Abstract
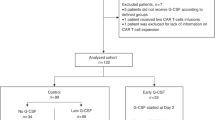
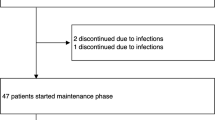
Polyethylene glycol (PEG)-asparaginase (pegaspargase) is a key agent in chemotherapy for acute lymphoblastic leukemia (ALL), but recipients frequently experience allergic reactions. We hypothesized that by decreasing antibody-producing CD20-positive B cells, rituximab may reduce these reactions. Children and adolescents (aged 1–18 years) with newly diagnosed B-ALL treated on the St. Jude Total XVII study were randomized to induction therapy with or without rituximab on day 3 (cohort 1) or on days 6 and 24 (cohort 2). Patient clinical demographics, CD20 expression, minimal residual disease (MRD), rituximab reactions, pegaspargase allergy, anti-pegaspargase antibodies, and pancreatitis were evaluated. Thirty-five patients received rituximab and 37 did not. Among the 35 recipients, 16 (45.7%) experienced a grade 2 or higher reaction to rituximab. There were no differences between recipients and non-recipients in the incidence of pegaspargase reactions (P > 0.999), anti-pegaspargase antibodies (P = 0.327), or pancreatitis (P = 0.480). CD20 expression on day 8 was significantly lower in rituximab recipients (P < 0.001), but there were no differences in MRD levels on day 8, 15, or at the end of induction. Rituximab administration during induction in pediatric patients with B-ALL was associated with a high incidence of infusion reactions with no significant decrease in pegaspargase allergies, anti-pegaspargase antibodies, or MRD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hunger SP, Mullighan CG. Acute lymphoblastic leukemia in children. N Engl J Med. 2015;373:1541–52.
Inaba H, Greaves M, Mullighan CG. Acute lymphoblastic leukaemia. Lancet. 2013;381:1943–55.
Hijiya N, van der Sluis IM. Asparaginase-associated toxicity in children with acute lymphoblastic leukemia. Leuk Lymphoma. 2016;57:748–57.
Sassen SD, Mathot RA, Pieters R, Kloos RQ, de Haas V, Kaspers GJ, et al. Population pharmacokinetics of intravenous Erwinia asparaginase in pediatric acute lymphoblastic leukemia patients. Haematologica. 2017;102:552–61.
Liu Y, Smith CA, Panetta JC, Yang W, Thompson LE, Counts JP, et al. Antibodies predict pegaspargase allergic reactions and failure of rechallenge. J Clin Oncol. 2019;37:2051–61.
Woods D, Winchester K, Towerman A, Gettinger K, Carey C, Timmermann K, et al. From the children’s oncology group: evidence-based recommendations for PEG-asparaginase nurse monitoring, hypersensitivity reaction management, and patient/family education. J Pediatr Oncol Nurs. 2017;34:387–96.
Angiolillo AL, Schore RJ, Devidas M, Borowitz MJ, Carroll AJ, Gastier-Foster JM, et al. Pharmacokinetic and pharmacodynamic properties of calaspargase pegol Escherichia coli L-asparaginase in the treatment of patients with acute lymphoblastic leukemia: results from Children’s Oncology Group Study AALL07P4. J Clin Oncol. 2014;32:3874–82.
Vrooman LM, Blonquist TM, Stevenson KE, Supko JG, Hunt SK, Cronholm SM, et al. Efficacy and toxicity of pegaspargase and calaspargase pegol in childhood acute lymphoblastic leukemia: results of DFCI 11-001. J Clin Oncol. 2021;39:3496–505.
Ribrag V, Koscielny S, Bosq J, Leguay T, Casasnovas O, Fornecker LM, et al. Rituximab and dose-dense chemotherapy for adults with Burkitt’s lymphoma: a randomised, controlled, open-label, phase 3 trial. Lancet. 2016;387:2402–11.
Gottenberg JE, Guillevin L, Lambotte O, Combe B, Allanore Y, Cantagrel A, et al. Tolerance and short term efficacy of rituximab in 43 patients with systemic autoimmune diseases. Ann Rheum Dis. 2005;64:913–20.
Maury S, Chevret S, Thomas X, Heim D, Leguay T, Huguet F, et al. Rituximab in B-lineage adult acute lymphoblastic leukemia. N Engl J Med. 2016;375:1044–53.
Jeha S, Pei D, Choi J, Cheng C, Sandlund JT, Coustan-Smith E, et al. Improved CNS control of childhood acute lymphoblastic leukemia without cranial irradiation: st jude total therapy study 16. J Clin Oncol. 2019;37:3377–91.
Pauley JL, Panetta JC, Crews KR, Pei D, Cheng C, McCormick J, et al. Between-course targeting of methotrexate exposure using pharmacokinetically guided dosage adjustments. Cancer Chemother Pharmacol. 2013;72:369–78.
Pui CH, Pei D, Coustan-Smith E, Jeha S, Cheng C, Bowman WP, et al. Clinical utility of sequential minimal residual disease measurements in the context of risk-based therapy in childhood acute lymphoblastic leukaemia: a prospective study. Lancet Oncol. 2015;16:465–74.
