Abstract
The prevalence of pregnancy-induced hypertension (PIH) and preeclampsia (PE) are 5–10% and 2–4%, respectively. PIH might affect angiogenesis in preterm neonates, but its association with bronchopulmonary dysplasia (BPD) remains controversial. This study evaluated the association between PIH and BPD in very low-birth weight infants. We retrospectively analysed the maternal, perinatal, and neonatal data of preterm infants born before 30 weeks of gestation, selected from the nationwide registry of very low-birth weight infants, between January 2013 and December 2014. As a result, 1,624 infants without maternal PIH (gestational age: 27.3 ± 1.8 weeks) and 203 infants with maternal PIH (28.0 ± 1.4 weeks, p < 0.001) were included. Birth weight was higher in the non-PIH group, compared with the PIH group (1027.4 ± 250.2 vs. 876.4 ± 261.5 g, p < 0.001). Multivariate logistic regression showed that PIH was associated with BPD (adjusted OR 1.474, 95% confidence interval 1.025–2.121), after adjusting for confounders, including small-for-gestation age (SGA). The result of present study is consistent with the current concept of BPD as an early form of pulmonary vascular disease, for both PIH and BPD are attributed by abnormal vascular formation.
Similar content being viewed by others
Introduction
Bronchopulmonary dysplasia (BPD) is the most common complication of preterm birth among very low-birth weight (VLBW) infants. Although the progression of prematurity care, including the use of antenatal steroids and surfactant therapy, has improved neonatal outcomes, the incidence of BPD has not decreased with the increased survival of preterm infants1,2,3,4. These extremely preterm infants present with arrest in the development of the alveolar-capillary unit, characterized by enlarged and simplified alveolar structure, prominent interstitial fibrosis, and abnormal pulmonary vasculature5. For angiogenesis and alveolar development are interactive in the foetal lung, BPD has been recently recognized as a manifestation of vascular disease of the lungs in this population6.
The prevalence of pregnancy-induced hypertension (PIH) and preeclampsia (PE) are 5–10% and 2–4%, respectively7,8,9,10. Although the pathophysiology of PIH and PE are not established, inadequate placental implantation and abnormal vascularization might play certain roles in the development of PIH11. Several maternal angiogenic factors and anti-angiogenic factors regulate placental growth and vascular development in PE12,13,14. Inappropriate vascular endothelial growth factor (VEGF) signalling could also alter vascular development and reactivity in foetus, leading to neonatal pulmonary vascular disease15. In a clinical study, the pulmonary outcomes of preterm infants were predicted by measurements of the placental growth factor from the mother16. Since both PIH and BPD are associated with abnormal angiogenesis, there has been efforts to evaluate the association between PIH and BPD in preterm infants. A small prospective study showed that moderate to severe BPD was more prevalent in preterm infants born at less than 32 weeks of gestation, to mothers with PE17. A recent meta-analysis and international cohort study also reported that PIH was associated with BPD18,19.
On the other hand, a meta-analysis of three cohorts in Austria reported that PE was not associated with BPD20. Another large population-based study also reported that preeclampsia decreased the risk for BPD in VLBW infants21. This study demonstrated a negative association between PE and BPD only in the group with a gestational age (GA) of more than 31 weeks. However, as hypertensive disorders in pregnancy are greatly associated with small-for-gestational age (SGA) infants22, studies using birth weight-based registries should be interpreted with caution, because more mature but smaller infants could be included in the registry.
This retrospective cohort study selected and analysed infants born at less than 30 weeks of gestation, from a nationwide registry database of VLBW infants in Korea, to investigate the association between PIH and BPD.
