Abstract
Causes of death in persons with haematological cancers include the index cancer, a new cancer or a seemingly unrelated cause such as cardio-vascular disease. These causes are complex and sometimes confounded. We analyzed trends in cause of death in 683,333 persons with an index haematological cancer diagnosed in 1975–2016 reported in the Surveillance, Epidemiology and End Results dataset. Non-cancer deaths were described using standardized mortality ratios. The index cancer was the predominant cause of death amongst persons with plasma cell myeloma, acute lymphoblastic leukaemia and acute myeloid leukaemia. Non-cancer death was the major cause of death in persons with chronic lymphocytic leukaemia, Hodgkin lymphoma and chronic myeloid leukaemia, mostly from cardio-vascular diseases. The greatest relative decrease in index-cancer deaths was amongst persons with Hodgkin lymphoma, chronic myeloid leukaemia and chronic lymphocytic leukaemia, where the proportion of non-cancer deaths increased substantially. Changing distribution of causes of death across haematological cancers reflects substantial progress in some cancers and suggests strategies to improve the survival of persons with haematological cancers in the future.
Similar content being viewed by others
Introduction
Haematological cancers are an important cause of death worldwide [1]. In 2020, there were an estimated 1.3 million new haematological cancers with 700,000 deaths worldwide. Incidences of most haematological cancers increase with age. The Global Burden of Disease (GBD) study reported that incidences of non-Hodgkin lymphoma (NHL) and leukaemias increased 45 percent and 26 percent from 2006 to 2016 [2].
There are substantial recent advances in therapy of some haematological cancers such as Hodgkin lymphoma (HL) and NHL, chronic myeloid and lymphocytic leukaemias (CML and CLL) and plasma cell myeloma (PCM) [3,4,5,6,7]. There are more modest recent advances in other haematological cancers such as acute myeloid and lymphoid leukaemias (AML and ALL). Much of this progress has resulted in increased survival rather than increased cures [8]. Survivors of cancer are at risk for a range of late-occurring side effects from treatment, which would also change the fate of these patients [9]. In older persons with a haematological cancer, increased survival after a cancer diagnosis may result in more deaths from age-related diseases such as cardio-vascular disease (CVD), stroke and diabetes.
Analyses of causes of death in persons with a haematological cancer are complex. For example, as deaths from some cancers such as HL have decreased the proportion of deaths from new cancers, such as therapy-related AML and CVD, have increased [10, 11]. In CML, where survival has increased substantially, the proportion of deaths from non-CML causes has increased markedly [12]. Sometimes there is uncertainty to identify the cause(s) of death in persons with a haematologic cancer. For example, some persons with AML receiving a haematopoietic cell transplant whilst in 1st remission die from transplant-related mortality, such as graft-versus-host disease (GvHD) [13]. If these persons were cured before they received a transplant, it is unknown whether the death should be scored as from AML, the transplant or GvHD.
We interrogated data from the Surveillance, Epidemiology and End Results (SEER) dataset 1975–2016 to assess the trends for cancer-related and 26 major types of non-cancer cause(s) of death of persons with a haematological cancer.
Subjects and methods
Data source and study population
We performed a population-based cohort study using data from the Surveillance, Epidemiology and End Results (SEER) programme, a population-based cancer registry with data on cancer demographics, incidence, anatomic site, histology, stage, therapy, socio-economic state and vital statistics of about one-third of persons with cancer in the US [14].
We extracted data on all first primary newly-diagnosed haematologic cancers diagnosed between 1975 and 2016 from the SEER 18 database (2019 Edition) using SEER*Stat software version 8.3.8 [15]. Diagnosis was based on coding in International Classification of Diseases for Oncology 3rd edition [ICD-O-3] codes, 9590–9992. Subjects were excluded if their diagnoses were obtained only from death certificates or autopsies. We also excluded subjects without active follow-up and those with unknown follow-up time, age at diagnosis and/or cause of death (Fig. S1). To analyze the causes of death as a function of calendar year of death, we extracted cause of death data amongst persons with a first haematological cancer diagnosis between 1975 and 2016 using the SEER-9 incidence-based mortality session [16]. For comparison with the general population, we extracted sex-, age-, race- and year-stratified mortality data of the US general population between 1975 and 2016 from the National Center for Health Statistics [17].
