Abstract
Several studies have reported that chronic myeloid leukaemia (CML) patients expressing e14a2 BCR::ABL1 have a faster molecular response to therapy compared to patients expressing e13a2. To explore the reason for this difference we undertook a detailed technical comparison of the commonly used Europe Against Cancer (EAC) BCR::ABL1 reverse transcriptase quantitative polymerase chain reaction (RT-qPCR) assay in European Treatment and Outcome Study (EUTOS) reference laboratories (n = 10). We found the amplification ratio of the e13a2 amplicon was 38% greater than e14a2 (p = 0.015), and the amplification efficiency was 2% greater (P = 0.17). This subtle difference led to measurable transcript-type dependent variation in estimates of residual disease which could be corrected by (i) taking the qPCR amplification efficiency into account, (ii) using alternative RT-qPCR approaches or (iii) droplet digital PCR (ddPCR), a technique which is relatively insensitive to differences in amplification kinetics. In CML patients, higher levels of BCR::ABL1/GUSB were identified at diagnosis for patients expressing e13a2 (n = 67) compared to e14a2 (n = 78) when analysed by RT-qPCR (P = 0.0005) but not ddPCR (P = 0.5). These data indicate that widely used RT-qPCR assays result in subtly different estimates of disease depending on BCR::ABL1 transcript type; these differences are small but may need to be considered for optimal patient management.
Similar content being viewed by others
Introduction
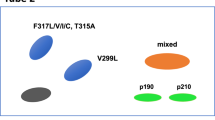
BCR::ABL1 is the primary driver of chronic myeloid leukaemia (CML) but this chimeric gene exists in several different isoforms that need to be recognized for optimal patient management [1]. The two most common BCR::ABL1 mRNA transcripts, both of which encode a 210 kDa BCR::ABL1 protein (p210), are characterized by splicing of BCR exon 13 or BCR exon 14 to ABL1 exon 2, and are designated as e13a2 and e14a2, respectively [1,2,3]. BCR exon 14 is 75 bp in size and thus the e14a2 mRNA encodes an additional 25 amino acids compared to e13a2 [1]. Together, these two transcripts are seen in 98% of cases of CML, with e14a2 nearly twice as prevalent as e13a2 and up to 10% of cases expressing both variants [2]. The remaining 2% of CML cases express atypical BCR::ABL1 fusions involving different BCR and/or ABL1 exons; recognition of these cases is important for their clinical management [4]. The BCR::ABL1 transcript type expressed by individual patients is determined largely by the precise positions of the genomic breakpoints on chromosomes 22 and 9 [5], and is thus stable over time.
For routine molecular monitoring of response to treatment, most laboratories use the Europe Against Cancer (EAC) reverse transcriptase quantitative polymerase chain reaction (RT-qPCR) assay, or variants thereof, which use a single primer pair/probe combination to detect and quantify e13a2 and/or e14a2 in the same procedure [6]. Whilst this allows for a single test to be used for the vast majority of CML patients, it presents a potential technical issue as the e14a2 amplicon is approximately twice as large as e13a2 (149 bp vs 74 bp; Fig. 1), and it is known that the qPCR quantification cycle (Cq) generally increases as a function of amplicon size [7]. Indeed, a small study has described a bias towards preferential amplification of e13a2 over e14a2 when using RT-qPCR compared to digital droplet PCR (ddPCR), as well as distinct RT-qPCR amplification profiles for each transcript type [8].
Several clinical studies have indicated that patients expressing e13a2 BCR::ABL1 have an inferior molecular response to treatment at multiple timepoints compared to those expressing e14a2 [9,10,11], although this does not appear to translate into a measurable effect on survival [12]. The possibility that the observed difference in response could be explained by variance in RT-qPCR assay performance between the two major transcripts has not yet been fully investigated. As treatment cessation for CML patients who achieve sustained deep molecular response (DMR) to tyrosine kinase inhibitor (TKI) therapy becomes routine practice, it is increasingly important to ensure molecular monitoring is as accurate as possible for all patients, and that treatment decisions are based upon robust laboratory data.
The study described here was designed to investigate the possibility that the observation of higher measurable residual disease (MRD) levels in e13a2 patients could be due to differing efficiencies in PCR amplification between the two transcripts, which is a crucial parameter in RT-qPCR [13, 14].
Methods
EUTOS technical study
RT-qPCR study design
14 reference laboratories from the European Treatment and Outcome Study (EUTOS) for CML network that routinely use the EAC BCR::ABL1 assay (Fig. 1) and ABL1 as a reference gene were sent study materials that were prepared in Salisbury. The materials included (i) three sets of primers and probes: set 1 was specific to e13a2 [15], set 2 used the EAC design for BCR::ABL1 [6] and set 3 was specific to e14a2 (Supplementary Table 1); [15] (ii) 1 set of plasmid dilutions and 3 sets of cell lysate dilutions for both e13a2 and e14a2. RNA extraction, cDNA synthesis and EAC BCR::ABL1 qPCR were performed at each site according to local procedures and included the use of laboratory-specific conversion factors (CF) to express results on the International Scale (IS) according to the protocol detailed in Supplementary Methods A and summarised in Supplementary Fig. 1. Results were assessed to ensure the study protocol had been complied with and were excluded from 3 laboratories due to the use of variable RT-qPCR thresholds across different runs. The results from one further laboratory were also excluded as the average AR of the local BCR::ABL1 assay exceeded 1.5 fold of the interquartile range of all laboratories [16]. The final dataset thus consisted of results from 10 laboratories. Since both the ERM-AD623 certified reference plasmid [17] and WHO International Genetic Reference Panel for the quantitation of BCR::ABL1 [18] are both based on e14a2 BCR::ABL1, results were considered relative to this transcript type.
