differences in conditional overall survival (Fig. 2b).
a Landmark survival analyses (all patients) at 3, 6, 12 and 24 months according to reaching, or not reaching, molecular response levels at 0.1%, 1% and 10% BCR::ABL1IS, b calculated conditional survival differences according to molecular response levels of 0.1%, 1% and 10% BCR::ABL1IS at 3, 6, 12 and 24 months with confidence intervals.
Response level 0.1% BCR::ABL1IS
The survival differences (conditional overall survival, OS) between patients reaching, or not reaching, 0.1% BCR::ABL1 at 3 or 6 months (line 1 of Fig. 2a) were always below 10% in the first 10 years (see line 1 of Fig. 2b). We did not find significant differences regarding the hazard ratios. Conversely, not reaching, 0.1% BCR::ABL1IS at 12 and 24 months resulted in significant differences in hazard ratios of 0.63 (p = 0.010) respectively 0.43 (p < 0.001). Both indicate a warning. For the 12 months landmark, we observed constant, yet small differences in survival below 10% in the conditional probabilities. For the 24 months landmark, the differences between both groups reached 14.4% (pointwise 95%-confidence interval (CI): 4.5–24.5%) at 12 years.
Response level 1% BCR::ABL1IS
The conditional OS differences between patients reaching, or not reaching, 1% BCR::ABL1IS at 3 and 6 months were comparatively small with maxima of 10.7% and 8.2% both at about 12 years (line 2 of Fig. 2b). Not reaching 1% at 12 or 24 months is considered a failure. Here, the differences occurred earlier. For the 12 months landmark, the difference was already 10% at 3 years. For the 24 months landmark, the differences reached up to 29.0% (95%-CI: 12.8–45.2%). The hazard ratios for all four landmarks were significantly different from one and ranged from 0.26 (24 months, p < 0.001) to 0.63 (3 months, p = 0.031).
Response level >10% BCR::ABL1IS
The conditional OS differences between patients reaching or not reaching 10% BCR::ABL1IS at 3 months (line 3 of Fig. 2a) were again below 10% at maximum (7.8% at about 12 years). For the other landmarks, where not reaching 10% BCR::ABL1IS is considered a treatment failure, we found larger and earlier differences (Fig. 2b, line 3). These differences grew to about 30% for the 12- and 24-months landmarks, both at around 6 years. Similar to the 1% level, the hazard ratios for all four landmarks were significantly different from one and ranged from 0.22 (24 months, p < 0.001) to 0.61 (3 months, p = 0.015).
Slow responders and impact of residual disease
Figure 2a also shows that the proportions of patients failing the failure milestones 1% BCR::ABL1IS by 12 months and 10% BCR::ABL1IS by 6 months decreased during the observation interval from 18.8% at 12 months to 10.9% at 24 months at the 1% response level (line 2), and from 11.7% at 6 months to 7.5% at 12 months and further to 4.9% at 24 months at the 10% level (line 3) assuming that a substantial proportion of initially failing patients responded later (slow responders) [9]. It is apparent that survival is dependent on the amount of residual disease still present at subsequent time points. Not to have reached <1% BCR::ABL1IS at 12 months (line 2), or <10% at 6 and 12 months (line 3) is less impacting on OS than to have not reached this goal at 24 months.
Impact of age
The respective analyses for all patients stratified by age more or less than 60 years are shown in Fig. 3. Although the analyses show similar results according to reaching or not reaching milestones in both age groups, the underlying survival was rather different between younger and older patients translating to large differences in the hazard ratios for early death. Using Cox models with interaction effects, we found hazard ratios of 4.0 (95% CI: 2.0–8.1) for the younger patients, but only 0.9 (95%-CI: 0.4–1.8) for the elderly at 10% BCR::ABL1IS by 6 months. Similar differences were observed for the other milestones that indicated a failure, and, to a slightly smaller degree, for the warnings. The reasons for early death in the younger patients were mostly CML-related, whereas the elderly primarily died of other reasons as determined earlier [12]. In a sensitivity analysis, age was considered a metrical covariate. As the main conclusions regarding the landmarks were the same as before, we decided to stay with the dichotomisation for the sake of the visualisation.