Methods
The Korean Neonatal Network (KNN) is a national prospective registry of VLBW infants (birth weight < 1,500 g) born in the Republic of Korea, covering more than 70% of the overall births of VLBW infants in Korea23. The KNN registry was approved by the institutional review board (IRB) at each participating hospital, and informed consent was obtained from the parents of all infants at enrollment by the NICUs participating in the KNN. All methods were carried out in accordance with the IRB-approved protocol and in compliance with relevant guidelines and regulations. The definitions of the data were guided by the manual of operation of the KNN and the data registered in the KNN database comprises the antenatal and perinatal histories, postnatal morbidities, and clinical outcomes evaluated during the hospital stay using a standardized electronic case-report form. Altogether 3,507 VLBW infants were born and registered with the KNN database from January 2013 to December 2014, and 2,276 infants who were born at less than 30 weeks of gestation were enrolled in the study. Infants with congenital anomalies, those born to mothers with chronic hypertension, infants without BPD data, and infants who died before 36 weeks of post-menstrual age (PMA) were excluded from the study.
PIH was defined as newly diagnosed hypertension in a pregnant woman after 20 weeks of gestation, where systolic blood pressure was ≥140 mmHg and/or diastolic blood pressure was ≥90 mmHg. BPD was defined as the need for supplemental oxygen or positive pressure support at 36 weeks of PMA. This corresponds with moderate or severe BPD, according to the severity-based definition for BPD provided by the National Institute of Health consensus24. Respiratory distress syndrome (RDS) was defined by clinical diagnosis and required surfactant therapy. Intraventricular haemorrhage (IVH) was defined by the Papile criteria, using cranial ultrasonography25. Necrotizing enterocolitis (NEC) was defined according to Bell’s criteria (stage 2 or higher)26. Retinopathy of prematurity (ROP) was defined according to the international classification of ROP27. SGA was defined as birth weight lower than the third percentile for GA, according to Fenton’s growth charts28. The study was approved by the Institutional Review Board of Seoul National University Hospital (1701-024-821).
The Chi-squared test was used for comparing categorical variables and the Student’s two-tailed t-test was used for analysing the continuous variables between groups. Univariate and multivariate logistic regression analyses were used to investigate the association between PIH and BPD, after adjusting for potential confounders. Adjusted odds ratios, with a 95% confidence interval (CI) were obtained, to assess the magnitude of the association between various factors and BPD. Subgroup analysis according to the GA (<27 weeks and 27-29 weeks) was done to figure out whether the effects of PIH on BPD vary between different age groups. Sensitivity analysis was conducted with an extended population including death before PMA 36 weeks using a composite outcome of BPD and death to investigate the association with PIH. Data are presented as the mean ± standard deviation. Statistical analyses were performed with STATA 11.0 (Stata Corp, College Station, Tex., USA).
Results
Of the 3,507 infants registered with the KNN database during the study period, 1,231 infants were born at or more than 30 weeks of gestation, 28 infants were born to mothers with chronic hypertension and 65 infants had a congenital anomaly (Fig. 1). Nine infants without BPD data and 347 infants who died before 36 weeks of PMA were also excluded. Of the remaining 1,827 infants, 203 (11.1%) infants were born to mothers with PIH and 1,624 (88.9%) infants were born to mothers without hypertension.
Flow chart of the study population. Among 3,507 infants registered, 2,276 infants who were born at less than 30 weeks of gestation were enrolled and 1,827 were analysed. BPD: bronchopulmonary dysplasia, GA: gestational age, HTN: hypertension, KNN: Korean Neonatal Network, PIH: pregnancy-induced hypertension, PMA: postmenstrual age.
