Abstract
In acute myeloid leukaemia (AML) RUNX1 mutation is characterised by certain clinicopathological features with poor prognosis and adverse risk by the European LeukemiaNet recommendation. Though initially considered as provisional category, the recent World Health Organisation (WHO) classification of 2022 removed RUNX1-mutated AML from the unique entity. However, the significance of RUNX1 mutation in paediatric AML remains unclear. We retrospectively analysed a German cohort of 488 paediatric patients with de novo AML, enroled in the AMLR12 or AMLR17 registry of the AML-BFM Study Group (Essen, Germany). A total of 23 paediatric AML patients (4.7%) harboured RUNX1 mutations, 18 of which (78%) had RUNX1 mutation at initial diagnosis. RUNX1 mutations were associated with older age, male gender, number of coexisting alterations and presence of FLT3-ITD but mutually exclusive of KRAS, KIT and NPM1 mutation. RUNX1 mutations did not prognostically impact overall or event-free survival. Response rates did not differ between patients with and without RUNX1 mutations. This comprehensive study, comprising the largest analysis of RUNX1 mutation in a paediatric cohort to date, reveals distinct but not unique clinicopathologic features, with no prognostic significance of RUNX1-mutated paediatric AML. These results broaden the perspective on the relevance of RUNX1 alterations in leukaemogenesis in AML.
Similar content being viewed by others
Introduction
Acute myeloid leukaemia (AML) is a genetically heterogeneous disease. Analyses of genetic aberrations helped to unravel a complex genetic landscape and improved our knowledge of AML pathogenesis, leading to refined, risk-adapted treatment allocation [1,2,3,4]. In paediatric AML, optimising genetic and response-dependent risk-group stratification, allocating high-risk patients to receive allogeneic stem cell transplantation (SCT) in first complete remission (CR) allows survival rates of about 80% [4]. Notably, frequency of several prognostic biomarkers differs greatly between adult and paediatric AML, suggesting a different ontogeny in childhood AML [5,6,7]. Moreover, distinct age-specific genetic profiles point at a unique biology in paediatric AML and implicate the necessity for precise, age-tailored diagnostic and therapeutic approaches [7,8,9,10,11].
Intragenic mutations of the runt-related transcription factor-1 (RUNX1) have been associated with distinct clinical and genetic features as well as inferior prognosis in adult AML [12,13,14,15,16]. These results prompted the inclusion of “AML with mutated RUNX1” as new provisional entity of the World Health Organisation (WHO) classification as part of the revision in 2016 [17, 18]. Due to lack of specificity, this was rejected by the latest 5th edition of the WHO classification [19]. Considering the independent association with unfavourable risk, the European LeukemiaNet (ELN) recommendation classified RUNX1-mutated AML into the adverse risk category [20, 21].
The RUNX1 transcription factor, encoded on chromosome 21q22.3, is crucial for early lineage differentiation and indispensable for definite hematopoiesis [22, 23]. In AML, the core-binding factor (CBF) family member RUNX1 is involved in the recurrent chromosomal aberrations t(8;21), leading to the leukaemia-initiating RUNX1::RUNX1T1 fusion, predicting favourable prognosis [24]. Native RUNX1 was found to critically promote leukaemogenesis in t(8;21) AML [25].
Intragenic mutations of the RUNX1 gene were preliminary reported in MDS, secondary and therapy-related AML, radiation exposed myelodysplastic syndrome (MDS) and AML [26,27,28]. Inherited RUNX1 mutation were found to cause familial platelet disorder (FPD) with a propensity to MDS and AML [29,30,31]. To date, the impact of the RUNX1 mutation in paediatric AML has remained unclear. There are only a few controversial reports, with a limited data and number of patients on the RUNX1 mutation in paediatric AML [32,33,34,35].
This retrospective study elucidates the pathological and clinical implication of RUNX1 mutation in a substantial paediatric AML cohort. By targeted sequencing, we assess concomitant genetic changes and their impact in development of paediatric AML.
Methods
Study participants
A paediatric cohort of 488 patients (0–18 years), diagnosed with de-novo AML between 2015 and 2021 was included. The cohort represents a German paediatric AML population, excluding patients with acute promyelocytic leukaemia (FAB M3), Down syndrome (ML-DS), secondary and treatment-related AML. All included patients were enroled and treated either according to the AMLR12 registry (EudraCT number: 2013-000018-39) or AMLR17 registry (DRKS number: DRKS00013030) of the AML-BFM Study Group. The ethical committees and institutional review boards of the university hospital of Hannover and Essen approved both registries according to the declaration of Helsinki. Informed consent was obtained from patients and their legal guardians prior to treatment participation. Initial and follow-up diagnostics including morphological, immunophenotypic and molecular genetic testing were performed centrally by the German AML-BFM reference laboratory Essen according to standard procedures. Analysis for classical cytogenetics and fluorescence in situ hybridisation (FISH) were carried out by the Institute of Human Genetics in Hannover Medical School. The treatment recommendations of analysed registries included similar cytarabine- and daunorubicin-based induction chemotherapy [36]. Depending on the risk stratification intensive chemotherapy, maintenance therapy and allogeneic SCT were performed by indication.
Genetic analyses
Primary bone marrow or peripheral blood samples from paediatric patients were subjected to molecular genetic screening at the time of diagnosis by next generation sequencing (NGS) using the TruSight® Myeloid Panel (Illumina, San Diego, California, USA). Using the standard NGS technology, the mutational screening included 54 different leukaemia-associated genes (Supplementary Table S2b). Sequencing was performed on the Illumina MiSeq™DX System (Illumina, San Diego, California, USA). Analysis was conducted using the SOPHIA DDMTM software (Sophia Genetics, Switzerland). RUNX1 mutations were confirmed by PCR and subsequent Sanger sequencing.
