Abstract
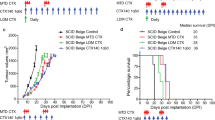
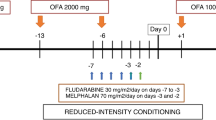
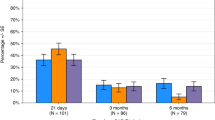
Immune evasion, due to abnormal expression of programmed-death ligands 1 and 2 (PD-L1/PD-L2), predicts poor outcomes with chemoimmunotherapy in diffuse large B-cell lymphoma (DLBCL). Immune checkpoint inhibition (ICI) has limited efficacy at relapse but may sensitise relapsed lymphoma to subsequent chemotherapy. ICI delivery to immunologically intact patients may thus be the optimal use of this therapy. In the phase II AvR-CHOP study, 28 patients with treatment-naive stage II–IV DLBCL received sequential avelumab and rituximab priming (“AvRp;” avelumab 10 mg/kg and rituximab 375 mg/m2 2-weekly for 2 cycles), R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone for 6 cycles) and avelumab consolidation (10 mg/kg 2-weekly for 6 cycles). Grade 3/4 immune-related adverse events occurred in 11%, meeting the primary endpoint of a grade ≥3 irAE rate of <30%. R-CHOP delivery was not compromised but one patient ceased avelumab. Overall response rates (ORR) after AvRp and R-CHOP were 57% (18% CR) and 89% (all CR). High ORR to AvRp was observed in primary mediastinal B-cell lymphoma (67%; 4/6) and molecularly-defined EBV-positive DLBCL (100%; 3/3). Progression during AvRp was associated with chemorefractory disease. Two-year failure-free and overall survival were 82% and 89%. An immune priming strategy with AvRp, R-CHOP and avelumab consolidation shows acceptable toxicity with encouraging efficacy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Requests for non-identifiable data for valid academic reasons as judged by the trial management group will be granted, with appropriate data sharing agreement, and should be addressed to the chief investigator (EAH). The study protocol is included as a data supplement available with the online version of this article.
References
Coiffier B, Thieblemont C, Van Den Neste E, Lepeu G, Plantier I, Castaigne S, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood. 2010;116:2040–5.
Bartlett NL, Wilson WH, Jung SH, Hsi ED, Maurer MJ, Pederson LD, et al. Dose-adjusted EPOCH-R compared with R-CHOP as frontline therapy for diffuse large B-cell lymphoma: clinical outcomes of the phase III intergroup trial alliance/CALGB 50303. J Clin Oncol. 2019;37:1790–9.
Cunningham D, Hawkes EA, Jack A, Qian W, Smith P, Mouncey P, et al. Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: a phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet. 2013;381:1817–26.
Leonard JP, Kolibaba KS, Reeves JA, Tulpule A, Flinn IW, Kolevska T, et al. Randomized phase II study of R-CHOP with or without bortezomib in previously untreated patients with non-germinal center B-cell-like diffuse large B-cell lymphoma. J Clin Oncol. 2017;35:3538–46.
Younes A, Sehn LH, Johnson P, Zinzani PL, Hong X, Zhu J, et al. Randomized phase III trial of ibrutinib and rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in non-germinal center B-cell diffuse large B-cell lymphoma. J Clin Oncol. 2019;37:1285–95.
Tilly H, Morschhauser F, Sehn LH, Friedberg JW, Trněný M, Sharman JP, et al. Polatuzumab vedotin in previously untreated diffuse large B-cell lymphoma. N. Engl Med. 2021;386:351–63.
Vitolo U, Trneny M, Belada D, Burke JM, Carella AM, Chua N, et al. Obinutuzumab or rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in previously untreated diffuse large B-cell lymphoma. J Clin Oncol. 2017;35:3529–37.
Kiyasu J, Miyoshi H, Hirata A, Arakawa F, Ichikawa A, Niino D, et al. Expression of programmed cell death ligand 1 is associated with poor overall survival in patients with diffuse large B-cell lymphoma. Blood. 2015;126:2193–201.