The Sun Yat-sen University Cancer Center (SYSUCC) Institutional Review Board (IRB) waived the requirement for a Research Data Agreement and informed consent consistent with principles of the Declaration of Helsinki.
Co-variates analyzed
Follow-up from diagnosis was defined as the interval between cancer diagnosis and death from any cause, last follow-up or the end of the study on December 31, 2016. Interrogated co-variates included sex, race, age at diagnosis, year of cancer diagnosis, cancer histology, follow-up duration and cause of death.
We classified haematological cancers by histology including: (1) HL (ICD-O-3 codes: 9650-9667); (2) NHL (ICD-O-3 codes: 9590-9597, 9670-9671, 9673, 9675, 9678-9680, 9684, 9687-9691, 9695, 9698-9702, 9705, 9708-9709, 9712, 9714-9719, 9724-9729, 9735, 9737-9738, 9811-9818, 9823, 9827, 9837); (3) PCM (ICD-O-3 codes: 9731-9732, 9734); (4) ALL (ICD-O-3 codes: 9811-9818, 9826, 9835-9837); (5) CLL (ICD-O-3 codes: 9823); (6) AML (ICD-O-3 codes: 9840, 9861, 9865-9867, 9869, 9871-9874, 9891, 9895-9897, 9898, 9910-9911, 9920); (7) CML (ICD-O-3 codes: 9863, 9875-9876, 9945-9946: and (8) other leukaemias (ICD-O-3 codes: 9733, 9742, 9800-9801, 9805-9809, 9820, 9831-9834, 9860, 9870, 9930-9931, 9940, 9948, 9963-9964).
Cause of death was defined using the International Statistical Classification of Diseases and Related Health Problems [ICD]. Because death codes changed over the interval we studied, we used ICD-8 codes for cases diagnosed from 1975 to 1978, ICD-9 codes for cases diagnosed from 1979 to 1998 and ICD-10 codes for cases diagnosed from 1999 to 2016. The SEER programme summarized these codes and generated a combined death code.
We classified causes of death into three groups: (1) index-cancer; (2) non-index-cancer; or (3) non-cancer. Causes of death were defined by SEER cause-specific death classification variable from death certificates [18, 19]. Non-cancer causes were categorized into 26 major groups which were consolidated into 7 broad categories: (1) infection; (2) CVD; (3) respiratory disease; (4) gastro-intestinal disease; (5) kidney disease; (6) external injuries; and (7) other. Deaths from in situ, benign or unknown behavior neoplasms are classified as non-cancer deaths by SEER programme [18, 19]. We did not include these deaths in the non-cancer deaths. These deaths also cannot be classified into cancer-related deaths; thus, they were excluded from our analyses (3,534 cases were excluded [0.5%]; Fig. S1). In the SEER programme, survival is measured in months. Subjects with survival < 1 month were recorded as 0 months according to standard epidemiologic convention [20].
Statistical analyses
Mortality rates were calculated as number of deaths divided by the person-years of follow-up. For non-cancer deaths, standardized mortality ratios (SMRs) and 95% Confidence Intervals (CIs) were calculated for comparison with the US population [19, 21]. SMR was estimated as ratio of observed to expected number of deaths. Observed number of deaths represents the number of deaths from certain causes in persons with cancer and expected number of deaths represents numbers of people dying from the same causes in the general population with a similar distribution of age, sex, race and calendar year. All-cause and cause-specific SMRs were calculated among patients with haematological cancer.
To obtain the expected number of deaths, we derived the stratum-specific mortality rates from the same cause in the reference general population collected by the SEER programme and calculated person-years of relevant strata in the haematological cancer cohort. The stratum-specific expected number of deaths was estimated as the product of death rate in the reference cohort and person-years in the haematological cancer cohort. Total expected number of deaths is the sum of all expected deaths across the strata.
