Abstract
Objective
The objective of this study is to assess the impact of maternal age on neurodevelopmental (ND) outcomes of infants < 29 weeks gestational age (GA) at 18–24 months.
Study design
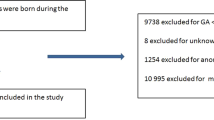
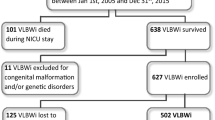
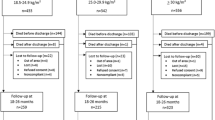
A retrospective cohort study of preterm infants < 29 weeks GA admitted to Canadian tertiary NICUs was performed. The primary outcome was a composite of death or ND impairment (NDI)/significant NDI (sNDI) at 18–24 months. Association between maternal age and outcome was assessed across maternal age groups (15–19, 20–34, 35–39 and ≥40 years) using logistic regression after adjusting for confounders.
Results
Of 3691 eligible infants, 2652 with complete data were included in the analysis. Significant differences in maternal characteristics existed across age groups. The only difference in neonatal characteristics was the incidence of bronchopulmonary dysplasia (p < 0.01). There was no association between maternal age and death or NDI/sNDI after controlling for confounders.
Conclusion
Maternal age is not associated with differences in NDI/sNDI rates among Canadian preterm infants < 29 weeks GA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Blaymore-Bier J, Pezzullo J, Kim E, Oh W, Garcia-Coll C, Vohr BR. Outcome of extremely low-birth-weight infants: 1980–1990. Acta Paediatr. 1994;83:1244–8.
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics. 2000;105:1216–26.
Msall ME, Buck GM, Rogers BT, Merke DP, Wan CC, Catanzaro NL, et al. Multivariate risks among extremely premature infants. J Perinatol. 1994;14:41–7.
Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005;115:696–703.
van Vliet EO, de Kieviet JF, Oosterlaan J, van Elburg RM. Perinatal infections and neurodevelopmental outcome in very preterm and very low-birth-weight infants: a meta-analysis. JAMA Pediatr. 2013;167:662–8.
Marlow N, Wolke D, Bracewell MA, Samara M, Group EPS. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005;352:9–19.
Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N Engl J Med. 2000;343:378–84.
Potharst ES, van Wassenaer AG, Houtzager BA, van Hus JW, Last BF, Kok JH. High incidence of multi-domain disabilities in very preterm children at five years of age. J Pediatr. 2011;159:79–85.
Ko G, Shah P, Lee SK, Asztalos E. Impact of maternal education on cognitive and language scores at 18 to 24 months among extremely preterm neonates. Am J Perinatol. 2013;30:723–30.
Johnson JA, Tough S, SOGC Genetics Committee. Delayed child-bearing. J Obstet Gynaecol Can. 2012;34:80–93.
Aoyama K, Pinto R, Ray JG, Hill AD, Scales DC, Lapinsky SE, et al. Association of maternal age with severe maternal morbidity and mortality in Canada. JAMA Netw Open. 2019;2:e199875.
Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R. The perinatal effects of delayed childbearing. Obstet Gynecol. 2005;105:1410–8.
Kenny LC, Lavender T, McNamee R, O’Neill SM, Mills T, Khashan AS. Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PLoS ONE. 2013;8:e56583.
Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005;105:983–90.
Tough SC, Newburn-Cook C, Johnston DW, Svenson LW, Rose S, Belik J. Delayed childbearing and its impact on population rate changes in lower birth weight, multiple birth, and preterm delivery. Pediatrics. 2002;109:399–403.
Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS ONE. 2017;12:e0186287.
Kanungo J, James A, McMillan D, Lodha A, Faucher D, Lee SK, et al. Advanced maternal age and the outcomes of preterm neonates: a social paradox? Obstet Gynecol. 2011;118:872–7.
Vohr BR, Tyson JE, Wright LL, Perritt RL, Li L, Poole WK, et al. Maternal age, multiple birth, and extremely low birth weight infants. J Pediatr. 2009;154:498–503.
Chen X, Dwyer C, Hader J, Kurji J, Lee C, Lefebvre D, et al. In due time: why maternal age matters. Canadian Institute for Health Information; 2011. Available from: https://secure.cihi.ca/free_products/AIB_InDueTime_WhyMaternalAgeMatters_E.pdf. Accessed 1 Mar 2017.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Bayley N. Manual for the Bayley scales of infant and toddler development. 3rd ed. San Antonio, TX, The Psychological Corporation; 2006.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–43.
Tseng KT, Peng CC, Chang JH, Hsu CH, Lin CY, Jim WT, et al. The impact of advanced maternal age on the outcomes of very low birth weight preterm infants. Medicine. 2019;98:e14336.
Cakmak Celik F, Aygun C, Kucukoduk S, Bek Y. Maternal and neonatal outcomes in advanced maternal age: a retrospective cohort study. J Matern Fetal Neonatal Med. 2017;30:2452–6.
Yen TA, Yang HI, Hsieh WS, Chou HC, Chen CY, Tsou KI, et al. Preeclampsia and the risk of bronchopulmonary dysplasia in VLBW infants: a population based study. PLoS ONE. 2013;8:e75168.
Cheong JLY, Doyle LW. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin Perinatol. 2018;42:478–84.
Katz-Salamon M, Gerner EM, Jonsson B, Lagercrantz H. Early motor and mental development in very preterm infants with chronic lung disease. Arch Dis Child Fetal Neonatal Ed. 2000;83:F1–6.