To check for germline mutations, paired remission samples of RUNX1-mutated AML patients, harbouring a VAF above 30 were analysed by PCR to detect the respective RUNX1 mutation.
RNA sequencing was analysed using the TruSight® RNA Fusion Panel (Illumina, San Diego, CA, USA) according to manufacturer’s recommendations. Classical karyotyping was performed following the International System for Human Cytogenetic (International System of Cytogenetic Nomenclature; ISCN 1995–2013).
Statistical analysis
Patient characteristics between groups were compared using Pearson chi-square or Fisher’s exact test for categorical variables and Mann–Whitney U test for continuous variables. A p-value of less than 0.05 was considered to indicate statistical significance. Survival analysis included Overall survival (OS), defined as the time from diagnosis to death or last follow-up, Event-free survival (EFS), defined as the time from diagnosis to relapse, secondary malignancy, death, or the time of last follow-up. Kaplan–Meier curves were calculated for OS and EFS. The log-rank test was obtained to compare survival differences. To identify prognostic variables, Cox-models were used for univariate and multivariate regression analyses. Results were reported as hazard risk ratios with 95% confidence intervals (CI) indicated. Following complexity and dimensionality reduction to a reasonable, recommended number of 50 principal components (PCs), the unsupervised clustered data were visualised using t-distributed stochastic neighbourhood embedding (t-SNE) according to recent recommendations [37] using Seaborn and Plotly Express Python visualisation libraries based on matplotlib (Python 3.9.13, Jupyter Notebook 6.4.12). Statistical analysis was conducted using SPSS software version 28.0 (Chicago, IL, USA) and R software version 4.0.2 (http://www.Rproject.org). Illustrations were generated using Graphpad Prism™ 8.3, R software version 4.0.2, Python 3.9.13 and DOG 2.0 [38].
Results
Characteristics of RUNX1 mutations
In 23 patients (4.7%), 27 RUNX1 mutations (OMIM No. 151385) were detected of which 24 mutations were distinct from each other (Fig. 1, Supplementary Table S1a, b). Within the RUNX1-mutated cohort, 18 out of 23 patients presented at least one RUNX1 mutation at initial diagnosis (78%). Among eight patient-matched paired diagnosis and relapse samples, RUNX1 mutations were detectable only at relapse in five cases (Supplementary Tables S1a and S6). The same RUNX1 mutation was present in two patients at both time points. In one case, RUNX1 mutation was undetectable at relapse. Comparing the paired samples in this case, two additional mutations were lost from initial diagnosis to relapse. Regarding morphologic, immunophenotypic and cytogenetic criteria the early relapse resembled the initial diagnosis, indicating that the loss of the RUNX1 mutation occurred during the process of clonal evolution (Supplementary Tables S6).
Gene diagram depicting the structure of RUNX1 (Ref Seq NM_001001890). RUNX1 mutations are visualised and assigned to the corresponding locus. Six mutations were detected in five relapsed samples (black line). RHD Runt homology domain, TAD transactivation domain, RD repression domain. Protein in the top row and mRNA of isoform 1b, variant 2 in the bottom row (NM_001001890.3, reference sequence).
Considering all 27 detected RUNX1 coding sequence alterations, the majority were characterised as frameshift (48.1%), followed by nine missense (33.3%) and two different deletion-insertions (delins) in five cases (18.5%). Four patients were found to have two different RUNX1 mutations, three of which shared the same combinatorial pattern (p.A208_M209delinsDR, p.R206C), including the sample with RUNX1 mutation only at diagnosis. Among the five relapsed samples harbouring RUNX1 mutation only at relapse, three frameshifts, two missenses, and the repeatedly occurring mutational combination were found. Considering the distribution on the RUNX1 gene (Fig. 1), one mutation was allocated to exon 2, six mutations to exon 3, one to exon 4, seven to exon 5.1, (including p.A208_M209delinsDR, p.R206C), one to exon 5.2 and five to exon 6. Mutations were assigned to different functional groups, whilst the largest proportion of eleven mutations (40.7%) was clustered in the runt homology domain (RHD), two mutations (7.4%) were in the transactivation domain (TAD), four (14.8%) in the repression domain (RD) and eight (29.6%) mutations were located between the TAD and RD. One frameshift mutation was localised at C-terminal to the RD. In the RHD all three different kinds of mutations were discovered, whereas in the TAD and RD only frameshift mutation occurred. To exclude germline mutations and proof the somatic origins, RUNX1-mutated AML with a variant allele frequency (VAF) > 30% were selected for germline-testing. Since one of which never reached remission, samples at remission were available for nine patients. The suspected RUNX1 mutation was not detectable in any of the remission samples, confirming the somatic origin.