Impact of early cytogenetic response on survival
When cytogenetic analyses were used to define milestones, similar survival results were seen as with the corresponding molecular tests (Fig. 4). Cytogenetic analyses were available in 518 patients at 6 months, in 502 patients at 12 months and in 321 patients at 24 months. The differences in conditional OS between patients achieving complete, partial, or less than partial cytogenetic remissions were not significant at months 6 and 12. At 24 months patients that did not achieve at least a partial cytogenetic remission showed an inferior conditional OS compared to both other groups.
Discussion
Our data show that CML-patients derive benefit from TKI treatment even if milestones defining failure are not reached. TKI-treated patients not reaching the failure milestones 1% BCR::ABL1IS by 12 months and 10% BCR::ABL1IS by 6 months still have a 10-to-12-year conditional OS of 80% which is 10% less than that of responders. This data may help decide on treatment continuation when an alternative treatment carries risks due to patients‘ comorbidities, adverse drug effects or transplantation. Treatment can be individualised and adapted to patients‘ needs by taking survival under continued TKI-treatment and risk of the new treatment into consideration. In view of these data definitions of failure and warning milestones may have to be revised.
Our data compare well with the 60% 15-year OS observed with 131 CP-patients who did not reach MMR within 2 years of TKI treatment [16], but patients not reaching at least partial cytogenetic remission within 24 months (19 of 321) may have a poorer survival. To verify a survival difference between these subgroups, a comparison between studies would be needed that takes risk profiles, cytogenetics [17] and other prognostic factors into consideration.
If the 10% BCR::ABL1IS response level is not reached by 12 or 24 months, the survival difference to responders increases to about 30% which still may be an acceptable outcome in the absence of reasonable alternatives.
The impact of intermediate response levels >1–10% BCR:ABL1IS on survival shows the limitations of a dichotomous evaluation approach and points to the need of individualised interpretation.
The strength of the data comes from the number of patients, the study protocol of CML-study IV [9] asking for regular molecular analyses of all patients over the entire study duration, and from the follow up of up to 14 years.
The survival differences between patients reaching and not reaching the failure milestones confirm the value of the response milestones [1, 2], but failure milestones may have to be adapted to the new more mature data.
If the data were analysed according to age more or less than 60 years, differences between the age groups were noted. Younger patients not reaching the failure milestones were more likely to die early, mostly of progression, whereas reaching the milestones is less important for the elderly who died predominantly of other reasons [12].
A limitation of the data is that imatinib was the primary TKI in CML-study IV. As differences between patients with and without failures or warnings were similar when patients were censored at the time of switching, we can conclude that the milestones were reasonable in both scenarios. The design of CML study IV precludes a comparison of imatinib to 2nd generation TKI after treatment failure.
The molecular data are confirmed by cytogenetic data. Cytogenetics were increasingly replaced by molecular tests during the study, but as evident from Fig. 4, there still were sufficient patients with cytogenetic analyses available to show that results with cytogenetically and molecularly defined milestones were similar.
In conclusion, TKI-treated patients not reaching failure milestones still may derive benefit from continuing TKI-treatment with acceptable survival probabilities showing that TKI have a beneficial effect even if milestones are not reached. The definition of milestones may have to be revised. Individualisation of therapy according to comorbidity, effectivity and treatment goals is desirable.
Data availability
Authors are committed to sharing access to patient-level data and supporting clinical documents with qualified external researchers upon request. These requests are reviewed and approved by an independent review panel based on scientific merit. All data provided are anonymized to respect the privacy of patients who have participated in the trial consistent with applicable laws and regulations.
References
Baccarani M, Saglio G, Goldman J, Hochhaus A, Simonsson B, Appelbaum F, et al. Evolving concepts in the management of chronic myeloid leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood. 2006;108:1809–20.
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122:872–84.
Hochhaus A, Baccarani M, Silver RT, Schiffer C, Apperley JF, Cervantes F, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34:966–84.
Hanfstein B, Müller MC, Hehlmann R, Erben P, Lauseker M, Fabarius A, et al. Early molecular and cytogenetic response is predictive for long-term progression-free and overall survival in chronic myeloid leukemia (CML). Leukemia. 2012;26:2096–102.