Age at diagnosis was divided into 19 cohorts: (1) 00 years; (2) 01–04 years; (3) 05–09 years; (4) 10–14 years; (5) 15–19 years; (6) 20–24 years; (7) 25–29 years; (8) 30–34 years; (9) 35–39 years; (10) 40–44 years; (11) 45–49 years; (12) 50–54 years; (13) 55–59 years; (14) 60–64 years; (15) 65–69 years; (16) 70–74 years; (17) 75–79 years; (18) 80–84 years; and (19) 85+ years. Year of haematological cancer diagnosis was divided into 8 cohorts: (1) 1975–1979; (2) 1980–1984; (3) 1985–1989; (4) 1990–1994; (5) 1995–1999; (6) 2000–2004; (7) 2005–2009; and (8) 2010–2016. 95% confidence intervals (CIs) of SMRs were obtained using an approximation from a Poisson distribution [20, 22]. The Kaplan-Meier method was used to estimate actuarial probability of death amongst persons with a haematological cancer and competing risk analyses were done to estimate risk of dying from the index cancer, non-index cancer and non-cancer causes.
Data on deaths were extracted from SEER 9 registries databases which continually code death trends from diverse causes by calendar year of cancer diagnosis from 1975 to 2016. In the trend analyses, we restricted follow-up interval to avoid bias from different intervals of follow-up time for persons diagnosed in different periods. For example, subjects diagnosed 1975–1979 were followed to 1984 (an additional 5-year minimum duration), those diagnosed 1980–1984 were followed to 1989, and those diagnosed in 2010–2014 were followed to 2016. All deaths during follow-up were recorded. Cancers diagnosed 2015–2016 were excluded because of inadequate follow-up. Joinpoint Software was used to fit the trends of deaths from index cancer, non-index cancer and non-cancer causes [23]. Joinpoint Software generated one or more curves based on a log-linear regression model and so-called joinpoints, which were used to connect adjacent curves to generate a continuous curve spanning the study interval. Percentage change per 5 years for each trend was estimated and integrated to generate an average 5-year percentage change for the entire trend. We describe risk of death from non-cancer causes as a function of haematological cancer-type and interval from haematological cancer diagnosis.
Tests were two-sided and P-values < 0.05 were considered statistically significant. Analyses were done with SEER*Stat software version 8.3.6, the R version 3.63 statistical software, and Joinpoint Regression Software version 4.7.0.0 [15, 23, 24].
Results
683,333 persons with a haematological cancer diagnosed from 1975 to 2016 were included (Fig. S1). Median follow-up from index cancer diagnosis was 3 years (range, 0 to 42 years). 55 percent were male and 83 percent were white. Median age at diagnosis was 64 years (Inter-Quartile Range [IQR], 0–109 years). 46 percent had an NHL, 15 percent, PCM, 11 percent, CLL, 9 percent, AML, 5 percent, ALL, and 4 percent, CML. Baseline co-variates are displayed in Table 1.
Causes of death by calendar interval
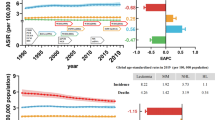
We analyzed death trends by assessing deaths from index cancer, other cancer or non-cancer causes by cancer type (Fig. 1). In persons diagnosed in 1975–1979, index-cancer deaths accounted for 65 percent of deaths, 2nd cancer for 15 percent and non-cancer deaths, 20 percent. In persons diagnosed in 2010–2014, index-cancer deaths decreased to 62 percent (p = 0.04), 2nd cancers decreased to 12 percent (p = 0.04) and non-cancer deaths increased to 26 percent (p = 0.02).
Persons most likely to die from their index cancer were those with PCM, ALL and AML. The proportion of deaths from index cancer remained stable or changed slightly for ALL (p = 0.5). For AML, there was a relative increase in index-cancer deaths beginning in 1985 (1975–1979 to 1985–1989: p = 0.2; 1985–1989 to 2010–2014: p = 0.01), with an insignificant overall trend (p = 0.07). In contrast, there was a marked decrease in index-cancer deaths in persons with HL, CML, CLL (HL: p < 0.001; CML: p < 0.001; CLL: p = 0.004) and a modest decrease in index-cancer deaths in persons with NHL and PCM (NHL: p = 0.02; PCM: p = 0.001;) (Fig. 1 and Table S1).
