Abstract
Objective
To examine the association between maternal hypertension during pregnancy and neurodevelopmental impairment (NDI) at 24 months post-menstrual age in extremely preterm infants.
Study design
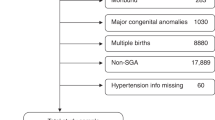
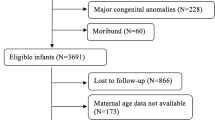
Using data from two tertiary neonatal units (2011–2017) for infants born at 23 + 0 to 28 + 6 weeks, we investigated outcomes of NDI related to maternal hypertension and small-for-gestational-age (SGA) status.
Results
Of 1019 pre-term infants, 647 had complete data and were included in the analysis. Ninety-six (15%) had maternal hypertension exposure; 25 (4%) were also SGA. Infants with maternal hypertension showed a higher odds of any NDI (aOR: 2.29, 95% CI = 1.36–3.87) and significant NDI (aOR: 2.01, 95% CI = 1.02–3.95). The combination of hypertension and SGA further elevated this risk (aOR for any NDI: 4.88, 95% CI = 1.80–13.22; significant NDI: 6.91, 95% CI = 2.50–19.12).
Conclusion
Maternal hypertension during pregnancy elevates the risk of NDI in extremely preterm infants, more so when combined with SGA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Derived data generated will be shared on reasonable request to the corresponding author.
References
Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller A-B, et al. Born Too Soon: The global epidemiology of 15 million preterm births. Reprod Health. 2013;10:S2.
de Paula Fiod Costa H, de Paula Fiod Costa E. Neonatal Complications of Prematurity. Perinatology: Evidence-Based Best Practices in Perinatal Medicine. 2022;1133–50.
The Canadian Neonatal Network. Canadian Neonatal Network Annual Report 2020. The Canadian Neonatal Network. 2020. Available from: http://www.canadianneonatalnetwork.org/portal/CNNHome.aspx.
Shafey A, Bashir RA, Shah P, Synnes A, Yang J, Kelly EN, et al. Outcomes and resource usage of infants born at ≤ 25 weeks gestation in Canada. Paediatr Child Health. 2020;25:207–15.
Serenius F, Källén K, Blennow M, Ewald U, Fellman V, Holmström G, et al. Neurodevelopmental Outcome in Extremely Preterm Infants at 2.5 Years After Active Perinatal Care in Sweden. JAMA 2013;309:1810.
Synnes A, Anson S, Baum J, Usher L. Incidence and pattern of hearing impairment in children with ≤ 800 g birthweight in British Columbia, Canada. Acta Paediatr. 2011;101:e48–54.
Ricci MF, Shah PS, Moddemann D, Alvaro R, Ng E, Lee SK, et al. Neurodevelopmental Outcomes of Infants at <29 Weeks of Gestation Born in Canada Between 2009 and 2016. J Pediatr. 2022;247:60–66.e1.
Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-Hospital Variation in Treatment and Outcomes in Extremely Preterm Infants. N. Engl J Med. 2015;372:1801–11.
Aucott SW, Donohue PK, Northington FJ. Increased Morbidity in Severe Early Intrauterine Growth Restriction. J Perinatol. 2004;24:435–40.
Bardin C, Zelkowitz P, Papageorgiou A. Outcome of small-for-gestational age and appropriate-for-gestational age infants born before 27 weeks of gestation. Pediatrics 1997;100:E4.
Esih K, Trunk T, Osredkar D, Verdenik I, Neubauer D, Troha Gergeli A, et al. The impact of birthweight on the development of cerebral palsy: A population-based matched case-control study. Early Hum Dev. 2022;165:105533.
Zhang S, Wang L, Leng J, Liu H, Li W, Zhang T, et al. Hypertensive disorders of pregnancy in women with gestational diabetes mellitus on overweight status of their children. J Hum Hypertens 2017;31:731–6.
Butalia S, Audibert F, Côté A-M, Firoz T, Logan AG, Magee LA, et al. Hypertension Canada’s 2018 Guidelines for the Management of Hypertension in Pregnancy. Can J Cardiol. 2018;34:526–31.
Magley M, Hinson MR. Eclampsia. Treasure Island (FL): StatPearls Publishing; 2021. p. 2021.
Ushida T, Kotani T, Kinoshita F, Imai K, Nakano-Kobayashi T, Nakamura N, et al. Maternal low birth weight and hypertensive disorders of pregnancy. Pregnancy Hypertens. 2021;23:5–10.
Zheng J-S, Liu H, Ong KK, Huang T, Guan Y, Huang Y, et al. Maternal Blood Pressure Rise During Pregnancy and Offspring Obesity Risk at 4 to 7 Years Old: The Jiaxing Birth Cohort. The. J Clin Endocrinol Metab. 2017;102:4315–22.