Lisonkova S, Pare E, Joseph KS. Does advanced maternal age confer a survival advantage to infants born at early gestation? BMC Pregnancy Childbirth. 2013;13:87.
Gray PH, O’Callaghan MJ, Mohay HA, Burns YR, King JF. Maternal hypertension and neurodevelopmental outcome in very preterm infants. Arch Dis Child Fetal Neonatal Ed. 1998;79:F88–93.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454.
Carlo WA, McDonald SA, Fanaroff AA, Vohr BR, Stoll BJ, Ehrenkranz RA, et al. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22 to 25 weeks’ gestation. JAMA. 2011;306:2348–58.
Crowley PA, Antenatal corticosteroid therapy: a meta-analysis of the randomized trials, 1972 to 1994. Am J Obstet Gynecol. 1995;173:322–35.
Marlow N, Bennett C, Draper ES, Hennessy EM, Morgan AS, Costeloe KL. Perinatal outcomes for extremely preterm babies in relation to place of birth in England: the EPICure 2 study. Arch Dis Child Fetal Neonatal Ed. 2014;99:F181–8.
Group E, Fellman V, Hellstrom-Westas L, Norman M, Westgren M, Kallen K, et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA. 2009;301:2225–33.
Sasaki Y, Ishikawa K, Yokoi A, Ikeda T, Sengoku K, Kusuda S, et al. Short- and long-term outcomes of extremely preterm infants in Japan according to outborn/inborn birth status. Pediatr Crit Care Med. 2019;20:963–9.
Guillen U, DeMauro S, Ma L, Zupancic J, Roberts R, Schmidt B, et al. Relationship between attrition and neurodevelopmental impairment rates in extremely preterm infants at 18 to 24 months: a systematic review. Arch Pediatr Adolesc Med. 2012;166:178–84.
Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA. 2014;311:1536–46.
Wong HS, Edwards P. Nature or nurture: a systematic review of the effect of socio-economic status on the developmental and cognitive outcomes of children born preterm. Matern Child Health J. 2013;17:1689–700.
Joseph RM, O’Shea TM, Allred EN, Heeren T, Kuban KK. Maternal educational status at birth, maternal educational advancement, and neurocognitive outcomes at age 10 years among children born extremely preterm. Pediatr Res. 2018;83:767–77.
Benavente-Fernandez I, Synnes A, Grunau RE, Chau V, Ramraj C, Glass T, et al. Association of socioeconomic status and brain injury with neurodevelopmental outcomes of very preterm children. JAMA Netw Open. 2019;2:e192914.
Asztalos EV, Church PT, Riley P, Fajardo C, Shah PS, Canadian Neonatal N, et al. Association between primary caregiver education and cognitive and language development of preterm neonates. Am J Perinatol. 2017;34:364–71.
Acknowledgements
The authors gratefully acknowledge all site investigators of the Canadian Neonatal Network (CNN) and Canadian Neonatal Follow-Up Network (CNFUN). We would also like to extend our thanks to the data abstractors of the CNN, particularly Junmin Yang, as well as the staff at the Maternal-Infant Care Research Centre at Mount Sinai Hospital, Toronto, for providing organizational and statistical support for this project.
Funding
Although no specific funding has been received for this study, organizational support for the Canadian Neonatal Network was provided by the Maternal-Infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by Canadian Institutes of Health Research (CIHR) Team Grant (CTP 87518), the Ontario Ministry of Health and Mount Sinai Hospital. The funding agencies had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review, or approval of the paper; and decision to submit the paper for publication. JGZ is funded by the Michael Smith Foundation for Health Research, Canadian Child Health Clinician Scientist Program, BC Children’s Hospital Research Institute, Sunny Hill Foundation and CIHR.
Author information
Authors and Affiliations
Consortia
Contributions
JD conceptualized and designed the study, obtained research ethics approval, had complete access to the study data that supported the publication, drafted the initial paper and approved the final paper as submitted. JGZ, RS and SD contributed to the interpretation of data, critically reviewed and revised the paper for intellectual content and approved the final paper as submitted. PSS contributed to the concept and design of the study, had complete access to the study data that supported the publication, critically reviewed and revised the paper for intellectual content and approved the final paper as submitted. VS contributed to the concept and design of the study, reviewed the initial study proposal and research ethics application, had complete access to the study data that supported the publication, contributed to the interpretation of data, critically reviewed and revised the paper and approved the final paper as submitted. All authors approved the final paper as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Data collection was approved by the research ethics board or hospital quality improvement committee at each participating hospital contributing to CNN. Approval for this particular study was obtained from Mount Sinai Hospital’s Research Ethics Board and the Steering Committee of the CNN.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Canadian Neonatal Network and Canadian Neonatal Follow-Up Network are listed in a supplementary file.
Supplementary information
Rights and permissions
About this article
Cite this article
DiLabio, J., Zwicker, J.G., Sherlock, R. et al. Maternal age and long-term neurodevelopmental outcomes of preterm infants < 29 weeks gestational age. J Perinatol 41, 1304–1312 (2021). https://doi.org/10.1038/s41372-020-0735-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0735-9
This article is cited by
-
Effect of maternal age on neonatal outcomes in very low birth weight singleton infants: a population-based study
Journal of Perinatology (2023)