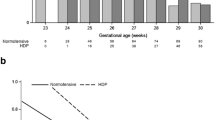
The GA of the PIH group was higher than that of the non-PIH group (27.3 ± 1.8 versus 28.0 ± 1.4 weeks, p < 0.001) (Table 1). Birth weight was lower in the PIH group than that in the non-PIH group (876.4 ± 261.5 versus 1027.4 ± 250.2 g, p < 0.001). Infants who were SGA were more common in the PIH group than the non-PIH group (1.4% vs. 9.9%, p < 0.001). Infants in the PIH group received more prenatal steroid therapy and were mostly delivered through a Cesarean section. On the other hand, multiple births, histologic chorioamnionitis (hCAM), and preterm premature rupture of the membrane were more prevalent in the non-PIH group. Severe IVH (≥grade 3) was significantly lower in the PIH group (10.6% versus 5.4%, p = 0.018) and the duration of total parenteral nutrition (TPN) was significantly longer in the PIH group (33.9 ± 28.6 versus 38.5 ± 28 days, p = 0.031) (Table 2). There were no differences in the duration of invasive ventilation or hospital stay between the non-PIH and PIH groups. The incidence of BPD (41.4% in the non-PIH group versus 44.8% in the PIH group) was not significantly different between the two groups.
Univariate and multivariate logistic regression analyses were performed to evaluate the risk factors for BPD. In the univariate analysis, lower GA at birth, SGA, RDS, male sex, hCAM, and treated patent ductus arteriosus (PDA) were associated with BPD (Table 3). Although PIH was not associated with BPD on the univariate analysis, PIH was associated with BPD (adjusted OR 1.474, 95% CI 1.025–2.121) along with GA, SGA, male sex, hCAM and treated PDA on the multivariate analysis. The subgroup analyses according to GA stratification were performed and multivariate analysis showed that there was an association between PIH and BPD in VLBW infants with 27–29 weeks of gestation (adjusted OR 1.626, 95% CI 1.075–2.460), but not in the other GA groups (Table 4).
Multivariate analyses with a population including infants who died before 36 weeks of PMA were further studied as a sensitivity analysis to evaluate the association of PIH with the composite outcome of BPD or death at 36 weeks of PMA (Table S2). PIH was associated with BPD or death at 36 weeks of PMA (adjusted OR 1.428, 95% CI 1.015–2.008).
Discussion
In this study, PIH was associated with BPD in the VLBW infants, who were born at less than 30 weeks of gestation, after adjusting for other risk factors. Impaired pulmonary vascular growth by altered signalling of angiogenic or antiangiogenic factors derived from mothers with hypertension may play a role in the pathogenesis of BPD29. Although how maternal angiogenic and anti-angiogenic factors influence the development of foetal lungs is not fully understood, elevation in anti-angiogenic factors, such as soluble fms-like tyrosine kinase-1 and soluble endoglin in the placenta and cord blood of a mother with PE might affect angiogenesis in foetal lungs with low levels of VEGF and placental growth factor30,31. Earlier studies from our group also demonstrated that increased soluble endoglin (an antiangiogenic factor) in cord blood was associated with the development of BPD in preterm infants born to mothers with PE32.
However, the results of several studies on the association of PIH or PE with BPD are conflicting. A population-based study analysing 5,753 VLBW infants by Yen et al. reported that foetal exposure to maternal PE was associated with a reduced risk of BPD21. A meta-analysis of 1,268 infants from three Victorian Infant Collaborative Study cohorts showed that PE did not influence the risk of BPD in extremely low-birth weight infants20. Results from these studies should be interpreted with caution due to several reasons. In the study by Yen et al., the study population included VLBW infants and was not defined according to the GA. Therefore, relatively smaller, mature babies were mostly included in the study population, especially in the PE group with a higher prevalence of SGA (73.3%). The protective effect of PE on BPD was shown only in the subgroup with a GA of 31~34 weeks, while the number of mature babies with SGA as a confounder would be higher in the VLBW population.
Studies with a GA-based population have yielded results that are different from earlier studies. An international cohort study comprising international neonatal (iNeo) databases based on GA analysed 28,092 preterm neonates born at 24 to 28 weeks of gestation and reported that the risk for BPD increased in infants born to mothers with hypertensive disorders of pregnancy18. A meta-analysis by Razak et al. reported that PIH was associated with BPD in the subpopulation of neonates born at <29 weeks of gestation19.