Nomura Y, John RM, Janssen AB, Davey C, Finik J, Buthmann J, et al. Neurodevelopmental consequences in offspring of mothers with preeclampsia during pregnancy: underlying biological mechanism via imprinting genes. Arch Gynecol Obstet. 2017;295:1319–29.
Ornoy A, Ratzon N, Greenbaum C, Wolf A, Dulitzky M. School-age children born to diabetic mothers and to mothers with gestational diabetes exhibit a high rate of inattention and fine and gross motor impairment. J Pediatr Endocrinol Metab. 2001;14:681–9.
Biagas KV, Hinton VJ, Hasbani NR, Luckett PM, Wypij D, Nadkarni VM, et al. Long-Term Neurobehavioral and Quality of Life Outcomes of Critically Ill Children after Glycemic Control. J Pediatr. 2020;218:57–63.e5.
Scime NV, Hetherington E, Tomfohr-Madsen L, Nettel-Aguirre A, Chaput KH, Tough SC. Hypertensive disorders in pregnancy and child development at 36 months in the All Our Families prospective cohort study. PLOS ONE. 2021;16:e0260590.
Rees S, Harding R, Walker D. An adverse intrauterine environment: implications for injury and altered development of the brain. Int J Dev Neurosci. 2008;26:3–11.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med. 2007;4:e296.
The Canadian Neonatal Network; CNN Publications. 2022 Abstractor’s manual: The Canadian Neonatal Network; (updated February 1, 2022). CNN v.3.5.2. Available from: https://www.canadianneonatalnetwork.org/portal/Portals/0/CNN%20Manuals/CNN%20Manual_20220201.pdf.
CHU SAINTE-JUSTINE-Mother and child university hospital center. 2022. Available from: https://www.chusj.org/en/soins-services/N/Neonatalogie.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–f4.
Haslam MD, Lisonkova S, Creighton D, Church P, Yang J, Shah PS, et al. Severe Neurodevelopmental Impairment in Neonates Born Preterm: Impact of Varying Definitions in a Canadian Cohort. J Pediatr. 2018;197:75–81.e4.
Amer R, Moddemann D, Seshia M, Alvaro R, Synnes A, Lee K-S, et al. Neurodevelopmental Outcomes of Infants Born at <29 Weeks of Gestation Admitted to Canadian Neonatal Intensive Care Units Based on Location of Birth. The. J Pediatr. 2018;196:31–7.e1.
Synnes A, Luu T, Moddemann D, Church P, Lee D, Vincer M, et al. 91: The Canadian Neonatal Follow-Up Network. Paediatr Child Health. 2014;19:e68-e.
Sala ME, Romero MF, Romero A, Fasano MV, Varea AM, Carrera P, et al. Neurodevelopmental assessment of infants born to mothers with hypertensive disorder of pregnancy at six months of age. J Dev Origins Health Dis. 2022;13:197–203.
Albers CA, Grieve AJ, Bayley N. Bayley Scales of Infant and Toddler Development– Third Edition. San Antonio, TX: Harcourt Assessment. J Psychoeducational Assess. 2007;25:180–90.
Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a model of gross motor function for children with cerebral palsy. Phys Ther. 2000;80:974–85.
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A New and Improved Population-Based Canadian Reference for Birth Weight for Gestational Age. Pediatrics 2001;108:e35-e.
Bernardes TP, Mol BW, Ravelli ACJ, Van Den Berg P, Boezen HM, Groen H. Early and late onset pre-eclampsia and small for gestational age risk in subsequent pregnancies. PLOS ONE. 2020;15:e0230483.
Morin J, Luu TM, Superstein R, Ospina LH, Lefebvre F, Simard MN, et al. Neurodevelopmental Outcomes Following Bevacizumab Injections for Retinopathy of Prematurity. Pediatrics. 2016;137:4.
Que J, Van Oerle R, Albersheim S, Panczuk J, Piper H. The effect of daily probiotics on the incidence and severity of necrotizing enterocolitis in infants with very low birth weight. Can J Surg. 2021;64:E644–E9.
The Canadian Neonatal Network. Postnatal use of steroids for treatment of Chronic Lung Disease in less than 29 weeks. Annual Report by the Canadian Neonatal Network. CNN; 2019. Page 145.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Jaworski M, Janvier A, Bourque CJ, Mai-Vo T-A, Pearce R, Synnes AR, et al. Parental perspective on important health outcomes of extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2022;107:495–500.
Chen Z, Li R, Liu H, Duan J, Yao C, Yang R, et al. Impact of maternal hypertensive disorders on offspring’s neurodevelopment: a longitudinal prospective cohort study in China. Pediatr Res. 2020;88:668–75.
Noda M, Yoshida S, Mishina H, Matsubayashi K, Kawakami K. Association between maternal hypertensive disorders of pregnancy and child neurodevelopment at 3 years of age: a retrospective cohort study. J Dev Orig Health Dis. 2021;12:428–35.
