Abstract
Objective
Determine the association between severe hypertensive disease of pregnancy (HDP) with moderate-severe bronchopulmonary dysplasia (BPD) in preterm infants (< 31 weeks’ gestation).
Study Design
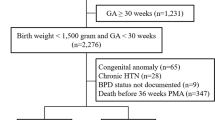
Preterm birth cohort study of 693 mother-infant dyads. Severe HDP was defined as severe preeclampsia, HELLP syndrome or eclampsia. The outcome was moderate-severe BPD classified at 36 weeks corrected gestational age, per the NICHD Consensus statement.
Results
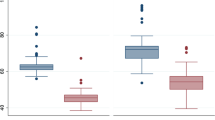
225 (32%) mothers developed severe HDP and 234 (34%) infants had moderate-severe BPD. There was an interaction between severe HDP and gestational age (p = 0.03). Infants born at < 25 weeks gestation to mothers with HDP had increased odds for moderate-severe BPD compared to infants of normotensive mothers delivering at the same gestational age. Infants born > 28 weeks to mothers with severe HDP had decreased odds for the outcome, though not statistically significant.
Conclusions
Severe HDP has a differential effect on the development of moderate-severe BPD based on gestational age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
A de-identified analytic dataset to replicate the reported study findings are available at Mendeley Data, V1, https://doi.org/10.17632/b8trr3xh37.1.
References
Mathews TJ, MacDorman MF. Infant mortality statistics from the 2005 period linked birth/infant death data set. Natl Vital Stat Rep. 2008;57:1–32.
Northway WH Jr., Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68.
Jobe AJ. The new BPD: an arrest of lung development. Pediatr Res. 1999;46:641–3.
Abman SH. Bronchopulmonary dysplasia: “a vascular hypothesis”. Am J Respir Crit Care Med. 2001;164:1755–6.
Thebaud B, Abman SH. Bronchopulmonary dysplasia: where have all the vessels gone? Roles of angiogenic growth factors in chronic lung disease. Am J Respir Crit Care Med. 2007;175:978–85.
Kinsella JP, Greenough A, Abman SH. Bronchopulmonary dysplasia. Lancet. 2006;367:1421–31.
Mourani PM, Sontag MK, Younoszai A, Miller JI, Kinsella JP, Baker CD, et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2015;191:87–95.
Heron M, Sutton PD, Xu J, Ventura SJ, Strobino DM, Guyer B. Annual summary of vital statistics: 2007. Pediatrics. 2010;125:4–15.
Zhou Y, McMaster M, Woo K, Janatpour M, Perry J, Karpanen T, et al. Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am J Pathol. 2002;160:1405–23.
Phipps EA, Thadhani R, Benzing T, Karumanchi SA. Pre-eclampsia: pathogenesis, novel diagnostics and therapies. Nat Rev Nephrol. 2019;15:275–89.
Tang JR, Karumanchi SA, Seedorf G, Markham N, Abman SH. Excess soluble vascular endothelial growth factor receptor-1 in amniotic fluid impairs lung growth in rats: linking preeclampsia with bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2012;302:L36–46.
Thebaud B, Lacaze-Masmonteil T. If your placenta doesn’t have it, chances are your lungs don’t have it either: the “vascular hypothesis” of bronchopulmonary dysplasia starts in utero. J Pediatr. 2010;156:521–3.
Mestan KK, Check J, Minturn L, Yallapragada S, Farrow KN, Liu X, et al. Placental pathologic changes of maternal vascular underperfusion in bronchopulmonary dysplasia and pulmonary hypertension. Placenta. 2014;35:570–4.
Rozance PJ, Seedorf GJ, Brown A, Roe G, O’Meara MC, Gien J, et al. Intrauterine growth restriction decreases pulmonary alveolar and vessel growth and causes pulmonary artery endothelial cell dysfunction in vitro in fetal sheep. Am J Physiol Lung Cell Mol Physiol. 2011;301:L860–71.
Hansen AR, Barnes CM, Folkman J, McElrath TF. Maternal preeclampsia predicts the development of bronchopulmonary dysplasia. J Pediatr. 2010;156:532–6.
Ozkan H, Cetinkaya M, Koksal N. Increased incidence of bronchopulmonary dysplasia in preterm infants exposed to preeclampsia. J Matern Fetal Neonatal Med. 2012;25:2681–5.
