Abstract
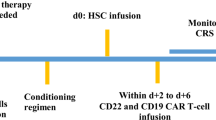
Relapse of B-cell precursor acute lymphoblastic leukemia (BCP-ALL) may occur in the central nervous system (CNS). Most clinical trials of CAR T-cell therapy excluded patients with active CNS leukemia, partially for concerns of neurotoxicity. Here, we report an international study of fifty-five children and adolescents who received CAR T-cell therapy for relapsed BCP-ALL with CNS involvement at the time of referral. All patients received bridging therapy, 16 still having active CNS disease at the time of lymphodepletion. Twelve patients received CD28-based CAR T-cells, 9 being subsequently treated with allogeneic hematopoietic stem-cell transplantation (allo-HSCT). Forty-three patients received 4-1BB-based CAR T-cells. Cytokine-release syndrome (CRS) and neurotoxicity occurred in 65% and 38% of patients, respectively, more frequently following treatment with CD28-based CARs. Fifty-one of 54 evaluable patients (94%) achieved complete response following this therapy. Relapse occurred in 22 patients: 19/43 following 4-1BB-based CARs (12 CNS relapses), and 3/12 after CD28-based CARs with subsequent HSCT (no CNS relapse). Patients treated with tisagenlecleucel for an isolated CNS relapse had a high incidence of a subsequent CNS relapse (6 of 8). CAR T-cells were found to be effective in this cohort, though the risk of CNS relapse was not completely mitigated by this approach.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Evans AE, Gilbert ES, Zandstra R. The increasing incidence of central nervous system leukemia in children. (Children’s Cancer Study Group A). Cancer. 1970;26:404–9.
Hunger SP, Mullighan CG. Acute Lymphoblastic Leukemia in children. N. Engl J Med. 2015;373:1541–52.
Goldsby RE, Liu Q, Nathan PC, Bowers DC, Yeaton-Massey A, Raber SH, et al. Late-occurring neurologic sequelae in adult survivors of childhood acute lymphoblastic leukemia: a report from the childhood cancer survivor study. J Clin Oncol. 2010;28:324–31.
Pui C-H, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N. Engl J Med. 2009;360:2730–41.
Liu HC, Yeh TC, Hou JY, Chen KH, Huang TH, Chang CY, et al. Triple intrathecal therapy alone with omission of cranial radiation in children with acute lymphoblastic leukemia. J Clin Oncol. 2014;32:1825–9.
Masurekar AN, Parker CA, Shanyinde M, Moorman AV, Hancock JP, Sutton R, et al. Outcome of central nervous system relapses in childhood acute lymphoblastic Leukaemia - Prospective open cohort analyses of the ALLR3 trial. PLoS ONE. 2014;9. https://doi.org/10.1371/journal.pone.0108107.
Tallen G, Ratei R, Mann G, Kaspers G, Niggli F, Karachunsky A, et al. Long-term outcome in children with relapsed acute lymphoblastic leukemia after time-point and site-of-relapse stratification and intensified short-course multidrug chemotherapy: results of trial ALL-REZ BFM 90. J Clin Oncol. 2010;28:2339–47.
Barredo JC, Devidas M, Lauer SJ, Billett A, Marymont M, Pullen J, et al. Isolated CNS relapse of acute lymphoblastic leukemia treated with intensive systemic chemotherapy and delayed CNS radiation: a pediatric oncology group study. J Clin Oncol. 2006;24:3142–9.
Winick NJ, Smith SD, Shuster J, Lauer S, Wharam MD, Land V, et al. Treatment of CNS relapse in children with acute lymphoblastic leukemia: a pediatric oncology group study. J Clin Oncol. 1993;11:271–8.
Brown PA, Ji L, Xu X, Devidas M, Hogan L, Bhatla T, et al. A Randomized Phase 3 Trial of Blinatumomab Vs. Chemotherapy As Post-Reinduction Therapy in Low Risk (LR) First Relapse of B-Acute Lymphoblastic Leukemia (B-ALL) in Children and Adolescents/Young Adults (AYAs): A Report from Children’s Oncology Group Study. Blood. 2021;138:363–363.
Maude SL, Latesch T, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-Cell Lymphoblastic Leukemia. N. Engl J Med. 2018;378:439–48.
Pasquini MC, Hu Z, Curran K, Laetsch T, Locke F, Rouce R, et al. Real-world evidence of tisagenlecleucel for pediatric acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Adv. 2020;4:5414–24.
Lee DW, Kochenderfer JN, Stetler-Stevenson M, Cui YK, Delbrook C, Feldman SA, et al. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet. 2015;385:517–28.
Gardner RA, Finney O, Annesley C, Brakke H, Summers C, Leger K, et al. Intent to treat leukemia remission by CD19 CAR T cells of defined formulation and dose in children and young adults. Blood. 2017;129:3322–31.
Jacoby E, Bielorai B, Avigdor A, Itzhaki O, Hutt D, Nussboim V, et al. Locally produced CD19 CAR T cells leading to clinical remissions in medullary and extramedullary relapsed acute lymphoblastic leukemia. Am J Hematol. 2018;93:1485–92.
Gust J, Hay KA, Hanafi L-A, Li D, Myerson D, Gonzalez-Cuyar LF, et al. Endothelial activation and blood–brain barrier disruption in neurotoxicity after adoptive immunotherapy with CD19 CAR-T Cells. Cancer Disco. 2017;7:1404–19.