Marin D, Ibrahim AR, Lucas C, Gerrard G, Wang L, Szydlo RM, et al. Assessment of BCR-ABL1 transcript levels at 3 months is the only requirement for predicting outcome for patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors. J Clin Oncol. 2012;30:232.
Steegmann JL, Baccarani M, Breccia M, Casado LF, García-Gutiérrez V, Hochhaus A, et al. European LeukemiaNet recommendations for the management and avoidance of adverse events of treatment in chronic myeloid leukaemia. Leukemia. 2016;30:1648–71.
Saußele S, Krauß MP, Hehlmann R, Lauseker M, Proetel U, Kalmanti L, et al. Impact of comorbidities on overall survival in patients with chronic myeloid leukemia: results of the randomized CML study IV. Blood. 2015;126:42–49.
Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2020 update on diagnosis, therapy and monitoring. Am J Hematol. 2020;95:691–709.
Hehlmann R, Lauseker M, Saußele S, Pfirrmann M, Krause S, Kolb HJ, et al. Assessment of imatinib as first-line treatment of chronic myeloid leukemia: 10-year survival results of the randomized CML study IV and impact of non-CML determinants. Leukemia. 2017;31:2398–406.
Hehlmann R, Müller MC, Lauseker M, Hanfstein B, Fabarius A, Schreiber A, et al. Deep molecular response is reached by the majority of patients treated with imatinib, predicts survival, and is achieved more quickly by optimized high-dose imatinib: results from the randomized CML-study IV. J Clin Oncol. 2014;32:415–23.
Kalmanti L, Saußele S, Lauseker M, Müller MC, Dietz CT, Heinrich L, et al. Safety and efficacy of imatinib in CML over a period of 10 years: data from the randomized CML-study IV. Leukemia. 2015;29:1123–32.
Pfirrmann M, Baccarani M, Saußele S, Guilhot J, Cervantes F, Ossenkoppele G, et al. Prognosis of long-term survival considering disease-specific death in patients with chronic myeloid leukemia. Leukemia. 2016;30:48–56.
Cross NCP, White HE, Müller MC, Saglio G, Hochhaus A. Standardized definitions of molecular response in chronic myeloid leukemia. Leukemia. 2012;26:2172–5.
Bruford EA, Antonescu CR, Carroll AJ, Chinnaiyan A, Cree IA, Cross NC, et al. HUGO Gene Nomenclature Committee (HGNC) recommendations for the designation of gene fusions. Leukemia. 2021;35:3040–3.
Lauseker M, Hanfstein B, Haferlach C, Schnittger S, Pfirrmann M, Fabarius A, et al. Equivalence of BCR-ABL transcript levels with complete cytogenetic remission in patients with chronic myeloid leukemia in chronic phase. J Cancer Res Clin Oncol. 2014;140:1965–9.
Bidikian A, Jabbour E, Issa GC, Short NJ, Sasaki K, Kantarjian H. Chronic myeloid leukemia without major molecular response after 2 years of treatment with tyrosine kinase inhibitor. Am J Hematol. 2023;98:639–44.
Hehlmann R, Voskanyan A, Lauseker M, Pfirrmann M, Kalmanti L, Rinaldetti S, et al. High-risk additional chromosomal abnormalities at low blast counts herald death by CML. Leukemia. 2020;34:2074–86.
Acknowledgements
We thank Hagop Kantarjian for suggesting this analysis, Johannes Hehlmann for assistance and all participants of SAKK and the German CML Study Group for contributing patients to CML Study IV as previously published [9].
Funding
Funded by the ELN Foundation. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
ML performed the statistical analyses and contributed to writing the manuscript. RH designed the study and wrote the manuscript. AH provided the molecular analyses. SS provided patient data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
AH: Research support from Novartis, BMS, Pfizer and Incyte. SS: Research support from Novartis, BMS, and Incyte, Honoraria from Novartis, Pfizer, Roche and Incyte.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lauseker, M., Hehlmann, R., Hochhaus, A. et al. Survival with chronic myeloid leukaemia after failing milestones. Leukemia 37, 2231–2236 (2023). https://doi.org/10.1038/s41375-023-02028-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-023-02028-2