e14a2 and e13a2 plasmids
The ERM-AD623 certified reference plasmid includes the e14a2 BCR::ABL1 junction sequence as well as parts of the ABL1, BCR and GUSB genes that are used commonly as a reference to control for variation in sample quality and RT-qPCR efficiency. The plasmid is supplied as 6 different concentrations over a range of 10 to 1 × 106 copies/µL and is commonly used as a calibration standard by laboratories performing molecular monitoring for CML [17]. The e13a2 plasmid was identical in construction to ERM-AD623 but contains an e13a2 BCR::ABL1 fragment in place of e14a2 (Supplementary Fig. 2). A 10-fold dilution series from approximately 10 to 1 × 106 copies/µL was prepared and calibrated to ERM-AD623 reference material using ABL1 copy number data (Supplementary Fig. 3). Each plasmid has a 1:1 ratio of BCR::ABL1/ABL1 copy numbers. Laboratories using the EAC assay routinely use an e14a2 plasmid to generate standard curves and use this curve to assign copy numbers to patient samples regardless of the transcript type being expressed, resulting in potential discrepancies in amplicon size between the standard curve and sample.
Cell line material
A five-fold dilution series was prepared by diluting BCR::ABL1 human cell lines expressing e14a2 (K562) or e13a2 (KCL-22) into a BCR::ABL1 negative cellular background (HL60). Dilutions of each cell line were targeted to contain approximately 10, 2, 0.4, 0.08, or 0.016% BCR::ABL1/ABL1, which was confirmed by RT-qPCR prior to distribution. The initial dilution was generated by adding 6 × 105 BCR::ABL1 expressing cells (K562 or KCL-22) to 6 × 107 HL60 cells, which were then further serially diluted into HL60 cells at a concentration of 1.5 × 106 cells/ml. Cells were lysed in RLT buffer (Qiagen, Hilden, Germany) according to the manufacturer’s instructions to generate final cell lysates samples containing approximately 5 × 105 cells in 600 µL of lysis buffer.
Droplet digital PCR
ddPCR was performed using EAC-based BCR::ABL1 and ABL1 assays according to locally established procedures [19], or with the commercially available QXDx BCR::ABL1 %IS kit (BioRad, Hercules, California, USA), according to the manufacturer’s instructions. Both cell line and plasmid material were tested, however as ddPCR experiments can become saturated at very high levels of template copy number, only 4/6 plasmid dilutions were used for ddPCR experiments, spanning a concentration range of approximately 1 × 101 to 1 × 104 copies/µL. The ratio of BCR::ABL1/ABL1 was calculated from the reported copy number of each target.
Dynamics of RT-qPCR
We measured two parameters to assess the performance of e13a2 and e14a2 amplification: (i) the amplification ratio (AR) and (ii) amplification efficiency (E) as previously defined [20]. Amplification efficiency-corrected AR values (designated ARC) were calculated [21], as well as the expected number of copies of a target amplicon with the observed values of E for e13a2 and e14a2. These calculations are detailed in Supplementary Methods B.
Patient cohorts
Diagnostic CML cohort
A cohort of CML patients at diagnosis were identified (n = 152). Patients shown to be co-expressing both e13a2 and e14a2 were excluded (n = 7), leaving a total of 145 cases in the final analysis (e13a2, n = 67; e14a2, n = 78). Patient samples were analysed using RT-qPCR assays for BCR::ABL1 and GUSB [6]. The same samples were also analysed using an in-house RT-ddPCR for BCR::ABL1 [19]. The BCR::ABL1 assays used for RT-qPCR and ddPCR both co-amplified e13a2 and e14a2. Results were expressed as %BCR::ABL1 (RT-qPCR or ddPCR copies) / GUSB (RT-qPCR copies). Results were not converted to the International Scale as the %BCR::ABL1 / GUSB values greatly exceeded 10%.
Subset of patients with sequential monitoring data
Sequential prospective monitoring of MRD at both the mRNA and DNA levels for a subset of 81 CML patients (43 males, 38 females) has been described previously [19]. Finally, data from 67/81 patients with optimized DNA-based assays were used and evaluated (Supplementary methods C). Of these, 27 patients expressed e13a2 and 40 patients expressed e14a2 BCR::ABL1 transcript type. Monitoring data from these patients were used to determine the time to achieve of a 3-log reduction in disease levels using a measure of individual molecular response (IMR) that is applicable to both RNA and DNA samples, as well as the kinetics of disease reduction [22] as described in detail in Supplementary Methods C.