Godfrey J, Tumuluru S, Bao R, Leukam M, Venkataraman G, Phillip J, et al. PD-L1 gene alterations identify a subset of diffuse large B-cell lymphoma harboring a T cell-inflamed phenotype. Blood. 2019;133:2279–90.
Matias A, Suvi-Katri L, Oscar B, Satu M, Judit Mészáros J, Marja-Liisa K-L, et al. Immune cell constitution in the tumor microenvironment predicts the outcome in diffuse large B-cell lymphoma. Haematologica. 2020;106:718–29.
Keane C, Vari F, Hertzberg M, Cao KAL, Green MR, Han E, et al. Ratios of T-cell immune effectors and checkpoint molecules as prognostic biomarkers in diffuse large B-cell lymphoma: a population-based study. Lancet Haematol. 2015;2:e445–55.
Li L, Sun R, Miao Y, Tran T, Adams L, Roscoe N, et al. PD-1/PD-L1 expression and interaction by automated quantitative immunofluorescent analysis show adverse prognostic impact in patients with diffuse large B-cell lymphoma having T-cell infiltration: a study from the International DLBCL Consortium Program. Mod Pathol. 2019;32:741–54.
Armand P, Rodig SJ, Melnichenko V, Thieblemont C, Bouabdallah K, Tumyan G, et al. Pembrolizumab in patients with relapsed or refractory primary mediastinal large B-cell lymphoma (PMBCL): data from the Keynote-013 and Keynote-170 studies. Blood. 2018;132:228.
Nayak L, Iwamoto FM, LaCasce A, Mukundan S, Roemer MGM, Chapuy B, et al. PD-1 blockade with nivolumab in relapsed/refractory primary central nervous system and testicular lymphoma. Blood. 2017;129:3071–3.
Ansell SM, Minnema MC, Johnson P, Timmerman JM, Armand P, Shipp MA, et al. Nivolumab for relapsed/refractory diffuse large B-cell lymphoma in patients ineligible for or having failed autologous transplantation: a single-arm, phase II study. J Clin Oncol. 2019;37:481–9.
Forde PM, Chaft JE, Smith KN, Anagnostou V, Cottrell TR, Hellmann MD, et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N. Engl J Med. 2018;378:1976–86.
Chalabi M, Fanchi LF, Dijkstra KK, Van den Berg JG, Aalbers AG, Sikorska K, et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med. 2020;26:566–76.
Smith SD, Till BG, Shadman MS, Lynch RC, Cowan AJ, Wu QV, et al. Pembrolizumab with R-CHOP in previously untreated diffuse large B-cell lymphoma: potential for biomarker driven therapy. Br J Haematol. 2020;189:1119–26.
Nowakowski GS, Willenbacher W, Greil R, Larsen TS, Patel K, Jäger U, et al. Safety and efficacy of durvalumab with R-CHOP or R(2)-CHOP in untreated, high-risk DLBCL: a phase 2, open-label trial. Int J Hematol. 2021;115:222–32.
Younes A, Burke JM, Cheson BD, Diefenbach C, Ferrari S, Hahn UH, et al. Safety and efficacy of atezolizumab in combination with rituximab plus CHOP in previously untreated patients with diffuse large B-cell lymphoma (DLBCL): updated analysis of a phase I/II study. Blood. 2019;134:2874–74.
Bröckelmann PJ, Goergen H, Keller U, Meissner J, Ordemann R, Halbsguth TV, et al. Efficacy of nivolumab and AVD in early-stage unfavorable classic Hodgkin lymphoma: the randomized phase 2 German Hodgkin Study Group NIVAHL Trial. JAMA Oncol. 2020;6:872–80.
Hughes E, Scurr M, Campbell E, Jones E, Godkin A, Gallimore A. T-cell modulation by cyclophosphamide for tumour therapy. Immunology. 2018;154:62–8.
Lossos C, Liu Y, Kolb KE, Christie AL, Van Scoyk A, Prakadan SM, et al. Mechanisms of lymphoma clearance induced by high-dose alkylating agents. Cancer Disco. 2019;9:944–61.
Rios-Doria J, Durham N, Wetzel L, Rothstein R, Chesebrough J, Holoweckyj N, et al. Doxil synergizes with cancer immunotherapies to enhance antitumor responses in syngeneic mouse models. Neoplasia. 2015;17:661–70.