PIH is associated with babies that are small for the GA at birth33,34. The baby’s size and GA both have a significantly inverse relationship with BPD35. These associations were demonstrated in the present study as well. Therefore, the “size for gestational age” should be adjusted or GA-based population determination should be considered, while analysing the association between PIH and BPD, similar to the iNeo study or the study by Razak et al.18,19. To elucidate the association between BPD and PIH amidst these confounders, infants with a GA of 30 weeks or more were excluded from the study population, where SGA babies would be preferentially included in the weight-based registration. Sensitivity analysis among the population containing those who died before 36 weeks of PMA showed that composite outcome of BPD or death was also associated with PIH. Among the 347 infants who died before 36 weeks of PMA, cardiorespiratory failure was a leading cause of death, but there was no significant difference in the proportion of cardiorespiratory causes of death between the PIH and non-PIH groups (Table S3).
In the subgroup analysis, more mature infants with a GA 27~29 weeks were influenced by PIH in the development of BPD. A higher incidence of BPD in the subgroup with a GA < 27 weeks compared to those with a GA 27~29 weeks (60.4~62.8% vs. 29.2~40%, respectively) might reflect the vulnerability of the less mature lungs, and the alveolar-capillary structure might be arrested in the earlier phase of development in this population5. Moreover, immature infants experience various kinds of stress during the neonatal period, such as oxygen stress, inflammation, and hypoxia. Since BPD is an entity with a multifactorial pathogenesis5, there could be many factors that contribute to the development of BPD other than imbalanced vascular growth influenced by the maternal side. Differences in the association of maternal hypertensive disorder among GA subgroups were also well demonstrated in the large cohort study from Israel Neonatal Network36.
In conclusion, PIH was associated with BPD in VLBW infants, who were born before 30 weeks of gestation. The utilization of a nationwide registration database of VLBW infants in Korea was a strength of this study. This study’s results are consistent with the current concept that BPD is an early manifestation of pulmonary vascular disease.
Data availability
According to the Korean Neonatal Network (KNN) Publication Ethics Policy, all registered data is confidential and is only available to researchers who have permission of access for the research activities. The dataset generated and analysed are not publicly available, but are available from the corresponding author on reasonable request.
References
Bancalari, E. & del Moral, T. Bronchopulmonary dysplasia and surfactant. Biol Neonate 80 (Suppl 1), 7–13, 47170 (2001).
Chawla, S. et al. Association of Neurodevelopmental Outcomes and Neonatal Morbidities of Extremely Premature Infants With Differential Exposure to Antenatal Steroids. JAMA Pediatr. 170, 1164–1172, https://doi.org/10.1001/jamapediatrics.2016.1936 (2016).
Stoll, B. J. et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA 314, 1039–1051, https://doi.org/10.1001/jama.2015.10244 (2015).
Christensen, R. D. Advances and controversies in neonatal ICU platelet transfusion practice. Adv. Pediatr. 55, 255–269 (2008).
Coalson, J. J. Pathology of new bronchopulmonary dysplasia. Semin. Neonatol. 8, 73–81 (2003).
Hilgendorff, A. et al. Pulmonary hypertension associated with acute or chronic lung diseases in the preterm and term neonate and infant. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102(Suppl 2), ii49–56, https://doi.org/10.1136/heartjnl-2015-308591 (2016).
von Dadelszen, P. et al. Maternal hypertension and neonatal outcome among small for gestational age infants. Obstet. Gynecol. 106, 335–339, https://doi.org/10.1097/01.AOG.0000171121.31564.14 (2005).
Zhang, J., Meikle, S. & Trumble, A. Severe maternal morbidity associated with hypertensive disorders in pregnancy in the United States. Hypertens. Pregnancy 22, 203–212, https://doi.org/10.1081/PRG-120021066 (2003).