Statistical analysis
Comparisons between groups were performed using the Mann-Whitney U test. Paired comparisons were performed using the Wilcoxon signed-rank test, with Bonferroni correction for multiple tests where appropriate. RT-qPCR and ddPCR measurements were also compared using Bland-Altman analysis [23] with the blandr package for R [24] to assess bias.
Results
Impact of BCR::ABL1 transcript type on amplification performance
To investigate the kinetics of BCR::ABL1 amplification by RT-qPCR by the widely-used EAC protocol, we undertook a detailed multicentre performance evaluation using control materials according to the schema shown in Supplementary Fig. 1. As the plasmid BCR::ABL1/ABL1 copy number ratio is 1:1 regardless of plasmid concentration, the median laboratory specific amplification ratio (number of target molecules relative to the number reference molecules; AR, see Supplementary Methods B) for each transcript type was determined using all plasmid samples for the routine, EAC-based BCR::ABL1 assay for each laboratory (runs 5 and 6, Supplementary Fig. 1). The e13a2 AR values were higher than e14a2 in 8/10 laboratories and, overall, the laboratory specific AR values were 38% higher for e13a2 compared to e14a2 (n = 10, median e13a2 AR = 1.57 versus e14a2 AR = 1.14, P = 0.015, Table 1, Fig. 2A). To determine if the observed difference in AR could be explained by differences in amplification efficiency, we estimated E (Supplementary Methods B, eqn. 2) for the e13a2, e14a2 and ABL1 assays for each centre using the results from plasmid samples (runs 5 and 6). Overall, amplification of e13a2 was 2% more efficient than e14a2, although this difference did not reach statistical significance (e13a2 median E = 0.972 versus e14a2 = 0.953, P = 0.17, Supplementary Fig. 4A). The amplification efficiency-corrected ARC values showed a reduction in the difference between e13a2 and e14a2; the median e13a2 ARC remained slightly greater than e14a2, but the difference was no longer significant (median e13a2 ARC = 1.18 versus e14a2 = 0.99, P = 0.63 Fig. 2B). This correction suggests the differences in amplification efficiency explain at least some of the observed difference in AR between e13a2 and e14a2.
A Without correction for efficiency, the median AR of the shorter EAC e13a2 amplicon was significantly higher than e14a2 (n = 10, median e13a2 ratio = 1.57, e14a2 ratio = 1.14, P = 0.015; Mann—Whitney U test). B Correcting for amplification efficiency greatly reduces this discrepancy (median e13a2 corrected ratio = 1.18, e14a2 = 0.99, P = 0.63). Using transcript-specific assays that are more similar in size, with (C) no efficiency correction the shorter e14a2 amplicon has a slightly elevated median AR compared to e13a2, but the difference is not statistically significant (median e13a2 ratio 1.34, e14a2 = 1.61, P = 0.31). D After correction for efficiency the difference is reduced (median e13a2 corrected ratio = 1.18, e14a2 = 1.23, P = 0.68).
To understand in more detail the impact of different amplicon size, the study design included e13a2-specific and e14a2-specific qPCR assays that are used routinely by some centres, particularly in Australasia [15]. The amplicon length for these assays is more comparable between BCR::ABL1 isoforms; e13a2 (96 bp) and e14a2 (74 bp). In contrast to the EAC assay, we found the AR for the specific assays to be higher for e14a2 in 7/10 laboratories, but the difference overall was not statistically significant (median AR for e13a2 = 1.34 versus e14a2 = 1.61, P = 0.31, Fig. 2C, Table 1). Furthermore, we found that the shorter e14a2 amplicon amplified 2% more efficiently than e13a2 using the transcript-specific assays (median E for e13a2 = 0.962 versus e14a2 = 0.982, P = 0.069, Supplementary Fig. 4B). Correction for amplification efficiency resulted in a median ARC that was closer to 1 for both transcripts, as well as a reduced difference in AR although the e14a2 ratio remained slightly greater than e13a2 (median e13a2 ARC = 1.18 versus e14a2 ARC = 1.23, p = 0.68, Fig. 2D, Table 1). Interestingly, these results are the inverse of those obtained from the EAC qPCR assay, with the e14a2 specific primers outperforming those specific to e13a2. In both cases, however, the more efficient amplification was seen for the shorter amplicon (Table 1).
Impact of BCR::ABL1 transcript type on standard curves used for quantification of copy number
To investigate if the BCR::ABL1/ABL1 qPCR results could be influenced by the transcript type of the standard curve, BCR::ABL1/ABL1 values for KCL-22 (e13a2 cell line) dilutions were calculated using the local EAC qPCR assay and either the e13a2 or the ERM-AD623 e14a2 plasmid standard curves used to assign copy numbers (runs 5 and 6). If the performance of the assay was similar for both transcript types, then the transcript type of the standard curve should not affect the calculated BCR::ABL1/ABL1 values. For all dilutions, the results (log10 scale) were higher when calculated using the e14a2 standard curve, compared to using the e13a2 standard curve (Fig. 3). This difference was statistically significant at the 0.016%, 0.08%, 0.4 and 2% dilution points and approached significance at the 10% dilution. After applying laboratory-specific CFs (derived from previous EUTOS standardisation rounds) to the results, there was no significant difference between BCR::ABL1/ABL1 derived from the e13a2 standard curve, and BCR::ABL1IS, indicating that the use of a CF may go some way to mitigating the difference in efficiency (Fig. 3).