Ilekis JV, Tsilou E, Fisher S, Abrahams VM, Soares MJ, Cross JC, et al. Placental origins of adverse pregnancy outcomes: potential molecular targets: an Executive Workshop Summary of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Am J Obstet Gynecol 2016;215:S1–46.
Voto LS, Zeitune MG. Preeclampsia. Perinatology: Evidence-Based Best Practices in Perinatal Medicine, 707–46.
Burd I, Balakrishnan B, Kannan S. Models of Fetal Brain Injury, Intrauterine Inflammation, and Preterm Birth. Am J Reprod Immunol. 2012;67:287–94.
Walker CK, Krakowiak P, Baker A, Hansen RL, Ozonoff S. Hertz-Picciotto I. Preeclampsia, Placental Insufficiency, and Autism Spectrum Disorder or Developmental Delay. JAMA Pediatrics. 2015;169:154.
Brown AS, Sourander A, Hinkka-Yli-Salomäki S, McKeague IW, Sundvall J, Surcel HM. Elevated maternal C-reactive protein and autism in a national birth cohort. Mol Psychiatry. 2014;19:259–64.
Rätsep MT, Hickman AF, Maser B, Pudwell J, Smith GN, Brien D, et al. Impact of preeclampsia on cognitive function in the offspring. Behav Brain Res. 2016;302:175–81.
Strand KM, Heimstad R, Iversen AC, Austgulen R, Lydersen S, Andersen GL, et al. Mediators of the association between pre-eclampsia and cerebral palsy: population based cohort study. BMJ 2013;347:f4089-f.
Kronenberg ME, Raz S, Sander CJ. Neurodevelopmental outcome in children born to mothers with hypertension in pregnancy: the significance of suboptimal intrauterine growth. Dev Med Child Neurol 2006;48:200–6.
Many A, Fattal A, Leitner Y, Kupferminc MJ, Harel S, Jaffa A. Neurodevelopmental and cognitive assessment of children born growth restricted to mothers with and without preeclampsia. Hypertens Pregnancy. 2003;22:25–9.
Padilla N, Falcón C, Sanz-Cortés M, Figueras F, Bargallo N, Crispi F, et al. Differential effects of intrauterine growth restriction on brain structure and development in preterm infants: a magnetic resonance imaging study. Brain Res. 2011;1382:98–108.
Matić M, Inati V, Abdel-Latif ME, Kent AL. Maternal hypertensive disorders are associated with increased use of respiratory support but not chronic lung disease or poorer neurodevelopmental outcomes in preterm neonates at <29 weeks of gestation. J Paediatr Child Health. 2017;53:391–8.
Robinson M, Mattes E, Oddy WH, de Klerk NH, Li J, McLean NJ, et al. Hypertensive diseases of pregnancy and the development of behavioral problems in childhood and adolescence: the Western Australian Pregnancy Cohort Study. J Pediatr. 2009;154:218–24.
Gray PH, O’Callaghan MJ, Mohay HA, Burns YR, King JF. Maternal hypertension and neurodevelopmental outcome in very preterm infants. Arch Dis Child Fetal Neonatal Ed 1998;79:F88–93.
Love ER, Crum J, Bhattacharya S. Independent effects of pregnancy induced hypertension on childhood development: a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 2012;165:219–24.
Warshafsky C, Pudwell J, Walker M, Wen S-W, Smith GN. Prospective assessment of neurodevelopment in children following a pregnancy complicated by severe pre-eclampsia. BMJ Open. 2016;6:e010884.
Bachnas MA, Akbar MIA, Dachlan EG, Dekker G. The role of magnesium sulfate (MgSO4) in fetal neuroprotection. J Matern Fetal Neonatal Med. 2021;34:966–78.
Acknowledgements
We acknowledge the support of the Canadian Neonatal Network and Canadian Neonatal Follow-up Network who provided the local databases with the standardized definitions.
Funding
ND is supported by the Fonds de recherche du Québec en Santé research salary award. ND also holds an Early Career Professorship in Women’s Heart and Brain Health from the Heart and Stroke Foundation of Canada (Quebec) and McGill University, which partly covered WAA master’s degree stipend.
Author information
Authors and Affiliations
Contributions
WAA conceptualized the study, conducted the analyses, interpreted the results and wrote the paper. AL, RB, AG, TML and MB interpreted the results and critically reviewed the manuscript for important intellectual content. GA and ND conceptualized and designed the study, interpreted the results, and reviewed and revised all manuscript drafts for important intellectual content. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Research ethics board approval was obtained at both institutions (MUHC, MP-37-2019-4876 and CHU-SJ, MEO-37-2019-2125). The need for informed consent was waived due to secondary use of data. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdelmageed, W.A., Lapointe, A., Brown, R. et al. Association between maternal hypertension and infant neurodevelopment in extremely preterm infants. J Perinatol 44, 539–547 (2024). https://doi.org/10.1038/s41372-024-01886-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-024-01886-7