Abstract
Objective
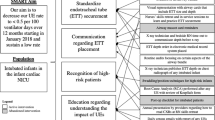
We sought to standardize and improve compliance with evidence-based premedication for non-emergent neonatal intubations in two academic-affiliated Neonatal Intensive Care Units.
Study design
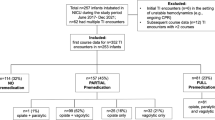
A multidisciplinary team created guidelines and electronic medical record order sets for intubation. Compliance with recommended premedication, number of intubation attempts, and frequency of bradycardia and desaturation were assessed.
Results
387 intubation procedures were reviewed. Provision of recommended premedication increased by 36% and 75% at the level III and IV units, respectively. Decreased frequency of bradycardia during intubation (p = 0.0003) occurred in the level III unit. A reduction in number of intubation attempts (p ≤ 0.001), improvement in first-attempt intubation success (p ≤ 0.001), and decreased frequency of bradycardia (p = 0.01) and desaturation (p = 0.02) during intubation occurred in the level IV unit.
Conclusions
This quality improvement initiative improved standardized premedication compliance and decreased adverse events associated with non-emergent neonatal intubations in two separate units.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Raju T, Suresh G, Higgins R. Patient safety in the context of neonatal intensive care: research and educational opportunities. Pediatric Res. 2011;70:109–15.
Foglia E, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–9.
Hatch L, Grubb P, Lea A, Walsh W, Markham M, Whitney G, et al. Endotracheal intubation in neonates: a prospective study of adverse safety events in 162 infants. J Pediatrics. 2016;168:62–6.
Sauer C, Kong J, Vaucher Y, Finer N, Proudfoot J, Boutin M, et al. Intubation attempts increase the risk for severe intraventricular hemorrhage in preterm infants – a retrospective cohort study. J Pediatr. 2016;177:108–13.
Wallenstein M, Birnie K, Arain Y, Yang W, Yamada N, Huffman L, et al. Failed endotracheal intubation and adverse outcomes among extremely low birth weight infants. J Perinatol. 2016;36:112–5.
Pouppirt N, Nassar R, Napolitano N, Nawab U, Nishisaki A, Nadkarni V, et al. Association between video laryngoscopy and adverse tracheal intubation-associated events in the neonatal intensive care unit. J Pediatr. 2018;201:281–4.
Sawyer T, Foglia E, Ades A, Moussa A, Napolitano N, Glass K, et al. Incidence, impact and indicators of difficult intubations in the neonatal intensive care unit: a report from the National Emergency Airway Registry for Neonates. Arch Dis Child Fetal Neonatal Ed. 2019;104:F461–466.
Foglia E, Ades A, Sawyer T, Glass K, Singh N, Jung P, et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics. 2019;143:e20180902.
Anand KJ. The International Evidence-Based Group for Neonatal Pain Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med. 2011;155:173–80.
Kumar P, Denson S, Mancuso T. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125:608–15.
Barrington K. Premedication for endotracheal intubation in the newborn infant. Paediatrics Child Health. 2011;16:159–64.
Ancora G, Lago P, Garetti E, Merazzi D, Levet P, Bellieni C, et al. Evidence-based clinical guidelines on analgesia and sedation in newborn infants undergoing assisted ventilation and endotracheal intubation. Acta Paediatrics. 2018;108:208–17.
Roberts K, Leone T, Edwards W, Rich W, Finer N. Premedication for nonemergent neonatal intubations: a randomized, controlled trial comparing atropine and fentanyl to atropine, fentanyl, and mivacurium. Pediatrics. 2006;118:1583–91.
Feltman D, Weiss M, Nicoski P, Sinacore J. Rocuronium for nonemergent intubation of term and preterm infants. J Perinatol. 2011;31:38–43.
Krick J, Gray M, Umoren R, Lee G, Sawyer T. Premedication with paralysis improves intubation success and decreases adverse events in very low birth weight infants: a prospective cohort study. J Perinatol. 2018;38:681–6.
Ghanta S, Abdel-Latif M, Lui K, Ravindranathan H, Awad J, Oei J. Propofol compared with the morphine, atropine and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics. 2007;119:e1248–55.
de Kort E, Prins S, Reiss I, Willemsen S, Andriessen P, Weissenbruch. M, et al. Propofol for endotracheal intubation in neonates: a dose-finding trial. Arch Dis Child Fetal Neonatal Ed. 2020; https://doi.org/10.1136/fetalneonatal-2019-318474.
Simons S, Lee R, Reiss I, Weissenbruch M. Clinical evaluation of propofol as sedative for endotracheal intubation in neonates. Acta Paediatrica. 2013;102:487–92.
Smits A, Thewissen L, Caicedo A, Naulaers G, Allegaert K. Propofol dose-finding to reach optimal effect for (semi-)elective intubation in neonates. J Pediatrics. 2016;179:54–60.
Welzing L, Kribs A, Eifinger F, Huenseler C, Oberthuer A, Roth B. Propofol as an induction agent for endotracheal intubation can cause significant arterial hypotension in preterm neonates. Pediatr Anesthesia. 2010;20:585–90.
Muniraman H, Yaari J, Hand I. Premedication use before nonemergent intubation in the newborn infant. Am J Perinatol. 2015;32:821–4.
Sarkar S, Schumacher R, Baumgart S, Donn S. Are newborns receiving premedication before elective intubation? J Perinatol. 2006;26:286–9.
National Emergency Airway Registry for Neonates (NEAR4NEOS). https://www.near4neos.org/.
Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Provost L, Murray S. The health care data guide: learning from data for improvement. San Francisco: Jossey-Bass, Publication; 2011.
Mari J, Franczia P, Margas W, Rutkowski J, Bebrysz M, Bokiniec R, et al. International consensus is needed on premedication for non-emergency neonatal intubation after survey found wide-ranging policies and practices in 70 countries. Acta Paediatrica. 2019;00:1–7.
Hatch L, Grubb P, Lea A, Walsh W, Markham M, Maynord P, et al. Interventions to improve patient safety during intubation in the neonatal intensive care unit. Pediatrics 2016;138:e20160069.
Author information
Authors and Affiliations
Contributions
RS designed the study, collected data, analyzed the data and wrote the manuscript. BW analyzed the data, created tables, and helped to write the manuscript. TG and JB designed the study and helped to write the manuscript. The authors acknowledge the expertise and input from the multidisciplinary care team at the University Colorado Hospital NICU and the Children’s Hospital Colorado NICU including nursing, respiratory therapy, pharmacy, advanced practiced providers, resident physicians, fellow physicians and faculty.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shay, R., Weikel, B.W., Grover, T. et al. Standardizing premedication for non-emergent neonatal tracheal intubations improves compliance and patient outcomes. J Perinatol 42, 132–138 (2022). https://doi.org/10.1038/s41372-021-01215-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01215-2