Log10 BCR::ABL1/ABL1 percentages derived from serially diluted e13a2 BCR::ABL1 cell line (KCL-22) lysates, calculated using either an e13a2 (red) or e14a2 (green) standard curve, or with the e14a2 standard curve and results converted to the IS (blue). e13a2 BCR::ABL1 results were consistently higher when calculated with an e14a2 standard curve compared to using an e13a2 standard curve (0.016% dilution, P = 0.012; 0.08% dilution, P = 0.041; 0.4% dilution, P = 0.041; 2% dilution, P = 0.041; 10% dilution, P = 0.058; Wilcoxon signed-rank test with Bonferroni correction for multiple comparisons). Using results expressed on the IS resolved this difference but with an apparent increase in variability.
However, estimation of e13a2 using the e14a2 standard curve with or without the CF resulted in increased variability compared to using the e13a2 standard curve (Fig. 3). The mean coefficient of variation (CV) across all dilutions of the e13a2 cell line when using the e13a2 standard curve was 33%, compared to 41% when using the e14a2 standard curve and CF. In contrast, the mean CV of the BCR::ABL1/ABL1 results from the e14a2 cell line decreased from 43 to 32% when laboratory-specific CFs were applied. This suggests that CFs are not completely optimised for e13a2 BCR::ABL1, and interestingly, that e13a2 amplification may be inherently less variable than e14a2, possibly as a result of the much shorter amplicon.
Effect of using ddPCR
To investigate if the differences in performance were specific to RT-qPCR, two laboratories performed ddPCR using their in-house ddPCR protocols, as well as a commercially available, CE marked ddPCR kit (QXDx BCR-ABL %IS, BioRad) for monitoring of BCR::ABL1 on the IS. Using the EAC primers and plasmid dilutions, there was no difference in ddPCR AR at either laboratory (Salisbury P = 0.89; Prague P = 0.71, Supplementary Fig. 5). The QXDx assay is not compatible with the ABL1 moiety in the ERM-AD623 plasmid and thus we were unable to perform the same comparison using the commercial kit, but we were able to compare BCR::ABL1IS RT-qPCR and QXDx IS ddPCR results for the cell line dilutions (n = 40). Bland-Altman analysis of the difference between the average log10 ddPCR and RT-qPCR results for both transcript types combined showed a bias of −0.11 (SD = 0.22, 95% CI [−0.15,−0.06]), (Supplementary Fig. 6). Individual analysis of each transcript type (Fig. 4) showed a negligible bias of −0.001 for e13a2 however the bias observed for e14a2 was −0.218, suggesting that the EAC RT-qPCR assay does not amplify e14a2 as effectively as the e13a2 transcript when compared to ddPCR. Although we did not observe a difference in AR using EAC ddPCR assays, ddPCR is able to distinguish between the two transcript types, with distinct clusters of droplets defined by BCR::ABL1 fluorescent amplitude present for each transcript, as has been reported previously [8].
Good concordance for the e13a2 amplicon (mean bias = −0.001, SD = 0.18, 95% CI [0.05, −0.05]) but negative bias for the e14a2 amplicon (mean bias = −0.218, SD = 0.21, 95% CI [−0.28, −0.16]). Each point represents the mean BCR::ABL1IS result of a cell lysate sample from a single laboratory, and the results cluster around the mean results from each dilution point. Blue shading indicates the mean bias (dashed line) and corresponding 95% CI (dotted lines). Green shading indicates the upper LoA and corresponding 95% CI. Red shading indicates the lower LoA and the corresponding 95% CI. SD = standard deviation, CI = confidence interval, LoA = 95% limit of agreement. Log10 scale.
Impact of transcript type in a patient cohort
To assess our findings in CML patients (n = 145), we used both RT-qPCR and ddPCR to measure %BCR::ABL1/GUSB at diagnosis. Using RT-qPCR, the %BCR::ABL1/GUSB was significantly higher for patients expressing e13a2 compared with those expressing e14a2 (e13a2 = 48.3%, e14a2 = 37.7%, P = 0.0005, Fig. 5A). Furthermore, the fold difference in median levels for each transcript type was 1.28, close to the theoretical 1.35-fold difference (equation 4 with 30 PCR cycles; Supplementary Methods) that would be expected given the observed 2% difference in amplification efficiency between targets. However, when BCR::ABL1 was analysed using ddPCR, the difference in %BCR::ABL1/GUSB was no longer significant (e13a2 = 37.2%, e14a2 = 34.6%, P = 0.5, Fig. 5B). Comparison of %BCR::ABL1/GUSB results for each transcript type considered independently showed that the results obtained by RT-qPCR for e13a2 remained significantly greater than those obtained by ddPCR, whereas there was no significant difference for e14a2 (e13a2, P < 0.0001; e14a2, P = 0.22; Fig. 6). Bland-Altman analysis of RT-qPCR and ddPCR results showed a mean bias for e13a2 of 11.52% (95% CI [6.84, 16.21], Fig. 7A), compared to a mean bias for e14a2 of 0.85% (95% CI [−2.94, 4.638], Fig. 7B). Taken together, these data confirm that e13a2 BCR::ABL1 is overestimated relative to e14a2 in the RT-qPCR assay at diagnosis, thereby resulting in artificially elevated BCR::ABL1 results for patients expressing this isoform.