Association with clinical characteristics
Compared to RUNX1 wildtype (wt) (n = 470), patients with RUNX1-mutated de novo AML (n = 18) were significantly older at diagnosis (11.7 [2–17] vs. 8.3 [0–18] years, p = 0.02), (Table 1). Age curve of mutated patients is clearly shifted to adolescent age (>12 years), whilst there is a relatively uniform age-distribution in RUNX1 wt-patients, (Fig. 2). RUNX1 mutations tends to associate with male gender (male: 50 vs. 72%, p = 0.06). In terms of the AML morphology, RUNX1-mutated were more likely to be myelomonocytic compared to non-mutated samples (FAB M4, 33 vs. 17%, p = 0.1), followed by AML with minimal differentiation and without maturation (FAB M0, 6 vs. 1%, p = 0.26; FAB M1, 22 vs. 17%, p = 0.29). In contrast, the number of samples evaluated as acute monocytic leukaemia (FAB M5, 11 vs. 23%, p = 0.39) and AML with maturation (FAB M2, 17 vs. 22%, p = 0.78) were lower in the mutated cohort. None of the six patients with acute erythroid leukaemia harboured RUNX1 mutation. The RUNX1-mutated patient samples showed no significant difference in terms of median haemoglobin level, white blood cell, platelet, bone marrow and peripheral blast count at diagnosis. Involvement of the central nervous system (CNS) at diagnosis was almost equal in both groups.
Association with genetic characteristics
Cytogenetic data were available for all 18 RUNX1-mutated and 460 (98%) RUNX1 wt-patients (Table 2). Prevalence of normal and complex karyotype did not differ significantly between RUNX1-mutated and wt-cohort (44 vs. 26%, p = 0.11 and 22 vs. 17%, p = 0.55, respectively). Frequent cytogenetic aberrations accompanying the RUNX1 mutation were t(8;21) and trisomy +8, showing almost equal distribution (17 vs. 12%, p = 0.7 and 11 vs. 15%, p = 1.0). RUNX1 mutation tends to associate with −7/7q, (17 vs. 5%, p = 0.08). RUNX1 mutation did not co-occur together with KMT2A rearrangement (KMT2Ar), (0 vs. 19%, p = 0.04). The recurrent aberration inv(16)/t(16;16) was present in one patient sample (6 vs. 7%, p = 0.82). In addition, RUNX1 mutations did not occur together with other recurrent cytogenetic changes, namely the t(6;9), −5/5q, trisomy +11 or +13.
Addressing the mutational spectrum of co-occurring mutations, all 18 RUNX1-mutated and 470 wt-cases were evaluated for 53 additional AML-related genes assayed by targeted NGS (Fig. 3, Supplementary Table S2b). The average number of concomitant aberrations was significantly increased in RUNX1-mutated patient cohort (2.4, range 0–5) compared with the wt-cohort (1.7, range 0–6), (p = 0.02). Whereas the largest proportion of wt-patients (32%) had one detectable mutation, most RUNX1-mutated cases (50 %) harboured two additional, accompanying mutations.
a Frequency of molecular genetic mutations as listed on the x-axis in RUNX1-mutated patients (red bars) and wt-patients (blue bars). b Chord diagram displaying the distribution and mutational pattern of molecular genetic aberrations in RUNX1-wt cohort (b.1) and RUNX1-mutated cohort (b.2) in childhood AML. SR SRSF2, U2 U2AF1, SF SF3B1, ZR ZRSR2, KD KDM6A, NU NUP98::NSD1, KM KMT2A, ST STAG2, SM SMC1A, RAD RAD21, SMC SMC3, DN DNMT3A, BR BRAF, JA JAK2; PD PDGFRA, NO NOTCH1, MY MYD88, MP MPL, PT PTEN, SE SETBP1, AT ATRX, FB FBXW7.
RUNX1 mutation was correlated with the presence of FLT3 with internal tandem duplication (FLT3-ITD), being the most common co-occurring genetic aberration in the RUNX1-mutated cohort (56 vs. 22%, p = 0.002). The second most frequent RUNX1 accompanying mutation was in Wilms-tumor1 (WT1) gene, which was found in 4 of the 18 RUNX1-mutated cases (22 vs. 12%, p = 0.26). Whereas NRAS mutations occurred as second most common mutations in wt-patients, it was rarely found in RUNX1-mutated samples (6 vs. 21%, p = 0.14). CEBPA aberrations were detected in two RUNX1-mutated samples and were slightly more commonly mutated in the RUNX1-mutated cohort (11 vs. 6%, p = 0.28). Upon further differentiation of all 27 CEBPA-mutant samples, CEBPA aberration was biallelic in 15 patients, including two RUNX1-mutated (11 vs. 3%, p = 0.11). RUNX1 mutations were mutually exclusive of recurrent alterations in KRAS, KIT and NPM1 (p = .024, p = 0.4 and p = 0.39). Other mutations studied were more evenly distributed in both cohorts, with no tendency for a specific correlation.
Genetic mutations detected by NGS were assigned to different functional groups according to the functional categorisation of the mutated genes [2] (Supplementary Table S2c). The largest proportion was attributed to activated signalling, which made up 41% among RUNX1-mutated and 50% among wt-cases. Mutations affiliated to epigenetic regulator occurred more frequently together with RUNX1 mutation (22 vs 10%). Alterations of transcription factors, excluding RUNX1, were the second most common aberrations among wt-cases, showing comparable frequency in RUNX1-mutated and wt-cohort (13 vs. 15%). Aberrations of tumour suppressor genes were evenly distribution between RUNX1-mutated and wt-cohorts (16 vs. 12%). Together, there was no clear association between RUNX1 mutations and any of the other genetic groups. Accordingly, RUNX1-mutated samples projected scattered without showing definable, separate clustering in the t-SNE plot, which contrasts with the well-known distinct entity of CBF in AML (Supplementary Fig. S1).
Impact of RUNX1 mutations on response, outcome and survival
Response to therapy was comparable between RUNX1-mutated and wt-cases (94 vs. 84% achieved CR, p = 0.33). None of RUNX1-mutated, but 20 of wt-cases suffered early death (4%) (Supplementary Table S3). The proportion of patients undergoing SCT in first CR was evenly distributed between the RUNX1-mutated, and wt-cohorts (23 vs. 22%). Likewise, number of patients transplanted as salvage therapy were almost equal in both groups (Supplementary Table S3).
