Abstract
Objective
Evaluate whether nasal intermittent positive-pressure ventilation (NIPPV) as rescue therapy after initial nasal continuous positive airway (NCPAP) failure reduces need for invasive mechanical ventilation (IMV) in infants with respiratory distress syndrome (RDS).
Design
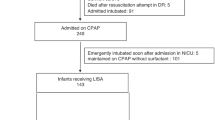
Retrospective cohort involving 156 preterm infants who failed initial NCPAP and were then submitted to NIPPV rescue therapy and classified into NIPPV success or failure, according to need for IMV.
Result
Of all infants included, 85 (54.5%) were successfully rescued with NIPPV while 71 (45.5%) failed. The NIPPV success group had significantly lower rates of bronchopulmonary dysplasia, peri/intraventricular hemorrhage, patent ductus arteriosus and greater survival without morbidities (all p ≤ 0.01). Infants who failed NIPPV had earlier initial NCPAP failure (p = 0.09). In final logistic regression model, birthweight ≤1000 g and need for surfactant remained significant factors for NIPPV failure.
Conclusion
NIPPV rescue therapy reduced the need for IMV in infants that failed NCPAP and was associated with better outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The authors acknowledge that the data and materials are available to referees at submission and to readers promptly upon request.
References
Owen LS, Manley BJ, Davis PG, Doyle LW. The evolution of modern respiratory care for preterm infants. Lancet [Internet]. 2017;389:1649–59. https://doi.org/10.1016/S0140-6736(17)30312-4.
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatrics. 2017;171:306.
Jensen EA, Schmidt B. Epidemiology of bronchopulmonary dysplasia. Birth Defects Res Part A - Clin Mol Teratol. 2014;100:145–57.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr [Internet]. 2018;197:300–8. https://doi.org/10.1016/j.jpeds.2018.01.043.
Dumpa V, Bhandari V. Non-invasive ventilatory strategies to decrease bronchopulmonary dysplasia—where are we in 2021? Children. 2021;8:1–11.
Fischer HS, Bührer C. Avoiding endotracheal ventilation to prevent bronchopulmonary dysplasia: a meta-analysis. Pediatrics. 2013;132:e1351–60.
Behnke J, Lemyre B, Czernik C, Zimmer KP, Ehrhardt H, Waitz M. Non-invasive ventilation in neonatology. Deutsches Aerzteblatt Online. 2019;116:177–83.
Alexiou S, Panitch HB. Physiology of non-invasive respiratory support. Semin Fetal Neonatal Med [Internet]. 2016;21:174–80. https://doi.org/10.1016/j.siny.2016.02.007.
Owen LS, Manley BJ. Nasal intermittent positive pressure ventilation in preterm infants: equipment, evidence, and synchronization. Semin Fetal Neonatal Med [Internet]. 2016;21:146–53. https://doi.org/10.1016/j.siny.2016.01.003.
Lemyre B, Laughon M, Bose C, Davis PG. Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev. 2016;12:CD005384.
Lemyre B, Davis PG, de Paoli AG, Kirpalani H. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Vol. 2017, Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd; 2017.
Ramaswamy VV, Bandyopadhyay T, Nanda D, Bandiya P, More K, Oommen VI, et al. Efficacy of noninvasive respiratory support modes as postextubation respiratory support in preterm neonates: a systematic review and network meta-analysis. Pediatr Pulmonol. 2020;55:2924–39.
Jensen EA, Chaudhary A, Bhutta ZA, Kirpalani H. Non-invasive respiratory support for infants in low- and middle-income countries. Semin Fetal Neonatal Med. 2016;21:181–8.
Dargaville PA, Aiyappan A, de Paoli AG, Dalton RGB, Kuschel CA, Kamlin CO. et al. Continuous positive airway pressure failure in preterm infants: incidence, predictors and consequences. Neonatology. 2013;104:8–14.
de Jaegere AP, van der Lee JH, Canté C, van Kaam AH. Early prediction of nasal continuous positive airway pressure failure in preterm infants less than 30 weeks gestation. Acta Paediatrica Int J Paediatr. 2012;101:374–9.
Ramos-Navarro C, Sanchez-Luna M, Sanz-López E, Maderuelo-Rodriguez E, Zamora-Flores E. Effectiveness of synchronized noninvasive ventilation to prevent intubation in preterm infants. Am J Perinatol Rep. 2016;06:e264–71.
Badiee Z, Nekooie B, Mohammadizadeh M. Noninvasive positive pressure ventilation or conventional mechanical ventilation for neonatal continuous positive airway pressure failure. Int J Prev Med [Internet]. 2014;5. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4258678/?report=printable
Bhandari V. Nasal intermittent positive pressure ventilation in the newborn: review of literature and evidence-based guidelines. J Perinatol [Internet]. 2010;30:505–12. https://doi.org/10.1038/jp.2009.165.
Meneses J, Bhandari V, Guilherme Alves J, Herrmann D. Noninvasive ventilation for respiratory distress syndrome: a randomized controlled trial. Pediatrics. 2011;127:300–7.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–24.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatrics. 2001;138:92–100.
