Abstract
Background
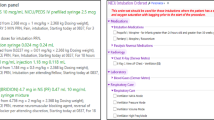
Following the opening of an infant cardiac neonatal intensive care unit, our aim was to determine a baseline UE rate and implement initiatives to target a goal less than 0.5 UEs/100 ventilator days.
Methods
We utilized the Model for Improvement. Key stakeholders included neonatal providers, nurses, and respiratory therapists. We focused on the creation of an airway bundle that addressed securement methods, communication and education.
Results
From October 2017 to January 2018, our baseline UE rate was 0.92 UEs/100 ventilator days. Subsequent to the implementation of an airway bundle with high compliance, we observed a significant change in the centerline (0.45 to 0.02 UEs/100 ventilator days) during the spring of 2021, followed by a period of 480 days with no UEs.
Conclusion
In a unit where UEs were infrequent events, high compliance with an airway bundle led to a significantly sustained decrease in our UE rates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Children’s Hospitals’ Solutions for Patient Safety. Available at http://www.solutionsforpatientsafety.org/. Accessed February, 2018.
Veldman A, Trautschold T, Weiss K, Fischer D, Bauer K. Characteristics and outcome of unplanned extubation in ventilated preterm and term newborns on a neonatal intensive care unit. Pediatr Anesth. 2006;16:968–73.
Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–9.
Barber JA. Unplanned extubation in the NICU. J Obstet Gynecol Neonatal Nurs. 2013;42:233–8.
Hatch LD, Grubb PH, Lea AS, Walsh WF, Markham MH, Whitney GM, et al. Endotracheal intubation in neonates: a prospective study of adverse safety events in 162 infants. J Pediatr. 2016;168:62–66.e6.
Sathyamoorthy M, Lerman J, Okhomina VI, Penman AD. Use of cuffed tracheal tubes in neonates, infants and children: a practice survey of members of the Society of Pediatric Anesthesia. J Clin Anesth. 2016;33:266–72.
Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997;86:627–31.
Pearson TE, Frizzola MA, Khine HH. Uncuffed endotracheal tubes: not appropriate for pediatric critical care transport. Air Med J. 2019;38:51–54.
Dariya V, Moresco L, Bruschettini M, Brion LP. Cuffed versus uncuffed endotracheal tubes for neonates. Cochrane Database Syst Rev. 2022;1:CD013736.
Sadowski R. Continuous quality improvement: reducing unplanned extubations in a pediatric intensive care unit. Pediatrics. 2004;114:628–32.
Merkel L, Beers K, Lewis MM, Stauffer J, Mujsce DJ, Kresch MJ. Reducing unplanned extubations in the NICU. Pediatrics. 2014;133:e1367–72.
Polin RA, Sahni R. Newer experience with CPAP. Semin Neonatol. 2002;7:379–89.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. REDCap Consortium, The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019; [https://doi.org/10.1016/j.jbi.2019.103208].
da Silva PSL, de Aguiar VE, Neto HM, de Carvalho WB. Unplanned extubation in a paediatric intensive care unit: impact of a quality improvement programme. Anaesthesia. 2008;63:1209–16.
Loughead JL, Brennan RA, DeJuilio P, Camposeo V, Jane W, Cooke D. Reducing accidental extubation in neonates. Jt Comm J Qual Patient Saf. 2008;34:164–70.
Sharek PJ, Horbar JD, Mason W, Bisarya H, Thurm CW, Suresh G, et al. Adverse events in the neonatal intensive care unit: development, testing, and findings of an NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics. 2006;118:1332–40.
Kandil SB, Emerson BL, Hooper M, Ciaburri R, Bruno CJ, Cummins N, et al. Reducing unplanned extubations across a children’s hospital using quality improvement methods. Pediatr Qual Saf. 2018;3:e114.
Roddy DJ, Spaeder MC, Pastor W, Stockwell DC, Klugman D. Unplanned extubations in children: impact on hospital cost and length of stay. Pediatr Crit Care Med. 2015;16:572–5.
Hatch LD, Scott TA, Slaughter JC, Xu M, Smith AH, Stark AR, et al. Outcomes, resource use, and financial costs of unplanned extubations in preterm infants. Pediatrics. 2020;145:e20192819.
Nair V, Smith H. Phased quality improvement interventions in reducing unplanned extubations in the neonatal ICU. Respir Care. 2020;65:1511–8.
Ferraz P, Barros M, Miyoshi M, Davidson J, Guinsburg R. Bundle to reduce unplanned extubation in a neonatal intensive care unit. J Matern Fetal Neonatal Med. 2020;33:3077–85.