Gupta S, Maude SL, O’Brien MM, Rau RE, McNeer JL. How the COG is approaching the high-risk patient with ALL: incorporation of immunotherapy into frontline treatment. Clin Lymphoma Myeloma Leuk. 2020;20:S8–S11.
Inaba H, Pui CH. Advances in the diagnosis and treatment of pediatric acute lymphoblastic leukemia. J Clin Med. 2021;10:1926.
Henriksen LT, Harila-Saari A, Ruud E, Abrahamsson J, Pruunsild K, Vaitkeviciene G, et al. PEG-asparaginase allergy in children with acute lymphoblastic leukemia in the NOPHO ALL2008 protocol. Pediatr Blood Cancer. 2015;62:427–33.
Burke MJ, Devidas M, Maloney K, Angiolillo A, Schore R, Dunsmore K, et al. Severe pegaspargase hypersensitivity reaction rates (grade >/=3) with intravenous infusion vs. intramuscular injection: analysis of 54,280 doses administered to 16,534 patients on children’s oncology group (COG) clinical trials. Leuk Lymphoma. 2018;59:1624–33.
Silverman LB, Stevenson KE, O’Brien JE, Asselin BL, Barr RD, Clavell L, et al. Long-term results of Dana-Farber Cancer Institute ALL Consortium protocols for children with newly diagnosed acute lymphoblastic leukemia (1985-2000). Leukemia. 2010;24:320–34.
Gupta S, Wang C, Raetz EA, Schore R, Salzer WL, Larsen EC, et al. Impact of asparaginase discontinuation on outcome in childhood acute lymphoblastic leukemia: a report from the children’s oncology group. J Clin Oncol. 2020;38:1897–905.
Karol SE, Pei D, Smith CA, Liu Y, Yang W, Kornegay NM, et al. Comprehensive analysis of dose intensity of acute lymphoblastic leukemia chemotherapy. Haematologica. 2022;107:371–80.
Kawedia JD, Liu C, Pei D, Cheng C, Fernandez CA, Howard SC, et al. Dexamethasone exposure and asparaginase antibodies affect relapse risk in acute lymphoblastic leukemia. Blood. 2012;119:1658–64.
Taylor RP, Lindorfer MA. Drug insight: the mechanism of action of rituximab in autoimmune disease-the immune complex decoy hypothesis. Nat Clin Pract Rheumatol. 2007;3:86–95.
Huhn D, von Schilling C, Wilhelm M, Ho AD, Hallek M, Kuse R, et al. Rituximab therapy of patients with B-cell chronic lymphocytic leukemia. Blood. 2001;98:1326–31.
Marks DI, Kirkwood AA, Rowntree CJ, Aguiar M, Bailey KE, Beaton B, et al. Addition of four doses of rituximab to standard induction chemotherapy in adult patients with precursor B-cell acute lymphoblastic leukaemia (UKALL14): a phase 3, multicentre, randomised controlled trial. Lancet Haematol. 2022;9:e262–e75.
Wong JT, Long A. Rituximab hypersensitivity: evaluation, desensitization, and potential mechanisms. J Allergy Clin Immunol Pract. 2017;5:1564–71.
Minard-Colin V, Auperin A, Pillon M, Burke GAA, Barkauskas DA, Wheatley K, et al. Rituximab for high-risk, mature B-cell non-hodgkin’s lymphoma in children. N Engl J Med. 2020;382:2207–19.
Dworzak MN, Schumich A, Printz D, Potschger U, Husak Z, Attarbaschi A, et al. CD20 up-regulation in pediatric B-cell precursor acute lymphoblastic leukemia during induction treatment: setting the stage for anti-CD20 directed immunotherapy. Blood. 2008;112:3982–8.
Campana D, Pui CH. Minimal residual disease-guided therapy in childhood acute lymphoblastic leukemia. Blood. 2017;129:1913–8.
Acknowledgements
The authors thank Keith A. Laycock, PhD, ELS, for scientific editing of the manuscript. This work was supported by National Institutes of Health (NIH) grants P30CA021765, R01CA142665, and R35GM141947; by the American Lebanese Syrian Associated Charities (ALSAC); and by Sevier Pharmaceuticals, LLC. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
KH, AMM, and HI contributed to writing and critically revising the manuscript, extracting and analyzing data, and interpreting results. JKC was responsible for reviewing the leukemia pathology. YZ and CC were responsible for statistical design and analysis. NHB, SJ, SEK, RCR, CHP, and HI contributed patients and to the design of the study. CGM, JJY, MVR, CHP, and HI were responsible for study conceptualization, study design, and critical review of the manuscript. HI was the principal investigator for the trial, and CHP was the co-principal investigator.
Corresponding author
Ethics declarations
Competing interests
This work was funded partially by Servier Pharmaceuticals, LLC. The company had no role in the study design, the collection or analysis of data, or the decision to publish.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hoshitsuki, K., Zhou, Y., Miller, A.M. et al. Rituximab administration in pediatric patients with newly diagnosed acute lymphoblastic leukemia. Leukemia 37, 1782–1791 (2023). https://doi.org/10.1038/s41375-023-01992-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-023-01992-z