Quinn GE. The international classification of retinopathy of prematurity revisited: an international committee for the classification of retinopathy of prematurity. Arch Ophthalmol. 2005;123:991–9.
Papile L, Burnstein J, Burnstein R, Koffelertt. Incidence and evolution of subependyma and intraventricular hemorrhage: a study of infants with birthweight less than 1500g. J Pediatr. 1978;92:529–33.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am [Internet]. 1986;33:179–201. https://doi.org/10.1016/S0031-3955(16)34975-6.
Shi Y, Muniraman H, Biniwale M, Ramanathan R. A review on non-invasive respiratory support for management of respiratory distress in extremely preterm infants. Front Pediatrics. 2020;8:1–17.
Soll RF, Barkhuff W. Noninvasive ventilation in the age of surfactant administration. Clin Perinatol. 2019;46:493–516.
Lemyre B, Davis PG, de Paoli AG. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for apnea of prematurity. Cochrane Database Syst Rev. 2002; CD002272.
Gulczyńska E, Szczapa T, Hożejowski R, Borszewska-Kornacka MK, Rutkowska M. Fraction of inspired oxygen as a predictor of CPAP failure in preterm infants with respiratory distress syndrome: a prospective multicenter study. Neonatology. 2019;116:171–8.
Rüegger CM, Owen LS, Davis PG. Nasal intermittent positive pressure ventilation for neonatal respiratory distress syndrome. Clin Perinatol [Internet]. 2021;48:725–44. https://doi.org/10.1016/j.clp.2021.07.004.
Ekhaguere O, Patel S, Kirpalani H. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure before and after invasive ventilatory support. Clin Perinatol. 2019;46:517–36.
McGillick EV, Orgeig S, Williams MT, Morrison JL. Risk of respiratory distress syndrome and efficacy of glucocorticoids: are they the same in the normally grown and growth-restricted infant? Reprod Sci. 2016;23:1459–72.
Malhotra A, Sasi A, Miller SL, Jenkin G, Polglase GR. The efficacy of surfactant replacement therapy in the growth-restricted preterm infant: What is the evidence? Front Pediatrics. 2014;2:1–5.
Harsha SS, Archana BR. SNAPPE-II (score for neonatal acute physiology with perinatal extension-II) in predicting mortality and morbidity in NICU. J Clin Diagnostic Res. 2015;9:SC10–2.
Flannery DD, Edwards EM, Puopolo KM, Horbar JD. Early-onset sepsis among very preterm infants. Pediatr. 2021;148:e2021052456.
Moretti C, Gizzi C. Synchronized nasal intermittent positive pressure ventilation. Clin Perinatol. 2021;48:745–59.
Waitz M, Mense L, Kirpalani H, Lemyre B. Nasal intermittent positive pressure ventilation for preterm neonates: synchronized or not? Clin Perinatol [Internet]. 2016;43:799–816. https://doi.org/10.1016/j.clp.2016.07.013.
Dumpa V, Katz K, Northrup V, Bhandari V. SNIPPV vs NIPPV: does synchronization matter. J Perinatol [Internet]. 2012;32:438–42. https://doi.org/10.1038/jp.2011.117.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, te Pas A, et al. European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology. 2019;115:432–50.
Sardesai S, Biniwale M, Wertheimer F, Garingo A, Ramanathan R. Evolution of surfactant therapy for respiratory distress syndrome: past, present, and future. Pediatr Res. 2017;81:240–8.
Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. In: JAMA. 2016;316:611–24.
Chan KYY, Miller SL, Schmölzer GM, Stojanovska V, Polglase GR. Respiratory support of the preterm neonate: lessons about ventilation-induced brain injury from large animal models. Front Neurol. 2020;11:1–14.
Ramaswamy VV, More K, Roehr CC, Bandiya P, Nangia S. Efficacy of noninvasive respiratory support modes for primary respiratory support in preterm neonates with respiratory distress syndrome: systematic review and network meta-analysis. Pediatr Pulmonol. 2020;55:2940–63.
Author information
Authors and Affiliations
Contributions
CI conceptualized the study, participated in the study design, data collection and data analysis, and wrote and revised the paper. JM conceptualized the study, participated in the study design and data analysis, and wrote and revised the paper. JA participated in the study design, data analysis and revision. JC participated in the study design and data collection. EA participated in the data analysis. VB conceptualized the study, participated in the study design, and revised the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The research complied with the ethical principles established in the Declaration of Helsinki and was submitted to the ethics committee of the Instituto de Medicina Integral Professor Fernando Figueira, IMIP, Recife, Brazil. CAAE: 27431919.0.0000.5201.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishigami, A.C., Meneses, J., Alves, J.G. et al. Nasal intermittent positive pressure ventilation as a rescue therapy after nasal continuous positive airway pressure failure in infants with respiratory distress syndrome. J Perinatol 43, 311–316 (2023). https://doi.org/10.1038/s41372-023-01600-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01600-z