Smith MR. Rituximab (monoclonal anti-CD20 antibody): mechanisms of action and resistance. Oncogene. 2003;22:7359–68.
Casadei B, Argnani L, Morigi A, Lolli G, Broccoli A, Pellegrini C, et al. Potential survival benefit for patients receiving autologous hematopoietic stem cell transplantation after checkpoint inhibitors for relapsed/refractory Hodgkin lymphoma: a real-life experience. Hematol Oncol. 2020;38:737–41.
Rossi C, Gilhodes J, Maerevoet M, Herbaux C, Morschhauser F, Brice P, et al. Efficacy of chemotherapy or chemo-anti-PD-1 combination after failed anti-PD-1 therapy for relapsed and refractory hodgkin lymphoma: a series from lysa centers. Am J Hematol. 2018;93:1042–9.
Carreau NA, Armand P, Merryman RW, Advani RH, Spinner MA, Herrera AF, et al. Checkpoint blockade treatment sensitises relapsed/refractory non-Hodgkin lymphoma to subsequent therapy. Br J Haematol. 2020;191:44–51.
Calabretta E, Guidetti A, Ricci F, Di Trani M, Monfrini C, Magagnoli M, et al. Chemotherapy after PD-1 inhibitors in relapsed/refractory Hodgkin lymphoma: Outcomes and clonal evolution dynamics. Br J Haematol. 2022;198:82–92.
Boyerinas B, Jochems C, Fantini M, Heery CR, Gulley JL, Tsang KY, et al. Antibody-dependent cellular cytotoxicity activity of a novel anti-PD-L1 antibody avelumab (MSB0010718C) on human tumor cells. Cancer Immunol Res. 2015;3:1148–57.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. (eds). WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. International Agency for Research on Cancer, Lyon, 2017.
Scott DW, Wright GW, Williams PM, Lih CJ, Walsh W, Jaffe ES, et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood. 2014;123:1214–7.
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–82.
Keane C, Tobin J, Gunawardana J, Francis S, Gifford G, Gabrielli S, et al. The tumour microenvironment is immuno-tolerogenic and a principal determinant of patient outcome in EBV-positive diffuse large B-cell lymphoma. Eur J Haematol. 2019;103:200–7.
Kelly K, Patel MR, Infante JR, Iannotti N, Nikolinakos P, Leach J, et al. Avelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with metastatic or locally advanced solid tumors: assessment of safety and tolerability in a phase I, open-label expansion study. J Clin Oncol. 2015;33:3044–44.
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32:3059–68.
Wight J, Wai SH, Shen E, Lee S-T, Berlangieri S, Fancourt T, et al. Predicting primary treatment failure using interim FDG-PET scanning in diffuse large B-cell lymphoma. Eur J Haematol. 2021;107:475–83.
Ryland GL, Jones K, Chin M, Markham J, Aydogan E, Kankanige Y, et al. Novel genomic findings in multiple myeloma identified through routine diagnostic sequencing. J Clin Pathol. 2018;71:895–9.
Cesano A. nCounter® PanCancer Immune Profiling Panel (NanoString Technologies, Inc., Seattle, WA). J Immunother Cancer. 2015;3:42.
Dufva O, Pölönen P, Brück O, Keränen MAI, Klievink J, Mehtonen J, et al. Immunogenomic landscape of hematological malignancies. Cancer Cell. 2020;38:380–.e313.
Cheson BD, Ansell S, Schwartz L, Gordon LI, Advani R, Jacene HA, et al. Refinement of the Lugano Classification lymphoma response criteria in the era of immunomodulatory therapy. Blood. 2016;128:2489–96.
Maurer MJ, Ghesquières H, Link BK, Jais J-P, Habermann TM, Thompson CA, et al. Diagnosis-to-treatment interval is an important clinical factor in newly diagnosed diffuse large B-cell lymphoma and has implication for bias in clinical trials. J Clin Oncol. 2018;36:1603–10.
Coiffier B, Haioun C, Ketterer N, Engert A, Tilly H, Ma D, et al. Rituximab (anti-CD20 monoclonal antibody) for the treatment of patients with relapsing or refractory aggressive lymphoma: a multicenter phase II study. Blood. 1998;92:1927–32.