Savitz, D. A., Danilack, V. A., Engel, S. M., Elston, B. & Lipkind, H. S. Descriptive epidemiology of chronic hypertension, gestational hypertension, and preeclampsia in New York State, 1995–2004. Matern. Child. Health J. 18, 829–838, https://doi.org/10.1007/s10995-013-1307-9 (2014).
Schneider, S. et al. Risk groups and maternal-neonatal complications of preeclampsia–current results from the national German Perinatal Quality Registry. J. Perinat. Med. 39, 257–265, https://doi.org/10.1515/JPM.2011.010 (2011).
Roberts, J. M. & Hubel, C. A. The two stage model of preeclampsia: variations on the theme. Placenta 30(Suppl A), S32–37, https://doi.org/10.1016/j.placenta.2008.11.009 (2009).
Burton, G. J., Charnock-Jones, D. S. & Jauniaux, E. Regulation of vascular growth and function in the human placenta. Reproduction 138, 895–902, https://doi.org/10.1530/REP-09-0092 (2009).
Conti, E. et al. Growth factors in preeclampsia: a vascular disease model. A failed vasodilation and angiogenic challenge from pregnancy onwards? Cytokine Growth Factor. Rev. 24, 411–425, https://doi.org/10.1016/j.cytogfr.2013.05.008 (2013).
Stubert, J. et al. Prediction of preeclampsia and induced delivery at <34 weeks gestation by sFLT-1 and PlGF in patients with abnormal midtrimester uterine Doppler velocimetry: a prospective cohort analysis. BMC Pregnancy Childbirth 14, 292, https://doi.org/10.1186/1471-2393-14-292 (2014).
Abman, S. H. Impaired vascular endothelial growth factor signaling in the pathogenesis of neonatal pulmonary vascular disease. Adv. Exp. Med. Biol. 661, 323–335, https://doi.org/10.1007/978-1-60761-500-2_21 (2010).
Tsao, P. N. et al. Placenta growth factor elevation in the cord blood of premature neonates predicts poor pulmonary outcome. Pediatrics 113, 1348–1351 (2004).
Ozkan, H., Cetinkaya, M. & Koksal, N. Increased incidence of bronchopulmonary dysplasia in preterm infants exposed to preeclampsia. J. Matern. Fetal Neonatal Med. 25, 2681–2685, https://doi.org/10.3109/14767058.2012.708371 (2012).
Gemmell, L. et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J. Perinatol. 36, 1067–1072, https://doi.org/10.1038/jp.2016.133 (2016).
Razak, A. et al. Pregnancy-induced hypertension and neonatal outcomes: a systematic review and meta-analysis. J. perinatology: Off. J. Calif. Perinat. Assoc. 38, 46–53, https://doi.org/10.1038/jp.2017.162 (2018).
O’Shea, J. E., Davis, P. G., Doyle, L. W. & Victorian Infant Collaborative Study, G. Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants. Pediatr. Res. 71, 210–214, https://doi.org/10.1038/pr.2011.27 (2012).
Yen, T. A. et al. Preeclampsia and the risk of bronchopulmonary dysplasia in VLBW infants: a population based study. PLoS One 8, e75168, https://doi.org/10.1371/journal.pone.0075168 (2013).
Allen, V. M. et al. The effect of hypertensive disorders in pregnancy on small for gestational age and stillbirth: a population based study. BMC Pregnancy Childbirth 4, 17, https://doi.org/10.1186/1471-2393-4-17 (2004).
Chang, Y. S., Park, H. Y. & Park, W. S. The Korean Neonatal Network: An Overview. J. Korean Med. Sci. 30, S3–S11, https://doi.org/10.3346/jkms.2015.30.S1.S3 (2015).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729, https://doi.org/10.1164/ajrccm.163.7.2011060 (2001).
Papile, L. A., Munsick-Bruno, G. & Schaefer, A. Relationship of cerebral intraventricular hemorrhage and early childhood neurologic handicaps. J. Pediatr. 103, 273–277 (1983).