Klugman D, Melton K, Maynord PO, Dawson A, Madhavan G, Montgomery VL, et al. Assessment of an unplanned extubation bundle to reduce unplanned extubations in critically ill neonates, infants and children. JAMA Pediatr. 2020;174:1–9.
Fontánez-Nieves TD, Frost M, Anday E, Davis D, Cooperberg D, Carey AJ. Prevention of unplanned extubations in neonates through process standardization. J Perinatol. 2016;36:469–73.
Galiote JP, Ridoré M, Carman J, Zell L, Brant K, Gayle C, et al. Reduction in Unintended Extubations in a Level IV Neonatal Intensive Care Unit. Pediatrics. 2019;143:e20180897.
Lai M, Inglis GD, Hose K, Jardine LA, Davies MW. Methods for securing endotracheal tubes in newborn infants. Cochrane Neonatal Group, editor. Cochrane Database Syst Rev [Internet]. 2014 Jul 31 [cited 2020 May 27]; Available from: https://doi.org/10.1002/14651858.CD007805.pub2.
Mahaseth M, Woldt E, Zajac ME, Mazzeo B, Basirico J, Natarajan G. Reducing unplanned extubations in a level IV neonatal intensive care unit: the elusive benchmark. Pediatr Qual Saf. 2020;5:e337.
Donn SM, Kuhns LR. Mechanism of endotracheal tube movement with change of head position in the neonate. Pediatr Radiol. 1980;9:37–40.
Todres ID, Moylan FMB. Endotracheal tube displacement in the newborn infant. J Pediatr. 1976;89:126–7.
Hatch L, Grubb P, Markham M, Scott T, Walsh W, Slaughter J, et al. Effect of anatomical and developmental factors on the risk of unplanned extubation in critically ill newborns. Am J Perinatol. 2017;34:1234–40.
Morris HF, Schuller L, Archer J, Niesen A, Ellsworth S, Egan J, et al. Decreasing unplanned extubation in the neonatal ICU with a focus on endotracheal tube tip position. Respir Care. 2020;65:1648–54.
Crezeé KL, DiGeronimo RJ, Rigby MJ, Carter RC, Patel S. Reducing unplanned extubations in the NICU following implementation of a standardized approach. Respir Care. 2017;62:1030–5.
Klugman D, Berger JT, Spaeder MC, Wright A, Pastor W, Stockwell DC. Acute harm: unplanned extubations and cardiopulmonary resuscitation in children and neonates. Intensive Care Med. 2013;39:1333–4.
Donn SM, Blane CE. Endotracheal tube movement in the preterm neonate: oral versus nasal intubation. Ann Otol Rhinol Laryngol. 1985;94:18–20.
Spitzer AR. Postextubation atelectasis-the role of oral versus nasal endotracheal tubes. J Pediatr. 1982;100:806–10.
McMillan DD, Rademaker AW, Buchan KA, Reid A, Machin G, Suave RS. Benefits of orotracheal and nasotracheal intubation in neonates requiring ventilatory assistance. Pediatrics 1986;77:39–44.
Spence K, Barr P, Cochrane Neonatal Group. Nasal versus oral intubation of mechanical ventilation of newborn infants. Cochrane Database Syst Rev. 1999;1999:CD000948.
Greenhalgh T, Papoutsi C. Spreading and scaling up innovation and improvement. BMJ. 2019;365:l2068.
Acknowledgements
We want to thank our nursing champions, respiratory therapists, radiology technicians, neonatology providers, Dr. Ganga Krishnamurthy, Dr. Nimrod Goldshtrom, Dr. Rakesh Sahni, Dr. Jen-Tien Wung, Dr. John Babineau, Aalya Chippa, Cynthia Okerfelt, Lynn Kim and clinical systems engineers at NewYork-Presbyterian for their support and guidance throughout this project. There was no external funding for this manuscript.
Funding
All authors have indicated they have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
Drs. Shui and Vargas conceptualized and designed the study and data collection instruments, and reviewed and revised the manuscript. Dr. Kim designed the data collection instruments, collected data and carried out the initial and final draft of the manuscript. Dr. Blancha Eckels collected data, reviewed and revised the manuscript. Dr. Brachio carried out the initial and final analyses, and reviewed and revised the final manuscript. Ms. Gomez, Brooks and Villaraza-Morales helped to design the data collection instruments, collected and audited data on a regular basis and reviewed and revised the final manuscript. Ms. Ehret reviewed the final analyses and revised the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, F., Eckels, V.B., Brachio, S.S. et al. Use of an airway bundle to reduce unplanned extubations in a neonatal intensive care unit. J Perinatol 44, 314–320 (2024). https://doi.org/10.1038/s41372-024-01879-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-024-01879-6