Eriksson L, Haglund B, Odlind V, Altman M, Kieler H. Prenatal inflammatory risk factors for development of bronchopulmonary dysplasia. Pediatr Pulmonol. 2014;49:665–72.
Gemmell L, Martin L, Murphy KE, Modi N, Hakansson S, Reichman B, et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J Perinatol. 2016;36:1067–72.
O’Shea JE, Davis PG, Doyle LW. Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants. Pediatr Res. 2012;71:210–4.
Yen TA, Yang HI, Hsieh WS, Chou HC, Chen CY, Tsou KI, et al. Preeclampsia and the risk of bronchopulmonary dysplasia in VLBW infants: a population based study. PLoS ONE. 2013;8:e75168.
Fierson WM. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131:189–95.
Cao JH, Wagner BD, McCourt EA, Cerda A, Sillau S, Palestine A, et al. The Colorado-retinopathy of prematurity model (CO-ROP): postnatal weight gain screening algorithm. J AAPOS. 2016;20:19–24.
Lynch AM, Wagner BD, Hodges JK, Thevarajah TS, McCourt EA, Cerda AM, et al. The relationship of the subtypes of preterm birth with retinopathy of prematurity. Am J Obstet Gynecol. 2017;217:354.e1–.e8.
Weinstein L. It has been a great ride: the history of HELLP syndrome. Am J Obstet Gynecol. 2005;193:860–3.
Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013;122:1122–31.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A. Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol. 2003;23:451–6.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Hackam D, Caplan M. Necrotizing enterocolitis: Pathophysiology from a historical context. Semin Pediatr Surg. 2018;27:11–8.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Redline RW. Inflammatory response in acute chorioamnionitis. Semin Fetal Neonatal Med. 2012;17:20–5.
Razak A, Florendo-Chin A, Banfield L, Abdul Wahab MG, McDonald S, Shah PS, et al. Pregnancy-induced hypertension and neonatal outcomes: a systematic review and meta-analysis. J Perinatol. 2018;38:46–53.
Soliman N, Chaput K, Alshaikh B, Yusuf K. Preeclampsia and the risk of bronchopulmonary dysplasia in preterm infants less than 32 weeks’ gestation. Am J Perinatol. 2017;34:585–92.
Vora N, Raju M, Jackson I, Mallett L, Samson S, Malhotra S, et al. Maternal preeclampsia as a risk factor for developing bronchopulmonary dysplasia in neonates. Minerva Pediatr (Torino). 2022. https://doi.org/10.23736/S2724-5276.22.07019-7. Online ahead of print.
Wilmink FA, Reijnierse J, Reiss IKM, Steegers EAP, de Jonge RCJ. Preeclampsia and risk of developing bronchopulmonary dysplasia in very preterm neonates. Pregnancy Hypertens. 2019;15:57–63.
Levine RJ, Karumanchi SA. Circulating angiogenic factors in preeclampsia. Clin Obstet Gynecol. 2005;48:372–86.
Acknowledgements
The authors acknowledge the generous institutional support by the University of Colorado Department of Ophthalmology and Pediatric Ophthalmology for the multidisciplinary team of the Colorado Retinopathy of Prematurity (CO-ROP) Research Group. Presentations: Presented in part at the Pediatric Academic Societies (PAS) Meeting, May 6-7, 2017, San Francisco, CA.
Funding
This project was supported in part by the Colorado Clinical and Translational Sciences Institute (CCTSI). The CCTSI is supported in part by the Colorado Clinical and Translational Science Award (CTSA) Grant UL1 TR002535, KL2 TR002534, and TL1 TR002533 from NCATS/NIH.
Author information
Authors and Affiliations
Contributions
EMW designed the study, data analysis and interpretation, wrote and finalized the manuscript. AML designed and supervised the study, data analysis, and finalization of the manuscript. TST and EA performed data abstraction and managed the database. JKS, JKH and JPK provided content expertize for study design, data interpretation and the manuscript. BDW developed the statistical analysis and interpretation and finalized the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wymore, E.M., Lynch, A.M., Singh, J.K. et al. The relationship between severe hypertensive diseases of pregnancy and moderate-severe bronchopulmonary dysplasia. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01910-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01910-w