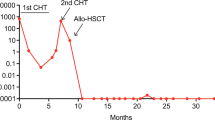
OS and EFS were compared between patients with and without RUNX1 mutation (Fig. 4). In the entire cohort, the mean follow-up time of survival for patients alive was 5.9 ± 1.3 years (95% CI, 5.7–6.1). RUNX1 mutations had no significant effect on 5-year OS (93 ± 6.1 vs. 78 ± 2.2%, p = .12) and EFS (55 ± 13.9 vs. 59 ± 2.6%, p = .53). Frequency of the associated outcome parameter death and relapse were comparable between RUNX1-mutated and wt-cohorts (Supplementary Table S3).
Univariable regression analysis revealed no strong prognostic impact of RUNX1 mutation on OS (HR 0.43, p = 0.16) or EFS (HR 0.78, p = 0.55; Supplementary Table S4a). Multivariable models were created following adjustment for age, risk groups, FLT3-ITD, SCT and additional mutations (Supplementary Table S4b). RUNX1 mutation was not predictive to experience any event (HR 1.4, p = 0.39) nor of death (HR 4.2 p = 0.17). Since RUNX1 mutation was significantly associated with FLT3-ITD, increased patient age and number of mutations, subgroup analyses were performed to separately assess the relative prognostic relevance of RUNX1 mutation within these subgroups (Supplementary Table S5a). In the presence of FLT3-ITD, concomitant RUNX1 mutation did not impact OS (80 ± 17.9 vs. 78.8 ± 4.3, p = 0.42) or EFS (57.1 ± 16.4 vs. 56.6 ± 5.5, p = 0.68). In children younger than 12-years at diagnosis, RUNX1-mutated and wt patients showed comparable outcome (OS, 63.5 ± 16.9 vs. 77.7 ± 2.8, p = 0.58, EFS, 53.3 ± 17.3 vs. 62.3 ± 3.2, p = 0.95). In older paediatric patients (>12-years) RUNX1 mutation tends to associate with increased OS (100 ± 0 vs. 76.9 ± 3.5, p = 0.11), but not EFS (71.6 ± 14 vs. 54.5 ± 4.3, p = 0.36). Among patients harbouring more than two additional genetic alterations, RUNX1 mutation neither impact OS (90.9 ± 8.7 vs. 74.9 ± 5.0, p = 0.24), nor EFS (54.2 ± 16.2 vs. 49.3 ± 6.3, p = 0.48). When separately assessing impact of RUNX1 mutation in the context of SCT, patients with and without RUNX1 mutation, receiving SCT in first CR achieved comparable survival rates (OS, 75.0 ± 21.7 vs. 77.0 ± 4.4, p = 0.91, EFS 60 ± 21.9 vs. 57.1 ± 5.2, p = 0.98). Separate survival analyses, conducted for standard-, intermediate-, and high-risk groups revealed no strong difference of survival by RUNX1 mutation for risk-associated groups (Supplementary Table S5b). Together, in our paediatric cohort, RUNX1 mutation showed no prognostic significance.
Discussion
AML with RUNX1 mutation was considered as adverse-risk AML by the ELN and new provisional entity in the 2016 WHO classification given its characteristic clinicopathologic features and inferior outcome in adult AML [13, 16,17,18, 20]. In 2022, the preliminary stand-alone entity was removed due to lack of specificity [19]. In paediatric AML, large-scale sequencing studies suggested a distinct genetic landscape with clinical significance [7, 8, 11]. However, impact of RUNX1-mutated AML in paediatrics has largely remained obscure.
This retrospective study evaluates RUNX1 mutations in the largest paediatric cohort to date. Prevalence of the studied RUNX1-mutated paediatric AML cases is relatively low (3.7%). In comparison, in adult AML, a frequency of ~5–13% has been reported, with highest prevalence when including elderly patients (>60 years) [13, 16, 39]. Accordingly, reported prevalence of RUNX1 mutation was lower in younger patients and an association with patients age has been shown before [12,13,14, 33]. Likewise, in the paediatric cohort studied here, RUNX1 mutation was found more frequently in older children. Consistent with previous findings our results confirm a positive correlation to male gender in paediatrics. Unlike previous studies [13, 15, 33], we could not detect a correlation with minimally differentiated AML (FAB M0). In AML with M0 phenotype, biallelic RUNX1 mutations have been frequently described, where in case of heterozygous RUNX1 mutation, a deletion on the other allele is suggested to result in a functional inactivation of RUNX1 [31, 40]. However, this could not be confirmed in the current paediatric cohort, since there was only one heterozygous, biallelic RUNX1 mutation in a FAB M4 sample, without evidence of further biallelic mutation.
The mutational spectrum revealed a higher proportion of frameshift mutations and a clustering of missense mutations at the N’-terminus, especially in RHD. A similar distribution of RUNX1 mutation according to different functional domains and clustered mutations at the N´-terminus was previously reported in adult AML, whilst Greif et al. detect a greater proportion of missense mutation in cytogenetically normal AML [14,15,16]. Unexpectedly, in three patients we found a recurrent combination of the same missense and delins mutational pattern, which were not described before. These mutations had a low VAF (<10) and were only detectable at diagnosis or relapse in paired patient-matched samples, suggesting high mutational instability. Prevalence and implication of germline mutations in AML samples with RUNX1 mutation has been discussed controversially [41, 42]. In our study, there was no evidence of germline mutations, which may not seem surprising given the reported wide age range for AML onset in FPD [30, 31]. Interestingly, in the current cohort, a child with Down Syndrome related AML (ML-DS) who was excluded a-priori from the analysis, harboured the same RUNX1 mutation in remission, suggesting a germline mutation (data not shown). To our knowledge, except for the increased dosing effect of RUNX1 in ML-DS, no increased prevalence and no specific mechanism of interaction between altered RUNX1 and GATA1 has been described [31, 43,44,45].
