Abstract
Objective
Nasal Intermittent Positive Pressure Ventilation (NIPPV) is an effective therapy for infants in respiratory distress. We here report the safety of a novel, low-cost, non-electric bubble NIPPV device in comparison with bubble NCPAP.
Study design
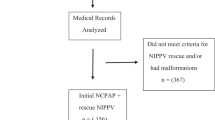
At Paramitha Children’s Hospital (Hyderabad, India), preterm (n = 60) neonates with moderate respiratory distress were pragmatically allocated to bubble NCPAP (5–8 cm H2O) or bubble NIPPV (Phigh 8–12 cm H2O/Plow 5–8 cm H2O) based on staff and equipment availability. Primary outcomes to assess safety included clinically relevant pneumothorax, nasal septal necrosis, or abdominal distention.
Results
One patient in each arm developed minor nasal septal injury (grade 3 on NCPAP, grade 2 on NIPPV); no patients in either arm developed a clinically significant pneumothorax or abdominal distention.
Conclusion
The similar rates of nasal septal injury, pneumothorax and abdominal distention suggest that bubble NIPPV has a similar safety profile as bubble NCPAP for preterm infants in respiratory distress.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
References
Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? The Lancet. 2005;365:891–900.
Tochie JN, Sibetcheu AT, Arrey-Ebot PE, Choukem SP. Global, regional and national trends in the burden of neonatal respiratory failure and essentials of its diagnosis and management from 1992 to 2022: a scoping review. Eur J Pediatr. 2023;17:1–42.
MacDonald MG, Ramasethu J, Rais-Bahrami K. Atlas of procedures in neonatology. Lippincott Williams & Wilkins; 2012.
Lee KS, Dunn MS, Fenwick M, Shennan AT. A comparison of underwater bubble continuous positive airway pressure with ventilator-derived continuous positive airway pressure in premature neonates ready for extubation. Neonatology. 1998;73:69–75.
Martin S, Duke T, Davis P. Efficacy and safety of bubble CPAP in neonatal care in low and middle income countries: a systematic review. Arch Disease Childhood-Fetal Neonatal Ed. 2014;99:F495–504.
Bhandari V. The potential of non-invasive ventilation to decrease BPD. Semin Perinatol. 2013;37(2):108–14.
Bhandari V. Nasal intermittent positive pressure ventilation in the newborn: review of literature and evidence-based guidelines. J Perinatol. 2010;30:505–12.
Lemyre B, Deguise MO, Benson P, Kirpalani H, Ekhaguere OA, Davis PG. Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev. 2023;7:CD005384.
Lemyre B, Deguise MO, Benson P, Kirpalani H, De Paoli AG, Davis PG. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. 2023;7:CD003212.
John SC, Barnett JD, Habben ND, Le HT, Cheng E, John SP, et al. Development and testing of a bubble bi-level positive airway pressure system. Respir Care. 2017;62:1131–6.
John SC, John AV, Moss AW, Gustafson PA, Fernando-Silva L, John SP. Bench testing of a bubble noninvasive ventilation device in an infant lung simulator. Respir Care. 2020;65:1339–45.
John SC, Mohammed A, Church JT, John AV, Perkins EM, McLeod JS, et al. Bubble bilevel ventilation facilitates gas exchange in anesthetized rabbits. Pediatric Res. 2021;89:622–7.
John SC, Adhikari BR, John AV, Cheng EO, Weiner GM, John SP. Feasibility of bubble non-invasive positive pressure ventilation, a first-in-human study. J Trop Pediatr. 2022;68:fmac095.
Bashir T, Murki S, Kiran S, Reddy VK, Oleti TP. ‘Nasal mask’ in comparison with ‘nasal prongs’ or ‘rotation of nasal mask with nasal prongs’ reduce the incidence of nasal injury in preterm neonates supported on nasal continuous positive airway pressure (nCPAP): a randomized controlled trial. PLoS ONE. 2019;14:e0211476.
Bhandari V, Black R, Gandhi B, Hogue S, Kakkilaya V, Mikhael M, et al. RDS-NExT workshop: consensus statements for the use of surfactant in preterm neonates with RDS. J Perinatol. 2023;15:1–9.
DiBlasi RM. Neonatal noninvasive ventilation techniques: do we really need to intubate? Respir Care. 2011;56:1273–97.
Ho JJ, Subramaniam P, Davis PG. Continuous positive airway pressure (CPAP) for respiratory distress in preterm infants. Cochrane Database Syst Rev. 2020;10:CD002271.
Lemyre B, Davis PG, De Paoli AG, Cochrane Neonatal Group. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for apnea of prematurity. Cochrane Database Syst Rev. 1996;2010.
Dumpa V, Katz K, Northrup V, Bhandari V. SNIPPV vs NIPPV: does synchronization matter? J Perinatol. 2012;32:438–42.
Sahni M, Bhandari V. Invasive and non-invasive ventilatory strategies for early and evolving bronchopulmonary dysplasia. Semin Perinatol. 2023;47:151815.
Cresi F, Chiale F, Maggiora E, Borgione SM, Ferroglio M, Runfola F, et al. Short-term effects of synchronized vs. non-synchronized NIPPV in preterm infants: study protocol for an unmasked randomized crossover trial. Trials. 2021;22:1–9.
Acknowledgements
This data has previously been presented at PRESS (Department of Pediatrics, University of Minnesota).
Funding
Research reported in this publication was supported by the Thrasher Foundation and by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1-TR002494.
Author information
Authors and Affiliations
Contributions
Study Conception and Design (SJ, MG, VB, TS, SM), Data analysis (SJ, MG, MM, AB, PR, VB, TS, SM), Drafting of manuscript and approval of final manuscript (SJ, MG, MM, AB, PR, VB, TS, SM).
Corresponding author
Ethics declarations
Competing interests
SCJ is a co-inventor of bubble NIPPV technology and co-founder of AIM Tech Health.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
John, S.C., Garg, M., Muttineni, M. et al. Safety of bubble nasal intermittent positive pressure ventilation (NIPPV) versus bubble nasal continuous positive airway pressure (NCPAP) in preterm infants with respiratory distress. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01904-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01904-8