Rubin DB, Danish HH, Ali AB, Li K, Larose S, Monk AD, et al. Neurological toxicities associated with chimeric antigen receptor T-cell therapy. Brain. 2019;142:1334–48.
Parker KR, Migliorini D, Perkey E, Yost KE, Bhaduri A, Bagga P.et al. Single-. Cell Analyses Identify Brain Mural Cells Expressing CD19 Potential -Tumor Targets CAR-T Immunotherapies Cell. 2020;183:126–142.e17..
Lee DW, Santomasso BD, Locke FL, Ghobadi A, Turtle CJ, Brudno JN, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transpl. 2019;25:625–38.
Dourthe M, Rabian F, Yakouben K, Chevillon F, Méchinaud F, Grain A, et al. Determinants of CD19-positive vs CD19-negative relapse after tisagenlecleucel for B-cell acute lymphoblastic leukemia. Leukemia. 2021;35:3383–93.
Schultz LM, Baggott C, Prabhu S, Pacenta H, Phillips CL, Rossoff J, et al. Disease burden impacts outcomes in pediatric and young adult B-Cell acute lymphoblastic leukemia after commercial tisagenlecleucel: results from the pediatric real world CAR consortium (PRWCC). Blood. 2020;136:14–5.
Abramson JS, McGree B, Noyes S, Plummer S, Wong C, Chen Y-B, et al. Anti-CD19 CAR T cells in CNS diffuse large-B-cell lymphoma. N. Engl J Med. 2017;337:23–4.
Frigault MJ, Dietrich J, Martinez-Lage M, Leick M, Choi BD, DeFilipp Z, et al. Tisagenlecleucel CAR-T Cell Therapy in Secondary CNS Lymphoma. Blood. 2019;134:860–6.
Ghafouri S, Timmerman J, Larson S, Mead MD. Axicabtagene Ciloleucel CAR T-cell therapy for relapsed/refractory secondary CNS non-Hodgkin lymphoma: comparable outcomes and toxicities, but shorter remissions may warrant alternative consolidative strategies? Bone Marrow Transplant. 2021;56:974–7.
Shah NN, Lee DW, Yates B, Yuan CM, Shalabi H, Martin S, et al. Long-term follow-up of CD19-CAR T-cell therapy in children and young adults with B-ALL. J Clin Oncol. 2021;39:1650–9.
Hay KA, Gauthier J, Hirayama AV, Voutsinas JM, Wu Q, Li D, et al. Factors associated with durable EFS in adult B-cell ALL patients achieving MRD-negative CR after CD19 CAR-T cells. Blood. 2019;133:1652–63.
Leahy AB, Newman H, Li Y, Liu H, Myers R, DiNofia A, et al. CD19-targeted chimeric antigen receptor T-cell therapy for CNS relapsed or refractory acute lymphocytic leukaemia: a post-hoc analysis of pooled data from five clinical trials. Lancet Haematol. 2021;8:e711–22.
Funding
This work was done on behalf of the international BFM Resistant Disease study group. This study was funded by the Dotan research center in hemato-oncology and by the Israel Cancer Association.
Author information
Authors and Affiliations
Contributions
EJ, JPB and AB conceived the study and oversaw the project; EJ, SG, BV, BDM, NB, OM, AY, JB, RE, BB, SR, ED, MM, CR, AT, AVS, FL, PB, JPB and AB collected patient data. EJ and MZ performed statistical analysis, EJ, MZ and AB analyzed and interpreted data; EJ, AB, SG, BV and BDM wrote and significantly revised the manuscript. All authors approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
This study was not supported by phama but by a NPO grant (ICA to Dr. Jacoby). EJ reports participation of advisory boards for Novartis and Lonza and speaker’s fee from Novartis. SG reports honoraria and conference support from Novartis. BDM reports participation of advisory boards for Novartis, NB reports speaker’s fee from Novartis. JB has received personal fees, advisory board/steering committee honoraria, and nonfinancial support from Novartis; and advisory board honoraria from Pfizer, Kite, and Janssen. MM reports speaker’s fee from Miltenyi. CR reports participation in advisory boards by Amgen, BMS, Celgene, Novartis and Pfizer. AB reports participation on advisory boards and travel from Servier, Celgene, Novartis, Jazz, AstraZeneca, and being an investigator on trials from Novartis, Kite, Celgene and Cellectis. BV, OM, AY, RE, BB, SR, ED, AT, AVS, FL, PB, and JPB report no conflict of interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jacoby, E., Ghorashian, S., Vormoor, B. et al. CD19 CAR T-cells for pediatric relapsed acute lymphoblastic leukemia with active CNS involvement: a retrospective international study. Leukemia 36, 1525–1532 (2022). https://doi.org/10.1038/s41375-022-01546-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01546-9
This article is cited by
-
Acute Lymphoblastic Leukemia with Central Nervous System Involvement—Challenges in Management
Indian Journal of Pediatrics (2024)
-
Immuntherapien bei Kindern und Jugendlichen mit akuter lymphoblastischer Leukämie und hochmalignen Lymphomen
Pädiatrie & Pädologie (2023)
-
Central nervous system involvement in childhood acute lymphoblastic leukemia: challenges and solutions
Leukemia (2022)