Regarding cytogenetics, we could not affirm an inverse correlation of RUNX1 mutation and the recurrent CBF-defining abnormalities t(8;21) and inv(16)/t(16;16). Consistent with reports in adult AML, RUNX1 mutation weakly associated with the unbalanced abnormality −7/7q [13, 16], which has also been described as myelodysplasia related aberration. However, none of the analysed paediatric AML patients had a known history of MDS and further cytogenetic alterations related to myelodysplasia, including −5/5q, were almost absent in the evaluated cohort. In contrast to previous reports, RUNX1 mutation did not correlate with trisomy +8 [16, 39, 46], trisomy +13 was even absent in the analysed RUNX1-mutated paediatric cohort [13, 15, 47]. Distribution of normal and complex karyotype was largely balanced, which in part, agrees with results of a small Japanese paediatric AML cohort, where 6 out of 11 RUNX1-mutated patients had normal karyotype, whilst +8 and complex KT were present in one patient [33]. Ultimately, RUNX1-mutated paediatric AML did not show a distinct cytogenetic pattern, particularly with respect to the overlap with prognostically favourable subgroup CBF-AML, arguing against RUNX1 mutation as a distinct AML type in paediatrics.
RUNX1-mutated AML completely lacks KMT2Ar, indicating that RUNX1 mutation most probably do not contribute to leukaemogenesis in KMT2Ar AML in paediatrics. In fact, in AML mouse models harbouring KMT2Ar, RUNX1 activity mediated leukaemic cell growth and survival [48, 49]. Similarly, RUNX1 was determined as transcriptional target in KMT2A::AFF1, previously known as MLL::AF4, AML by Wilkinson et al. [49], suggesting that RUNX1 activity cooperates with KMT2Ar to promote AML development. Considering the determined exclusivity of RUNX1 mutation and KMT2Ar, this could also be true for paediatric AML.
Given that RUNX1 mutations alone are highly unlikely to be sufficient to cause complete leukaemic transformation [50], investigation of cooperating mutations is required to further elucidate leukaemic mechanisms in RUNX1-mutated AML. Increased number of co-occurring mutations indicates a more complex genetic evolution of RUNX1-mutated AML, requiring a broad range of additional mutations.
FLT3-ITD was the most common co-occurring mutation and significantly associated with RUNX1 mutation in paediatric AML, which may suggest cooperativity between these two mutations. An early report indicated a link between RUNX1 mutation and FLT3-ITD contributing to leukaemogenesis in AML M0, in which RUNX1 mutations predominated [51]. In comparison, FLT3-ITD frequently occurred in RUNX1-mutated adult AML, albeit evenly distributed and without correlation with RUNX1 mutation [15, 39], supporting the notion of a cooperation between RUNX1 mutation and FLT3-ITD, which may be specific to paediatric AML [52]. RUNX1 mutations were almost exclusive of alterations involved in other activated-signalling pathways, namely NRAS, KRAS and KIT, which in contrast, were relatively common in the wt-cohort. These results may point at a reassortment in the functional group of activated-signalling, shifted towards FLT3-ITD, supporting the suggestion, that RUNX1 mutation preferably contributes to leukaemogenesis by cooperating with the activating FLT3-ITD, instead of other activating pathways in paediatric AML. Despite the fact that FLT3-ITD has long been known to associate with poor prognosis [53, 54], in the present study, co-occurrence of FLT3-ITD with RUNX1 mutation did not affect outcomes in paediatric AML, which is consistent with results in adult AML [15].
Despite the small number of patients, which makes the accurate assessment of additional genetic associations more difficult, concurrent genetic aberrations occurred more frequently in epigenetic modifiers, with a trend towards BCORL1, EZH2, and KDM6A. A propensity for association was noted for spliceosome U2AF1, whereas other spliceosome-related genetic aberrations were absent in RUNX1-mutated paediatric AML. In contrast, RUNX1-mutated adult AML has been associated with mutations in the spliceosome and cohesion complex, in addition to epigenetic modifiers [13], consistent with those reported in high-risk MDS [55, 56]. This further underlines the heterogeneity in biological properties between adults and paediatric AML.
Consistent with previous studies [12,13,14,15, 57], mutations of the transcription factor NPM1 were completely absent in the RUNX1-mutated paediatric cohort. NPM1 mutation is considered as founding genetic event in AML with certain biological and clinical features, warranting its own entity [52, 58]. The exclusivity of NPM1 and RUNX1 mutation in AML might suggest that RUNX1 mutation shares a similar role with NPM1 mutations in leukaemia development. In two cases we observed that RUNX1 mutation overlaps with double mutated CEBPA in paediatrics, contradicting the notion that RUNX1-mutated AML represents a distinct entity. Thus, according to the results of this cohort, previously reported characteristic features, favouring the concept of considering RUNX1-mutated AML as a distinct entity [13, 17], cannot be confirmed in paediatric AML since RUNX1 mutation lacks these mutational features and overlaps with AML defining mutational patterns.