A Using RT-qPCR, the %BCR::ABL1/GUSB results were significantly higher in patients expressing e13a2 compared to those expressing e14a2 (median %BCR::ABL1/GUSB; e13a2 = 48.3%, e14a2 = 37.7%, p = 0.0005). B ddPCR measurements for BCR::ABL1 in the same samples showed no significant difference between transcripts (median %BCR::ABL1/GUSB for e13a2 = 37.2% versus e14a2 = 34.6%, P = 0.5). Mann—Whitney U test.
A For the e13a2 patient group, RT-qPCR for BCR::ABL1 gave significantly higher %BCR::ABL1/GUSB results compared to ddPCR for BCR::ABL1 (e13a2 median ddPCR = 37.16% versus RT-qPCR = 48.32%, P < 0.0001, n = 67). B In the e14a2 group, there was no significant difference in %BCR::ABL1/GUSB between methods (median ddPCR = 34.64% versus RT-qPCR = 37.69%, P = 0.22, n = 78). Wilcoxon signed-rank test.
A For e13a2 samples (n = 67) the mean bias was 11.52% (95% CI [6.84, 16.21], SD = 19.20). B For e14a2 samples (n = 78) we found a negligible mean bias of 0.85% (95% CI [–2.94, 4.64], SD = 16.80). Blue shading indicates the mean bias (dashed line) and corresponding 95% CI (dotted lines). Green shading indicates the upper LoA and corresponding 95% CI. Red shading indicates the lower LoA and the corresponding 95%CI. CI confidence Interval, SD standard deviation, LoA 95% limits of agreement.
We investigated the effect of BCR::ABL1 transcript type in a cohort of patients undergoing TKI treatment (n = 67). Concordant with the findings of other groups, the time to MMR was shorter for patients expressing e14a2 compared to e13a2, although the difference was not significant in our relatively small series of cases (P = 0.077; Supplementary Fig. 7). The analysis of cumulative achievement of a 3 log reduction of BCR::ABL1 based on IMR measurements (i.e. relative to pretreatment levels for each patient) for both mRNA and DNA assessments showed noticeably less difference between transcript types (Supplementary Fig. 8). Examination of the kinetics of decline using a bi-exponential mixed effect model showed no difference in the α and β slopes between e13a2 and e14a2 for either mRNA or DNA-based assessments (Supplementary Fig. 8).
Discussion
Molecular monitoring to assess time-dependent therapeutic milestones is an important element in the management of patients with CML [25]. In recent years, several studies have reported that patients expressing e13a2 BCR::ABL1 have an inferior molecular response at multiple timepoints compared to those expressing e14a2 [9,10,11]. Although this difference does not affect overall survival [12], it would be expected to have some impact on the achievement of specific milestones as well as eligibility for, or timing of, treatment cessation. Broadly there are two potential, and not necessarily mutually exclusive, explanations for these findings: (i) there is a biological difference between e13a2 and e14a2 BCR::ABL1 that influences response to treatment [26] or (ii) the difference is a technical artefact attributable to the kinetics of RT-qPCR assays employed to measure BCR::ABL1 mRNA levels. There is some support for the notion that there may be a genuine biological difference between BCR::ABL1 isoforms, for example the finding that transcript type is associated with white cell or platelet counts at presentation [10, 11], progression-free survival [9] or cytogenetic response [27]. However these associations have not been replicated in multiple studies and thus remain tentative. Our study provides evidence that at least part of the difference is technical, and dependent on the assay configuration.
With RT-qPCR, BCR::ABL1 and reference gene copy numbers are estimated by interpolation of sample Cq to a standard curve derived from calibrated control reagents, and BCR::ABL1 copies are reported as a percentage of the reference gene, commonly ABL1, BCR or GUSB [28]. A difference in the efficiency of the target and/or reference gene amplification has the potential to introduce error into the results [29], which is why great care should be taken to ensure amplification is as efficient as possible, and equal for all targets tested [14]. Our results show that the EAC assay performs sub optimally in most laboratories when the target is e14a2, as compared to e13a2. In terms of E, the difference appears slight, but there was a significant difference in AR between e13a3 and e14a2 (Fig. 2A). We were able to correct for this difference by incorporating E into the calculation, indicating that a small difference in E is sufficient to have a measurable impact on the outcome. A likely source for the discrepancy in amplification performance is the difference in amplicon length generated by the EAC assay, although the sequence itself may also be important [6, 7]. Using transcript-specific assays that generate amplicons that are more similar in length, we did not observe a significant difference in AR between the transcript types, but the AR of the shorter amplicon was elevated in comparison to the longer one, supporting the hypothesis that the larger e14a2 EAC amplicon may be impacting amplification performance. Of note, the Adelaide group (which uses transcript-specific assays) did not find any impact of transcript type on the achievement of MMR or MR4, although they did find that e14a2 patients were more likely to achieve MR4.5 at 48 months [30].