For HL, CML and CLL, non-cancer deaths increased continually 1975–2014 (HL: p = 0.01; CML: p < 0.001; CLL: p = 0.04). For PCM and ALL, although non-cancer deaths were less frequent, there was an increased trend (PCM: p = 0.001; ALL: p = 0.01). For NHL, non-cancer deaths increased substantially 1975-1994, and remaind stable thereafter (1975–1979 to 1990–1994: p = 0.07; 1990–1994 to 2010–2014: p = 0.5). Beginning in 1980s, non-cancer causes became the most common causes of death in persons with CLL (Fig. 1 and Table S1).
Non-index-cancer deaths increased in persons with HL, CLL (HL: PC = 5.41; p = 0.001; CLL: p = 0.03), but decreased in ALL and AML (ALL: p = 0.03; AML: p < 0.001) (Fig. 1 and Table S1).
Causes of death by cancer type
There were 390,534 deaths amongst 683,333 persons with a haematological cancer (57%) diagnosed 1975–2016. 56 percent of deaths were from the index cancer (N = 219,731), 15 percent from a 2nd cancer (N = 57,631) and 29 percent (N = 113,172) from non-cancer causes, predominately CVD (13%, N = 49,498) (Table 2). The 10-year actuarial rate of all-cause deaths was 57.8% (57.6%, 57.9%). 10-year actuarial rates were 35.0% (34.9%, 35.2%) for index-cancer deaths, 8.7% (8.6%, 8.7%) for non-index-cancer deaths, and 16.9% (16.7%, 17.0%) for non-cancer deaths (Fig. 2).
The all-cause SMR for non-cancer deaths was 2.51 (2.49, 2.52) compared with the general population. Compared with cause-specific mortality in the general population, risks were highest for infections and kidney diseases, with cause-specific SMRs of 6.51 (6.42, 6.61) and 3.46 (3.34, 3.58), respectively. There were also increased risks of death for pregnancy, childbirth and puerperium complications (cause-specific SMR = 17.7 [13.6, 23.2]) (Table 2).
Index-cancer deaths
The index cancer accounted for a large proportion of deaths in persons with i PCM (70%), AML (68%), ALL (66%), NHL (54%), CML (52%), and for a smaller proportion of deaths in persons with HL (39%) and CLL (33%) (Fig. 3; Table S1 to S7). 10-year actuarial rates of index-cancer deaths were 58.9% (58.5%, 59.2%) for PCM, 57.1% (56.7%, 57.5%) for AML, 35.7% (35.0%, 36.3%) for CML, 32.2% (32.0%, 32.4%) for NHL, 27.3% (26.8%, 27.8%) for ALL, 20.1% (19.7%, 20.4%) for CLL and 12.5% (12.2%, 12.8%) for HL (Fig. 2).
Non-index cancer deaths
Non-index cancer accounted for a large proportion of deaths in persons with HL (24%), CLL (23%), ALL (23%) and AML (22%) and for a smaller proportion of deaths in persons with NHL (13%) and PCM (6%; Fig. 3, Tables S2–S8). 10-year actuarial rates of non-index-cancer deaths were 17.3% (17.0%, 17.6%) for AML, 13.3% (13.0%, 13.6%) for CLL, 10.6% (10.2%, 11.0%) for CML, 8.8% (8.5%, 9.2%) for ALL, 6.8% (6.7%, 6.9%) for NHL, 5.5% (5.3%, 5.7%) for HL and 4.5% (4.3%, 4.6%) for PCM (Fig. 2).