In the recent ELN-recommendation, RUNX1 mutation was stated as a late event in leukaemia development [21], which contradicts earlier studies, considering RUNX1 mutations as early events in leukemognenesis [15, 50]. The observed inconsistency of RUNX1 mutations in six out of eight paired diagnosis-relapse samples in this paediatric cohort, indicates instability, suggesting that RUNX1 mutation rather is a late genetic event contributing to advanced clonal evolution. Moreover, the detected high number of additional aberrations accompanying RUNX1 mutation and the observed overlap with the AML-causing events CBF-fusions or NPM1 mutation in the assessed paediatric patients, further support the concept that RUNX1 mutations are more likely to contribute to the late-stage leukaemia development.
In this study, RUNX1 mutation did not show a prognostic significance for outcomes and survival. These results contrast with previous data on RUNX1 mutation in AML, indicating that RUNX1 is a negative prognosticator [12,13,14, 33]. Since some reports combined primary and secondary AML, Quesada et al. assessed the prognostic impact of RUNX1-mutated de novo AML according to the WHO definition and detected no differences in outcome [57], which is concordant with our findings in primary paediatric AML. In addition, Greif et al. proved negative prognostic significance in elderly (> 60 years) cytogenetically normal AML, whereas this could not be confirmed for younger patients [14, 16], suggesting age-dependency of the poor prognostic impact of RUNX1 mutation. This observation could be strengthened by our results, where RUNX1 mutation showed no predictive relevance in paediatric AML. However, we did not observe a strong difference when separately assessing age-depending prognostic impact of RUNX1 mutation in paediatric patients. Since the survival was not affected by RUNX1 mutation in different risk groups, there seems to be no relevance for including RUNX1 mutations in the risk stratification of paediatric AML. In terms of indication for SCT, survival was comparable in patients with and without SCT in first CR, suggesting that the presence of RUNX1 mutation does not require modification in eligibility criteria in paediatric AML.
This analysis uncovers the impact of RUNX1 mutation in a well characterised paediatric AML cohort and provides new insights into its clinicopathological relevance. Although this study evaluates RUNX1 mutations in the largest paediatric cohort studied to date, analyses are still limited due to small sample sizes for some analysis-subgroups and the retrospective dataset, necessitating further validation to confirm these observations.
In conclusion, RUNX1 mutations did not impact outcomes in this paediatric AML cohort, suggesting a clinical impact that differs from that reported in adult AML. Importantly, RUNX1 mutations lacked clinical characteristics and genetic features, which would justify a separate WHO entity. Therefore, the previously stated provisional WHO entity ‘RUNX1 mutated AML’, is not appropriate in paediatric AML. The results of this study agree with the recently published fifth edition of the WHO classification which removed RUNX1 mutations as distinct entities in AML [19].
Code availability
The code used for the t-SNE analysis and visualisation can be provided upon request.
Data availability
A detailed data sharing statement is provided in the Supplementary Materials.
References
Marceau-Renaut A, Duployez N, Ducourneau B, Labopin M, Petit A, Rousseau A, et al. Molecular profiling defines distinct prognostic subgroups in childhood AML: a report from the French ELAM02 study group. HemaSphere. 2018;2:e31.
Ley TJ, Miller C, Ding L, Raphael BJ, Mungall AJ, Robertson AG, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368:2059–74.
Duncavage EJ, Schroeder MC, O’Laughlin M, Wilson R, MacMillan S, Bohannon A, et al. Genome sequencing as an alternative to cytogenetic analysis in myeloid cancers. N Engl J Med. 2021;384:924–35.
Rasche M, Zimmermann M, Borschel L, Bourquin J-P, Dworzak M, Klingebiel T, et al. Successes and challenges in the treatment of pediatric acute myeloid leukemia: a retrospective analysis of the AML-BFM trials from 1987 to 2012. Leukemia. 2018;32:2167–77.
Liang D-C, Liu H-C, Yang C-P, Jaing T-H, Hung I-J, Yeh T-C, et al. Cooperating gene mutations in childhood acute myeloid leukemia with special reference on mutations of ASXL1, TET2, IDH1, IDH2, and DNMT3A. Blood. 2013;121:2988–95.
Ho PA, Kutny MA, Alonzo TA, Gerbing RB, Joaquin J, Raimondi SC, et al. Leukemic mutations in the methylation-associated genes DNMT3A and IDH2 are rare events in pediatric AML: a report from the Children’s Oncology Group. Pediatr blood cancer. 2011;57:204–9.
Bolouri H, Farrar JE, Triche T, Ries RE, Lim EL, Alonzo TA, et al. The molecular landscape of pediatric acute myeloid leukemia reveals recurrent structural alterations and age-specific mutational interactions. Nat Med. 2018;24:103–12.
Farrar JE, Schuback HL, Ries RE, Wai D, Hampton OA, Trevino LR, et al. Genomic profiling of pediatric acute myeloid leukemia reveals a changing mutational landscape from disease diagnosis to relapse. Cancer Res. 2016;76:2197–205.
Hara Y, Shiba N, Yamato G, Ohki K, Tabuchi K, Sotomatsu M, et al. Patients aged less than 3 years with acute myeloid leukaemia characterize a molecularly and clinically distinct subgroup. Br J Haematol. 2020;188:528–39.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374:2209–21.
Walter C, Schneider M, Neuhoff N, von, Hanenberg H, Reinhardt D, Rasche M. Mutational landscape of pediatric acute myeloid leukemia: a report of the AML-BFM study group with a targeted NGS approach in 525 patients integrating de novo, relapsed and secondary AML. Blood. 2019;134:1398.
Mendler JH, Maharry K, Radmacher MD, Mrózek K, Becker H, Metzeler KH, et al. RUNX1 mutations are associated with poor outcome in younger and older patients with cytogenetically normal acute myeloid leukemia and with distinct gene and MicroRNA expression signatures. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30:3109–18.