Younes A, Hilden P, Coiffier B, Hagenbeek A, Salles G, Wilson W, et al. International Working Group consensus response evaluation criteria in lymphoma (RECIL 2017). Ann Oncol. 2017;28:1436–47.
Allen P, Chen QC, Lu X, O’Shea K, Chmiel J, Sukhanova M, et al. Frontline treatment with single agent pembrolizumab (PEM) followed by AVD chemotherapy for classic Hodgkin lymphoma: updated results and correlative analysis. Blood. 2021;138:231–31.
Acknowledgements
This work was financially supported by Merck Healthcare Pty. Ltd., Macquarie Park, Australia, an affiliate of Merck KGaA, Darmstadt, Germany (CrossRef Funder ID: 10.13039/100009945), as part of an alliance between the healthcare business of Merck KGaA, Darmstadt, Germany, and Pfizer. Funding for biomarker analysis provided by Scott Canning Tour de Cure grant (EAH) and the Wilson Centre for Lymphoma Genomics. Dr Catherine Oakman, Western Health, provided intellectual input and logistical support. KM is a DMedSci candidate at the University of Melbourne. This work is submitted in partial fulfillment of the requirement for the DMedSci and is supported by a Research Training Program Scholarship.
Author information
Authors and Affiliations
Contributions
Contributions: EAH, GC, LC, CK, PB, CF, AS, STL designed the study; EAH, KM, GC, STL, JM, WR, JH, AB, JW, AG conducted the study; EAH, KM, GC, JM, WR, JH, AB, JW, AG recruited and followed-up with patients; EAH, KM, GC, JM, WR, JH, AB, JW, AG, CS, WL were responsible for data collection; EAH, KM, CK, STL, CS, LC, PB, MB, NN, TF, AS were responsible for data analysis; EAH, KM, GC, CK, PB, NN were involved in the interpretation of data. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
KM has received travel expenses from Bristol Myers Squibb. GC has acted as a consultant/advisor for Bristol Myers Squibb Foundation (paid to institution) and received research funding from AstraZeneca, Bayer, Bristol-Myers Squibb, Hutchison MediPharma, Isofol Medical, Merck Serono, Pharmacyclics, Regeneron, SERVIER (all paid to institution). CK has received honoraria from Roche, Beigene, Karyopharm Therapeutics. WR has received research funding from GSK, Janssen, MorphoSys and Incyte (all paid to institution). AS has acted as a consultant for Imagion; received research funding from Telix, Curis, ITM, Adalta, Fusion, Astra Zeneca, EMD Serono, Cyclotek, AVID/Lilly and Merck (all paid to institution); and holds patents relating to antibodies to EGFR, HER2, PDGF-CC, FN-14, GM-CSF and EPhA3. AB has acted as a speaker for Roche and as a consultant/advisor for Gilead. JW has received honoraria and travel subsidies from Abbvie and Janssen; and is on the advisory board for Abbive and Alexion. CF has received honoraria from Abbvie, Amgen, Bristol-Myers Squibb, Novartis and Pfizer; has acted as a consultant/advisor for Abbvie, Amgen, Astellas Pharma, Bristol-Myers Squibb, Novartis and Pfizer; and has received research funding from Amgen and Astellas Pharma. EAH has received research funding Bristol Myers Squibb/Celgene, Merck KgA, Astra Zeneca, and F. Hoffmann-La Roche (all paid to institution); has acted as a consultant/advisor for F. Hoffmann-La Roche, Antigene, Bristol Myers Squibb, Astra Zeneca, Novartis, Merck Sharpe Dohme, Specialised therapeutics and Gilead; has acted as a speaker for Roche, Astra Zeneca, Janssen, and Regeneron. The remaining authors declare no competing financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Manos, K., Chong, G., Keane, C. et al. Immune priming with avelumab and rituximab prior to R-CHOP in diffuse large B-cell lymphoma: the phase II AvR-CHOP study. Leukemia 37, 1092–1102 (2023). https://doi.org/10.1038/s41375-023-01863-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-023-01863-7