A typical BCR::ABL1 RT-qPCR test result assumes the equal performance of multiple separate amplifications (BCR::ABL1 and reference gene for the sample and a 6-point standard curve such as ERM-AD623). This may be a reasonable assumption when comparing like-for-like samples and calibrators, however the commonly used ERM-AD623 plasmid calibrator contains the e14a2 target sequence [17]. As we and others [8] have shown, there is a clear difference in how the EAC-designed BCR::ABL1 RT-qPCR assay performs depending on the transcript type. It is unsurprising, therefore, that the use of a standard curve containing a different target amplicon may skew the results of an experiment. Indeed, we observed inflated BCR::ABL1 values from e13a2 expressing cell lines when an e14a2 calibrator was used, compared to results obtained using a matched e13a2 calibrator (Fig. 3). We observed the same pattern of results when an e13a2 calibrator was used to assign BCR::ABL1 values from e14a2 expressing cell lines (data not shown), which is consistent with an e13a2 standard curve that is amplifying more effectively than the e14a2 standard curve. Although the application of laboratory-specific CFs helps to mitigate against this difference, the increase in variation of the results suggests that CFs may not be fully optimised for the e13a2 transcript. Recent work by Dominy et al [31] also investigated the effect of transcript-specific standard curves, and our results corroborate and extend their findings. All currently available reference materials for BCR::ABL1 are based on e14a2, which likely accounts for the relative lack of assay optimisation for e13a2. In theory these issues could be addressed by production of e13a2-based reference materials that would enable assay optimisation (and potentially new assay design), estimation of E and correction of results. The ‘Pfaffl method’, for example, is frequently used in relative quantitation experiments [32] and has been proposed for use in absolute quantitation [29, 33]. However development of certified reference materials is a lengthy and complex process; furthermore it is not entirely clear how to deal with patients who express both e13a2 and e14a2.
An alternative approach is to use ddPCR, a technique which is relatively insensitive to differences in amplification efficiency as well as having other advantages such as producing results that are less variable that those produced by RT-qPCR and the lack of requirement for a standard curve [34,35,36,37]. Our initial data using control materials indicated that ddPCR results do not show the transcript-related differences that were seen using RT-qPCR. This was confirmed in CML patients, for whom we found BCR::ABL1/GUSB levels at diagnosis were apparently elevated in e13a2 cases compared to e14a2 when using RT-qPCR, but no difference was seen with ddPCR. The negative bias in RT-qPCR e14a2 amplification when compared with ddPCR is consistent with reduced efficiency of the e14a2 EAC assay as the source of experimental error. It is important to note that variations in laboratory protocols, including the use of different reference genes, are likely to lead to variable levels of bias (if any) between transcript types in different laboratories, and testing centres with concerns should undertake their own internal investigations to determine the performance of their assays for both e13a2 and e14a2 BCR::ABL1.
When RT-qPCR results were normalized to pre-treatment levels, there was no difference between transcript types with respect to achievement of a 3-log reduction in levels of disease, and no difference in the α or β slopes was apparent (Supplementary Fig. 8). Although this approach is helpful to evaluate prognostically significant differences in the rate of disease reduction during the first weeks of therapy [38, 39], and is the only approach to monitor molecular response for cases with rare, atypical BCR::ABL1 variants [4], it is of limited value for most patients because the results cannot be related to the IS. Similarly, DNA-based results can provide useful information in patients in DMR [19, 40] but this technically difficult approach appears to add little value for routine monitoring.
In conclusion, there is a growing body of evidence that points to discrepancies in the performance of the EAC RT-qPCR assay in relation to BCR::ABL1 transcript type. This issue is almost certainly not limited to the EAC primer/probe set, but likely affects other assays with similar differences in amplicon sizes between e13a2 and e14a2. It is important to emphasize, however, that the discrepancy is subtle and, although its consequences are apparently detectable in some large studies [9,10,11], the effect on individual cases is expected to be very small [31]. Nevertheless, we recommend caution in making clinical decisions based on patient transcript type and stress the need to consider trends in sequential MRD results in addition to the achievement of defined milestones at specific timepoints.
Data availability
The datasets generated during the study are available from the corresponding author on reasonable request.
References
Chereda B, Melo JV. Natural course and biology of CML. Ann Hematol. 2015;94:107–21.
Baccarani M, Castagnetti F, Gugliotta G, Rosti G, Soverini S, Albeer A, et al. The proportion of different BCR-ABL1 transcript types in chronic myeloid leukemia. An international overview. Leukemia. 2019;33:1173–83.
Melo JV. The diversity of BCR-ABL fusion proteins and their relationship to leukemia phenotype. Blood 1996;88:2375–84.
Schäfer V, White HE, Gerrard G, Möbius S, Saussele S, Franke G-N, et al. Assessment of individual molecular response in chronic myeloid leukemia patients with atypical BCR-ABL1 fusion transcripts: recommendations by the EUTOS cooperative network. J cancer Res Clin Oncol. 2021;147:3081–9.
Ross D, O’Hely M, Bartley P, Dang P, Score J, Goyne J, et al. Distribution of genomic breakpoints in chronic myeloid leukemia: analysis of 308 patients. Leukemia. 2013;27:2105–7.