Gaidzik VI, Teleanu V, Papaemmanuil E, Weber D, Paschka P, Hahn J, et al. RUNX1 mutations in acute myeloid leukemia are associated with distinct clinico-pathologic and genetic features. Leukemia. 2016;30:2160–8.
Greif PA, Konstandin NP, Metzeler KH, Herold T, Pasalic Z, Ksienzyk B, et al. RUNX1 mutations in cytogenetically normal acute myeloid leukemia are associated with a poor prognosis and up-regulation of lymphoid genes. Haematologica. 2012;97:1909–15.
Schnittger S, Dicker F, Kern W, Wendland N, Sundermann J, Alpermann T, et al. RUNX1 mutations are frequent in de novo AML with noncomplex karyotype and confer an unfavorable prognosis. Blood. 2011;117:2348–57.
Gaidzik VI, Bullinger L, Schlenk RF, Zimmermann AS, Röck J, Paschka P, et al. RUNX1 mutations in acute myeloid leukemia: results from a comprehensive genetic and clinical analysis from the AML study group. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29:1364–72.
Haferlach T, Stengel A, Eckstein S, Perglerová K, Alpermann T, Kern W, et al. The new provisional WHO entity ‘RUNX1 mutated AML’ shows specific genetics but no prognostic influence of dysplasia. Leukemia. 2016;30:2109–12.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405.
Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36:1703–19.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Döhner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood. 2022;140:1345–77.
Swiers G, Bruijn M, de, Speck NA. Hematopoietic stem cell emergence in the conceptus and the role of Runx1. Int J Dev Biol. 2010;54:1151–63.
Okuda T, van Deursen J, Hiebert SW, Grosveld G, Downing JR. AML1, the target of multiple chromosomal translocations in human leukemia, is essential for normal fetal liver hematopoiesis. Cell. 1996;84:321–30.
Peterson LF, Zhang D-E. The 8;21 translocation in leukemogenesis. Oncogene. 2004;23:4255–62.
Ben-Ami O, Friedman D, Leshkowitz D, Goldenberg D, Orlovsky K, Pencovich N, et al. Addiction of t(8;21) and inv(16) acute myeloid leukemia to native RUNX1. Cell Rep. 2013;4:1131–43.
Harada H, Harada Y, Tanaka H, Kimura A, Inaba T. Implications of somatic mutations in the AML1 gene in radiation-associated and therapy-related myelodysplastic syndrome/acute myeloid leukemia. Blood. 2003;101:673–80.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J. Mutations of AML1 are common in therapy-related myelodysplasia following therapy with alkylating agents and are significantly associated with deletion or loss of chromosome arm 7q and with subsequent leukemic transformation. Blood. 2004;104:1474–81.
Harada H, Harada Y, Niimi H, Kyo T, Kimura A, Inaba T. High incidence of somatic mutations in the AML1/RUNX1 gene in myelodysplastic syndrome and low blast percentage myeloid leukemia with myelodysplasia. Blood. 2004;103:2316–24.
Song WJ, Sullivan MG, Legare RD, Hutchings S, Tan X, Kufrin D, et al. Haploinsufficiency of CBFA2 causes familial thrombocytopenia with propensity to develop acute myelogenous leukaemia. Nat Genet. 1999;23:166–75.
Owen CJ, Toze CL, Koochin A, Forrest DL, Smith CA, Stevens JM, et al. Five new pedigrees with inherited RUNX1 mutations causing familial platelet disorder with propensity to myeloid malignancy. Blood. 2008;112:4639–45.
Preudhomme C, Warot-Loze D, Roumier C, Grardel-Duflos N, Garand R, Lai JL, et al. High incidence of biallelic point mutations in the Runt domain of the AML1/PEBP2αB gene in Mo acute myeloid leukemia and in myeloid malignancies with acquired trisomy 21. Blood. 2000;96:2862–9.
Kutny MA, Alonzo TA, Gerbing RB, Miller K, Ho P, Heerema NA, et al. RUNX1 mutations in pediatric AML: a report from the children’s oncology group. Blood. 2009;114:2614.
Yamato G, Shiba N, Yoshida K, Hara Y, Shiraishi Y, Ohki K, et al. RUNX1 mutations in pediatric acute myeloid leukemia are associated with distinct genetic features and an inferior prognosis. Blood. 2018;131:2266–70.
Al-Kzayer LFY, Sakashita K, Al-Jadiry MF, Al-Hadad SA, Le Uyen TN, Liu T, et al. Frequent coexistence of RAS mutations in RUNX1-mutated acute myeloid leukemia in Arab Asian children. Pediatr Blood Cancer. 2014;61:1980–5.
Taketani T, Taki T, Takita J, Tsuchida M, Hanada R, Hongo T, et al. AML1/RUNX1 mutations are infrequent, but related to AML-M0, acquired trisomy 21, and leukemic transformation in pediatric hematologic malignancies. Genes Chromosomes Cancer. 2003;38:1–7.
Reinhardt D, Antoniou E, Waack K. Pediatric acute myeloid leukemia-past, present, and future. J Clin Med. 2022;11:504.
Kobak D, Berens P. The art of using t-SNE for single-cell transcriptomics. Nat Commun. 2019;10:5416.
Ren J, Wen L, Gao X, Jin C, Xue Y, Yao X. DOG 1.0: illustrator of protein domain structures. Cell Res. 2009;19:271–3.