Non-cancer causes of death
Non-cancer causes were the cause of death in persons with CLL (44%), HL (38%), NHL (33%), CML (29%), PCM (24%), ALL (11%) and AML (10%; Fig. 3, Tables S2–S8). The all-cause SMR of non-cancer deaths was highest in persons with ALL (all-cause SMR = 5.25 [4.97, 5.55) followed by AML (all-cause SMR = 5.13 [4.99, 5.28) and HL (all-cause SMR = 3.80 [3.71, 3.90]; Fig. 4A). 10-year actuarial rates of non-index-cancer deaths were 25.1% (24.8%, 25.5%) for CLL, 19.7% (19.4%, 20.0%) for PCM, 19.7% (19.2%, 20.3%) for CML, 18.0% (17.9%, 18.2%) for NHL, 8.8% (8.6%, 9.1%) for HL, 8.0% (7.8%, 8.3%) for AML and 4.2% (4.0%, 4.5%) for ALL (Fig. 2).
Infections were a cause of non-cancer deaths with exceeding risks in several cancers including ALL (cause-specific SMR = 19 [17, 21), AML (cause-specific SMR = 13 [12, 14]) and HL (cause-specific SMR = 10 [9.5, 10.7]; Fig. 4, Tables S2–S8). CVD was a common non-cancer cause of death in several cancers including CLL (22%), HL (15%), NHL (14%), CML (14%) and PCM (12%; Fig. 3, Tables S2–S8). CVD was associated with the highest SMRs in ALL (cause-specific SMR = 4.22 [3.78, 4.72), AML (cause-specific SMR = 3.89 [3.71, 4.08]) and HL (cause-specific SMR = 3.68 [3.54, 3.83; Figs. 3 and 4C, Tables S2–S8). Cause-specific SMRs for respiratory deaths was high in HL (cause-specific SMR = 3.73 [3.35, 4.17]) and for kidney disease in PCM (cause-specific SMR = 6.96; [6.55, 7.41; Fig. 4).
Cause of death per interval after diagnosis
The interval immediately after a haematological cancer diagnosis had the highest risk of index-cancer-specific deaths except for CLL (Fig. 5). Subsequently, the likelihood of deaths from non-cancer causes increased in long-term survivors. In CLL, non-cancer causes were the leading cause of death regardless of post-diagnosis interval (Fig. 5). Persons with cancer had higher SMRs compared with the general population throughout the follow-up interval (Fig. 6). Most cancer types had high all-cause SMRs of non-cancer deaths in the 1st year after the haematological cancer diagnosis. All-cause SMRs decreased slightly during the next 4 years and then either decreased slightly or increased thereafter. For some non-cancer causes, the cause-specific SMR was highest in the 1st year after diagnosis including infections and external injuries. For other non-cancer causes, the cause-specific SMR in the interval after 5 years after haematological cancer diagnosis was like that or less than in the 5 years following diagnosis including CVD and respiratory and kidney diseases. People with newly-diagnosed ALL and AML had the highest all-cause SMRs of non-cancer deaths in the 1st year after diagnosis. We also observed extremely high cause-specific SMR for infections and external injuries in persons with newly-diagnosed HL whereas an extremely high cause-specific SMR for respiratory disease was seen in long-term HL survivors. Trends are displayed in Fig. 6.
Discussion
We analyzed causes of death amongst 686,867 persons with haematologic cancers registered in SEER 1975-2016. Non-cancer deaths now exceed index-cancer deaths in CLL and will likely surpass index-cancer deaths soon in HL and CML. Causes of death varied by era of cancer diagnosis, cancer type, interval after diagnosis to death and other co-variates, including age and race. As cancer therapy has improved, new cancers and non-cancer causes of death are increasing in long-term cancer survivors.
We found risk of death from the index cancer, another cancer and non-cancer causes has changed for some but not all haematological cancers. As people with haematological cancer survive longer, risks of death from a new cancer and those from age-related non-cancer causes increase. There are many reasons why death from an index haematological cancer might decrease, including earlier diagnosis, better therapies, increased access to health care and others including changes in how deaths are coded and reported. Our analyses focused on characterizing cause of death amongst people with haematological cancer, not elucidating the reasons of changes which are likely complex. Such an analysis requires detailed subject-level data which are generally unavailable in population-based cancer registries such as SEER.