Bell, M. J. et al. Neonatal Necrotizing Enterocolitis - Therapeutic Decisions Based Upon Clinical Staging. Ann. Surg. 187, 1–7, https://doi.org/10.1097/00000658-197801000-00001 (1978).
Garner, A. An International Classification of Retinopathy of Prematurity. Arch. Ophthalmol-Chic 102, 1130–1134 (1984).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC pediatrics 13, 59, https://doi.org/10.1186/1471-2431-13-59 (2013).
Stenmark, K. R. & Abman, S. H. Lung vascular development: implications for the pathogenesis of bronchopulmonary dysplasia. Annu. Rev. Physiol. 67, 623–661, https://doi.org/10.1146/annurev.physiol.67.040403.102229 (2005).
Tsao, P. N. et al. Excess soluble fms-like tyrosine kinase 1 and low platelet counts in premature neonates of preeclamptic mothers. Pediatrics 116, 468–472, https://doi.org/10.1542/peds.2004-2240 (2005).
Lassus, P. et al. Vascular endothelial growth factor in human preterm lung. Am. J. Respir. Crit. Care Med. 159, 1429–1433, https://doi.org/10.1164/ajrccm.159.5.9806073 (1999).
Kim, D. H. et al. Association of increased cord blood soluble endoglin with the development of bronchopulmonary dysplasia in preterm infants with maternal preeclampsia. Pregnancy Hypertens. 13, 148–153, https://doi.org/10.1016/j.preghy.2018.06.002 (2018).
Xiong, X. et al. Impact of pregnancy-induced hypertension on fetal growth. Am. J. Obstet. Gynecol. 180, 207–213 (1999).
Srinivas, S. K. et al. Rethinking IUGR in preeclampsia: dependent or independent of maternal hypertension? J. Perinatol. 29, 680–684, https://doi.org/10.1038/jp.2009.83 (2009).
Bose, C. et al. Fetal growth restriction and chronic lung disease among infants born before the 28th week of gestation. Pediatrics 124, e450–458, https://doi.org/10.1542/peds.2008-3249 (2009).
Klinger, G. et al. Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am. J. Obstet. Gynecol. 208, 115 e111–119, https://doi.org/10.1016/j.ajog.2012.11.026 (2013).
Acknowledgements
This research was supported by a fund (2016-ER6307-02#) by Research of Korea Centers for Disease Control and Prevention and by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2017R1D1A1B03036383). Portions of this study were presented at 7th congress of the European Academy of Pediatric Societies (EAPS2018), October 30-November 3, 2018, Paris, France.
Author information
Authors and Affiliations
Contributions
Concept and design: Seung Hyun Shin, Seung Han Shin, Data acquisition: Seung Hyun Shin, Seh Hyun Kim, Yoo-Jin Kim, Hannah Cho, Monitoring during the study: Ee-Kyung Kim, Han-Suk Kim, Data analysis and interpretation: Seung Hyun Shin, Seung Han Shin, Drafting the article: Seung Hyun Shin, Article revision for important intellectual content: Ee-Kyung Kim, Han-Suk Kim, Review and final approval of manuscript revisions: Seung Hyun Shin, Seung Han Shin.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shin, S.H., Shin, S.H., Kim, S.H. et al. The Association of Pregnancy-induced Hypertension with Bronchopulmonary Dysplasia – A Retrospective Study Based on the Korean Neonatal Network database. Sci Rep 10, 5600 (2020). https://doi.org/10.1038/s41598-020-62595-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62595-7
This article is cited by
-
Maternal hypertensive disorders and survival without major morbidities among extremely low gestation newborns
Journal of Perinatology (2023)
-
Lung recruitment improves the efficacy of intubation-surfactant-extubation treatment for respiratory distress syndrome in preterm neonates, a randomized controlled trial
BMC Pediatrics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.