Gabert J, Beillard E, Velden VHJvd, Bi W, Grimwade D, Pallisgaard N, et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia – A Europe Against Cancer Program. Leukemia. 2003;17:2318–57.
Debode F, Marien A, Janssen É, Bragard C, Berben G. The influence of amplicon length on real-time PCR results. Biotechnol Agron Soc Environ. 2017;21:3–11.
Kjaer L, Skov V, Andersen MT, Aggerholm A, Clair P, Gniot M, et al. Variant-specific discrepancy when quantitating BCR-ABL1 e13a2 and e14a2 transcripts using the Europe Against Cancer qPCR assay. Eur J Haematol. 2019;103:26–34.
Castagnetti F, Gugliotta G, Breccia M, Iurlo A, Levato L, Albano F, et al. The BCR-ABL1 transcript type influences response and outcome in Philadelphia chromosome-positive chronic myeloid leukemia patients treated frontline with imatinib. Am J Hematol. 2017;92:797–805.
Hanfstein B, Lauseker M, Hehlmann R, Saussele S, Erben P, Dietz C, et al. Distinct characteristics of e13a2 versus e14a2 BCR-ABL1 driven chronic myeloid leukemia under first-line therapy with imatinib. Haematologica. 2014;99:1441–7.
Jain P, Kantarjian H, Patel KP, Gonzalez GN, Luthra R, Shamanna RK, et al. Impact of BCR-ABL transcript type on outcome in patients with chronic-phase CML treated with tyrosine kinase inhibitors. Blood. 2016;127:1269–75.
Pfirrmann M, Evtimova D, Saussele S, Castagnetti F, Cervantes F, Janssen J, et al. No influence of BCR-ABL1 transcript types e13a2 and e14a2 on long-term survival: results in 1494 patients with chronic myeloid leukemia treated with imatinib. J cancer Res Clin Oncol. 2017;143:843–50.
Bustin S, Huggett J. qPCR primer design revisited. Biomolecular Detection Quantification. 2017;14:19–28.
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M, et al. The MIQE Guidelines: Minimum Information for Publication of Quantitative Real-Time PCR Experiments. Clin Chem. 2009;55:611–22.
Branford S, Hughes TP, Rudzki Z. Monitoring chronic myeloid leukaemia therapy by real-time quantitative PCR in blood is a reliable alternative to bone marrow cytogenetics. Br J Haematol. 1999;107:587–99.
Tukey JW Exploratory data analysis. Addison-Wesley Series in Behavioral Science: Quantitative Methods. 1977.
White H, Deprez L, Corbisier P, Hall V, Lin F, Mazoua S, et al. A certified plasmid reference material for the standardisation of BCR–ABL1 mRNA quantification by real-time quantitative PCR. Leukemia. 2015;29:369–76.
White HE, Matejtschuk P, Rigsby P, Gabert J, Lin F, Lynn Wang Y, et al. Establishment of the first World Health Organization International Genetic Reference Panel for quantitation of BCR-ABL mRNA. Blood. 2010;116:e111–7.
Machova Polakova K, Zizkova H, Zuna J, Motlova E, Hovorkova L, Gottschalk A, et al. Analysis of chronic myeloid leukaemia during deep molecular response by genomic PCR: a traffic light stratification model with impact on treatment-free remission. Leukemia. 2020;34:2113–24.
Kubista M, Andrade JM, Bengtsson M, Forootan A, Jonák J, Lind K, et al. The real-time polymerase chain reaction. Mol Asp Med. 2006;27:95–125.
Sta A, Kubista M. Quantitative real-time PCR method for detection of b-lymphocyte monoclonality by comparison of κ and λ immunoglobulin light chain expression. Clin Chem. 2003;49:9.
Glauche I, Kuhn M, Baldow C, Schulze P, Rothe T, Liebscher H, et al. Quantitative prediction of long-term molecular response in TKI-treated CML – Lessons from an imatinib versus dasatinib comparison. Sci Rep. 2018;8:12330.
Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327:307–10.
Datta D blandr: a Bland-Altman Method Comparison package for R. 2017.
Hochhaus A, Baccarani M, Silver RT, Schiffer C, Apperley JF, Cervantes F, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34:966–84.
Baccarani M, Rosti G, Soverini S. Chronic myeloid leukemia: the concepts of resistance and persistence and the relationship with the BCR-ABL1 transcript type. Leukemia. 2019;33:2358–64.
Lucas CM, Harris RJ, Giannoudis A, Davies A, Knight K, Watmough SJ, et al. Chronic myeloid leukemia patients with the e13a2 BCR-ABL fusion transcript have inferior responses to imatinib compared to patients with the e14a2 transcript. Haematologica. 2009;94:1362.
Cross NC, White HE, Colomer D, Ehrencrona H, Foroni L, Gottardi E, et al. Laboratory recommendations for scoring deep molecular responses following treatment for chronic myeloid leukemia. Leukemia. 2015;29:999–1003.
Gallup JM Difficult templates and inhibitors of PCR. PCR Troubleshooting and Optimization: The Essential Guide. 2011.