Our study is comprehensive but has several limitations. First, it is descriptive and retrospective. Second, cause of death may have been mis-classified because of inaccurate coding of death certificates in different intervals. This is an unlikely cause of substantial bias [25,26,27,28]. Rules for coding deaths changed during our study interval. It is also possible there might be a difference in accuracy of the cause of death in different cancers and non-cancer causes. Nevertheless, the SEER programme used standardized data collection procedures to ensure accuracy [28]. This approach has been validated [25,26,27, 29, 30].
Conclusion
Risk of death from an index cancer, new cancer or non-cancer causes varied by haematological cancer type, era of diagnosis, interval after diagnosis and other co-variates including age and race. Non-cancer deaths now exceed index-cancer deaths in CLL and will become dominants soon in HL and CML. Index-cancer deaths remained dominant cause of death amongst persons with PCM, ALL and AML in the 2010s. Changes in causes of death amongst people with different haematological cancers suggest distinct strategies to improve survival, such as increased screening for new cancers or non-cancer comorbidities. Non-cancer deaths might be decreased, prevented or effectively treated, especially in persons with CLL, HL and CML. In other haematological cancers including PCM, ALL and AML, preventing death from the index cancer remains the most pressing goal.
Data availability
Data can be accessed from the Surveillance, Epidemiology, and End Results (SEER) database at https://seer.cancer.gov/data/.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Global Burden of Disease Cancer C, Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: A systematic analysis for the global burden of disease study. JAMA Oncol. 2018;4:1553–68.
Wang L, Qin W, Huo YJ, Li X, Shi Q, Rasko JEJ, et al. Advances in targeted therapy for malignant lymphoma. Signal Transduct Target Ther. 2020;5:15.
Evens AM, Hutchings M, Diehl V. Treatment of Hodgkin lymphoma: The past, present, and future. Nat Clin Pr Oncol. 2008;5:543–56.
Hunter AM, Zhang L, Padron E. Current management and recent advances in the treatment of chronic myelomonocytic leukemia. Curr Treat Options Oncol. 2018;19:67.
Bosch F, Dalla-Favera R. Chronic lymphocytic leukaemia: From genetics to treatment. Nat Rev Clin Oncol. 2019;16:684–701.
Du J, Zhuang J. Major advances in the treatment of multiple myeloma in American Society of Hematology annual meeting 2020. Chronic Dis Transl Med. 2022;7:220–6.
Maslak P, Scheinberg D. Targeted therapies for the myeloid leukaemias. Expert Opin Investig Drugs. 2000;9:1197–205.
Tonorezos ES, Cohn RJ, Glaser AW, Lewin J, Poon E, Wakefield CE, et al. Long-term care for people treated for cancer during childhood and adolescence. Lancet. 2022;399:1561–72.
Al-Juhaishi T, Khurana A, Shafer D. Therapy-related myeloid neoplasms in lymphoma survivors: Reducing risks. Best Pr Res Clin Haematol. 2019;32:47–53.
van Nimwegen FA, Schaapveld M, Janus CP, Krol AD, Petersen EJ, Raemaekers JM, et al. Cardiovascular disease after Hodgkin lymphoma treatment: 40-year disease risk. JAMA Intern Med. 2015;175:1007–17.
Wang Q, Jiang C, Zhang Y, Zhang Y, Yue B, Zheng-Lin B, et al. Cardiovascular mortality among chronic myeloid leukemia patients in the pre-tyrosine kinase inhibitor (TKI) and TKI eras: a surveillance, epidemiology and end results (SEER) analysis. Leuk Lymphoma. 2020;61:1147–57.
Gassas A, Sivaprakasam P, Cummins M, Breslin P, Patrick K, Slatter M, et al. High transplant-related mortality associated with haematopoietic stem cell transplantation for paediatric therapy-related acute myeloid leukaemia (t-AML). A study on behalf of the United Kingdom Paediatric Blood and Bone Marrow Transplant Group. Bone Marrow Transpl. 2018;53:1165–9.
Surveillance, Epidemiology, and End Results (SEER) Program. The SEER databse. Available at http://www.seer.cancer.gov. Accessed on March, 2020.