Tang J-L, Hou H-A, Chen C-Y, Liu C-Y, Chou W-C, Tseng M-H, et al. AML1/RUNX1 mutations in 470 adult patients with de novo acute myeloid leukemia: prognostic implication and interaction with other gene alterations. Blood. 2009;114:5352–61.
Roumier C, Eclache V, Imbert M, Davi F, Macintyre E, Garand R, et al. M0 AML, clinical and biologic features of the disease, including AML1 gene mutations: a report of 59 cases by the Groupe Français d’Hématologie Cellulaire (GFHC) and the Groupe Français de Cytogénétique Hématologique (GFCH). Blood. 2003;101:1277–83.
Simon L, Spinella J-F, Yao C-Y, Lavallée V-P, Boivin I, Boucher G, et al. High frequency of germline RUNX1 mutations in patients with RUNX1-mutated AML. Blood. 2020;135:1882–6.
Ernst MPT, Kavelaars FG, Löwenberg B, Valk PJM. Raaijmakers MHGP: RUNX1 germline variants in RUNX1-mutant AML: how frequent? Blood. 2021;137:1428–31.
Grimm J, Heckl D, Klusmann J-H. Molecular mechanisms of the genetic predisposition to acute megakaryoblastic leukemia in infants with down syndrome. Front Oncol. 2021;11:636633.
Mateos MK, Barbaric D, Byatt S-A, Sutton R, Marshall GM. Down syndrome and leukemia: insights into leukemogenesis and translational targets. Transl Pediatrics. 2015;4:76–92.
Langebrake C, Klusmann J-H, Wortmann K, Kolar M, Puhlmann U, Reinhardt D. Concomitant aberrant overexpression of RUNX1 and NCAM in regenerating bone marrow of myeloid leukemia of Down’s syndrome. Haematologica. 2006;91:1473–80.
Wang K, Zhou F, Cai X, Chao H, Zhang R, Chen S. Mutational landscape of patients with acute myeloid leukemia or myelodysplastic syndromes in the context of RUNX1 mutation. Hematol Am Soc Hematol Educ Program. 2020;25:211–8.
Dicker F, Haferlach C, Kern W, Haferlach T, Schnittger S. Trisomy 13 is strongly associated with AML1/RUNX1 mutations and increased FLT3 expression in acute myeloid leukemia. Blood. 2007;110:1308–16.
Goyama S, Schibler J, Cunningham L, Zhang Y, Rao Y, Nishimoto N, et al. Transcription factor RUNX1 promotes survival of acute myeloid leukemia cells. J Clin Investig. 2013;123:3876–88.
Wilkinson AC, Ballabio E, Geng H, North P, Tapia M, Kerry J, et al. RUNX1 is a key target in t(4;11) leukemias that contributes to gene activation through an AF4-MLL complex interaction. Cell Rep. 2013;3:116–27.
Osato M. Point mutations in the RUNX1/AML1 gene: another actor in RUNX leukemia. Oncogene. 2004;23:4284–96.
Matsuno N, Osato M, Yamashita N, Yanagida M, Nanri T, Fukushima T, et al. Dual mutations in the AML1 and FLT3 genes are associated with leukemogenesis in acute myeloblastic leukemia of the M0 subtype. Leukemia. 2003;17:2492–9.
Falini B, Martelli MP, Bolli N, Sportoletti P, Liso A, Tiacci E, et al. Acute myeloid leukemia with mutated nucleophosmin (NPM1): is it a distinct entity? Blood. 2011;117:1109–20.
Thiede C, Steudel C, Mohr B, Schaich M, Schäkel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–35.
Zwaan CM, Meshinchi S, Radich JP, Veerman AJP, Huismans DR, Munske L, et al. FLT3 internal tandem duplication in 234 children with acute myeloid leukemia: prognostic significance and relation to cellular drug resistance. Blood. 2003;102:2387–94.
Papaemmanuil E, Gerstung M, Malcovati L, Tauro S, Gundem G, van Loo P, et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122:3616–27. quiz 3699
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28:241–7.
Quesada AE, Montalban-Bravo G, Luthra R, Patel KP, Sasaki K, Bueso-Ramos CE, et al. Clinico-pathologic characteristics and outcomes of the World Health Organization (WHO) provisional entity de novo acute myeloid leukemia with mutated RUNX1. Mod Pathol. 2020;33:1678–89.
Martelli MP, Pettirossi V, Thiede C, Bonifacio E, Mezzasoma F, Cecchini D, et al. CD34+ cells from AML with mutated NPM1 harbor cytoplasmic mutated nucleophosmin and generate leukemia in immunocompromised mice. Blood. 2010;116:3907–22.
Acknowledgements
We thank all members of the AML-BFM laboratory (Essen, Germany) and study group for providing and collecting patient samples. We acknowledge support by the Open Access Publication Fund of the University of Duisburg-Essen. SS was supported by the Clinician Scientist Program of the University Medicine Essen (UMEA), which is funded by the Deutsche Forschungsgemeinschaft (DFG).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
DR, SS, and NvN designed the study. SS, AA, LMH, EA, SD, NN, DR, NvN, and MaS collected and analysed patient related data. SS, NvN, MarkusS, and DR interpreted the data; SS, EO and MichaelS performed statistical analyses and data visualisation; SS, NvN, MarkusS and DR wrote and revised the paper; all authors revised and approved the published paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sendker, S., Awada, A., Domagalla, S. et al. RUNX1 mutation has no prognostic significance in paediatric AML: a retrospective study of the AML-BFM study group. Leukemia 37, 1435–1443 (2023). https://doi.org/10.1038/s41375-023-01919-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-023-01919-8