Marum JE, Branford S. Current developments in molecular monitoring in chronic myeloid leukemia. Therapeutic Adv Hematol. 2016;7:237–51.
Dominy KM, Claudiani S, O'Hare M, Szydlo R, Gerrard G, Foskett P, et al. Assessment of quantitative polymerase chain reaction for BCR-ABL1 transcripts in chronic myeloid leukaemia: Are improved outcomes in patients with e14a2 transcripts an artefact of technology? Br J Haematol. 2022;197:52–62.
Pfaffl MW. A new mathematical model for relative quantification in real-time RT–PCR. Nucleic Acids Res. 2001;29:e45.
Brankatschk R, Bodenhausen N, Zeyer J, Bürgmann H. Simple absolute quantification method correcting for quantitative PCR efficiency variations for microbial community samples. Appl Environ Microbiol. 2012;78:4481–9.
Bernardi S, Malagola M, Zanaglio C, Polverelli N, Dereli Eke E, D’Adda M, et al. Digital PCR improves the quantitation of DMR and the selection of CML candidates to TKIs discontinuation. Cancer Med. 2019;8:2041–55.
Bochicchio MT, Petiti J, Berchialla P, Izzo B, Giugliano E, Ottaviani E, et al. Droplet digital PCR for BCR–ABL1 monitoring in diagnostic routine: ready to start? Cancers 2021;13:5470.
Franke G-N, Maier J, Wildenberger K, Cross M, Giles FJ, Müller MC, et al. Comparison of real-time quantitative PCR and digital droplet PCR for BCR-ABL1 monitoring in patients with chronic myeloid leukemia. J Mol Diagnostics. 2020;22:81–9.
Scott S, Cartwright A, Francis S, Whitby L, Sanzone AP, Mulder A, et al. Assessment of droplet digital polymerase chain reaction for measuring BCR-ABL1 in chronic myeloid leukaemia in an international interlaboratory study. Br J Haematol. 2021;194:53–60.
Branford S, Yeung DT, Parker WT, Roberts ND, Purins L, Braley JA, et al. Prognosis for patients with CML and >10% BCR-ABL1 after 3 months of imatinib depends on the rate of BCR-ABL1 decline. Blood. 2014;124:511–8.
Hanfstein B, Shlyakhto V, Lauseker M, Hehlmann R, Saussele S, Dietz C, et al. Velocity of early BCR-ABL transcript elimination as an optimized predictor of outcome in chronic myeloid leukemia (CML) patients in chronic phase on treatment with imatinib. Leukemia. 2014;28:1988–92.
Pagani IS, Dang P, Saunders VA, Grose R, Shanmuganathan N, Kok CH, et al. Lineage of measurable residual disease in patients with chronic myeloid leukemia in treatment-free remission. Leukemia. 2020;34:1052–61.
Acknowledgements
This study was supported by the European LeukemiaNet via the “European Treatment and Outcome Study for CML”, EUTOS. Matthew Salmon was also supported by the Salisbury District Hospital Stars Appeal. Jan Zuna received support from the Czech Health Research Council NU21-03-00128.
Author information
Authors and Affiliations
Contributions
The study was designed by MS, HW, TE, AH, KMP and NC. MS and HW prepared samples for the technical aspect of the study, distributed the samples to participating EUTOS laboratories and analysed the data. Work in the participating laboratories was performed or supervised by HZ, EM, NC, DCol, DCor, GF, EG, BI, TJ, TL, VS, CV, PV and MZ. HZ, LH, JK, HK, MSM, DS, AB, VP, DZ, JM and KMP performed and/or supervised analysis of patient samples. Analysis of patient data was performed by AG, IR and IG. MS, HW, KMP and NC drafted the manuscript and all authors contributed to and approved the final version.
Corresponding author
Ethics declarations
Competing interests
HEW, MS, GNF, KMP, TE, NCPC and AH received support from Novartis through the European Treatment and Outcome Study (EUTOS) for CML. HW has received honoraria from Novartis. GNF has received honoraria from BMS, Novartis and Pfizer. TL has received honoraria from Incyte, Novartis, Pfizer, Angelini, Bristol Myers Squibb and research support from Incyte, Novartis and Pfizer. PV has received honoraria from Astra-Zeneca, Eli Lilly, Gilead; GlaxoSmithKline, Novartis, Pfizer, Roche, Teva and research support from Novartis and Pfizer. IR has received research support from Bristol-Myers Squibb and honoraria from Bristol Myers-Squibb and Janssen-Cilag. IG has received research support from Bristol-Myers Squibb. AH received research support from Novartis, BMS, Pfizer and Incyte. KMP has received honoraria from Angelini and Incyte. NCPC has received research support and honoraria from Novartis, and honoraria from Incyte and Astellas.
Ethical approval
This work involving patient samples and data was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committees of the Institute of Haematology and Blood Transfusion, Prague and Faculty Hospital Brno. All patients provided written informed consent for the use of their samples for this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salmon, M., White, H.E., Zizkova, H. et al. Impact of BCR::ABL1 transcript type on RT-qPCR amplification performance and molecular response to therapy. Leukemia 36, 1879–1886 (2022). https://doi.org/10.1038/s41375-022-01612-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01612-2