Surveillance Research Program, National Cancer Institute SEER*Stat software (www.seer.cancer.gov/seerstat) version 8.3.8.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence-Based Mortality - SEER 9 Regs Research Data, Nov 2018 Sub (1975-2016) <Katrina/Rita Population Adjustment> - Linked To County Attributes - Total U.S., 1969-2017 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2019, based on the November 2018 submission.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Mortality - All COD, Aggregated With State, Total U.S. (1969-2017) <Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, released December 2019. Underlying mortality data provided by NCHS (www.cdc.gov/nchs).
Anderson C, Lund JL, Weaver MA, Wood WA, Olshan AF, Nichols HB. Noncancer mortality among adolescents and young adults with cancer. Cancer. 2019;125:2107–14.
Chen J, Zheng Y, Wang H, Zhang D, Zhao L, Yu D, et al. Cause of death among patients with colorectal cancer: a population-based study in the United States. Aging (Albany NY). 2020;12:22927–48.
Koepsell TD, Weiss NS. Epidemiologic Methods: Studying the Occurrence of Illness. Oxford University Press: New York, 2003.
Yang K, Zheng Y, Peng J, Chen J, Feng H, Yu K, et al. Incidence of death from unintentional injury among patients with cancer in the United States. JAMA Netw Open. 2020;3:e1921647.
Ury HK, Wiggins AD. Another shortcut method for calculating the confidence interval of a Poisson variable (or of a standardized mortality ratio). Am J Epidemiol. 1985;122:197–8.
Joinpoint Regression Program, Version 4.7.0.0. February, 2019; Statistical Research and Applications Branch, National Cancer Institute.
R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available at https://www.R-project.org/. Accessed on December, 2019.
Lloyd-Jones DM, Martin DO, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–6.
Coady SA, Sorlie PD, Cooper LS, Folsom AR, Rosamond WD, Conwill DE. Validation of death certificate diagnosis for coronary heart disease: The Atherosclerosis Risk in Communities (ARIC) Study. J Clin Epidemiol. 2001;54:40–50.
Moyer LA, Boyle CA, Pollock DA. Validity of death certificates for injury-related causes of death. Am J Epidemiol. 1989;130:1024–32.
Park HS, Lloyd S, Decker RH, Wilson LD, Yu JB. Overview of the surveillance, epidemiology, and end results database: Evolution, data variables, and quality assurance. Curr Probl Cancer. 2012;36:183–90.
Lund JL, Harlan LC, Yabroff KR, Warren JL. Should cause of death from the death certificate be used to examine cancer-specific survival? A study of patients with distant stage disease. Cancer Invest. 2010;28:758–64.
Hu CY, Xing Y, Cormier JN, Chang GJ. Assessing the utility of cancer-registry-processed cause of death in calculating cancer-specific survival. Cancer. 2013;119:1900–7.
Acknowledgements
Prof. Tomas Radivoyevitch (Cleveland Clinic) provided helpful comments. for his valuable comments. RPG acknowledges support from the National Institute of Health Research (NIHR) Biomedical Research Centre funding scheme. YL is supported, in part, by Sun Yat-sen University Start-up Funding, grant no. 201603, the Program for Guangdong Introducing Innovative and Entrepreneurial Teams (2017ZT07S096) and the National Natural Science Foundation of China (Grant No. 81873428).
Author information
Authors and Affiliations
Contributions
YL and RPG designed the study. LC, YZ, KY, and SC performed the research. YL, LC, RPG, and ZXL developed the typescript. The authors approved the typescript, accept responsibility for the content and agreed to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
RPG is a Consultant to BeiGene Ltd., CStone Pharmaceuticals and Kite Pharmma; a Consultant to Fusion Pharma LLC, LaJolla NanoMedical Inc. and Mingsight Parmaceuticals Inc.; an Advisory Board member for Antegene Biotech LLC and StemRad Ltd; Medical Director at FFF Enterprises Inc; Partner in AZACA Inc; and on the Board of Directors of the Russian Foundation for Cancer Research Support.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, L., Zheng, Y., Yu, K. et al. Changing causes of death in persons with haematological cancers 1975–2016. Leukemia 36, 1850–1860 (2022). https://doi.org/10.1038/s41375-022-01596-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01596-z