Abstract
Objective
To evaluate the relationship between cholestasis and outcomes in medical and surgical necrotizing enterocolitis (NEC).
Study design
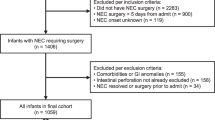
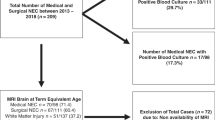
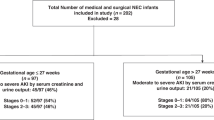
A retrospective analysis of prospectively collected data from 1472 infants with NEC [455 medical (mNEC) and 1017 surgical (sNEC)] from the Children’s Hospital Neonatal Database.
Results
The prevalence of cholestasis was lower in mNEC versus sNEC (38.2% vs 70.1%, p < 0.001). In both groups, cholestasis was associated with lower birth gestational age [mNEC: OR 0.79 (95% CI 0.68–0.92); sNEC: OR 0.86 (95% CI 0.79–0.95)] and increased days of parenteral nutrition [mNEC: OR 1.08 (95% CI 1.04–1.13); sNEC: OR 1.01 (95% CI 1.01–1.02)]. For both groups, the highest direct bilirubin was associated with the composite outcome mortality or length of stay >75th percentile [mNEC: OR 1.21 (95% CI 1.06–1.38); sNEC: OR 1.06 (95% CI 1.03–1.09)].
Conclusion
Cholestasis with both medical NEC and surgical NEC is associated with adverse patient outcomes including increased mortality or extreme length of stay.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data relevant to the study is included in the article. Requests for additional material can be made to Pritha.nayak@utsouthwestern.edu.
References
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, in-hospital morbidity, care practices, and 2-year outcomes for extremely preterm infants in the US, 2013–2018. Jama. 2022;327:248–63.
Jones IH, Hall NJ. Contemporary outcomes for infants with necrotizing enterocolitis—a systematic review. J Pediatr. 2020;220:86–92.e3.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. Jama. 2015;314:1039–51.
Vaidya R, Yi JX, O’Shea TM, Jensen ET, Joseph RM, Shenberger J, et al. Long-term outcome of necrotizing enterocolitis and spontaneous intestinal perforation. Pediatrics. 2022;150:e2022056445.
Modi BP, Galloway DP, Gura K, Nucci A, Plogsted S, Tucker A, et al. ASPEN definitions in pediatric intestinal failure. JPEN J Parenter Enteral Nutr. 2022;46:42–59.
Christensen RD, Henry E, Wiedmeier SE, Burnett J, Lambert DK. Identifying patients, on the first day of life, at high-risk of developing parenteral nutrition-associated liver disease. J Perinatol. 2007;27:284–90.
Fatemizadeh R, Gollins L, Hagan J, Debuyserie A, King K, Vogel AM, et al. In neonatal-onset surgical short bowel syndrome survival is high, and enteral autonomy is related to residual bowel length. JPEN J Parenter Enteral Nutr. 2022;46:339–47.
Lee WS, Chew KS, Ng RT, Kasmi KE, Sokol RJ. Intestinal failure-associated liver disease (IFALD): insights into pathogenesis and advances in management. Hepatol Int. 2020;14:305–16.
Karila K, Anttila A, Iber T, Pakarinen M, Koivusalo A. Intestinal failure associated cholestasis in surgical necrotizing enterocolitis and spontaneous intestinal perforation. J Pediatr Surg. 2019;54:460–4.
Veenstra M, Danielson L, Brownie E, Saba M, Natarajan G, Klein M. Enteral nutrition and total parenteral nutrition components in the course of total parenteral nutrition-associated cholestasis in neonatal necrotizing enterocolitis. Surgery. 2014;156:578–83.
Moss RL, Das JB, Raffensperger JG. Necrotizing enterocolitis and total parenteral nutrition-associated cholestasis. Nutrition. 1996;12:340–3.
Lauriti G, Zani A, Aufieri R, Cananzi M, Chiesa PL, Eaton S, et al. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: a systematic review. JPEN J Parenter Enteral Nutr. 2014;38:70–85.
Guthrie SO, Gordon PV, Thomas V, Thorp JA, Peabody J, Clark RH. Necrotizing enterocolitis among neonates in the United States. J Perinatol. 2003;23:278–85.
Llanos AR, Moss ME, Pinzon MC, Dye T, Sinkin RA, Kendig JW. Epidemiology of neonatal necrotising enterocolitis: a population-based study. Paediatr Perinat Epidemiol. 2002;16:342–9.
Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK, et al. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–304.
Kosters A, Karpen SJ. The role of inflammation in cholestasis: clinical and basic aspects. Semin Liver Dis. 2010;30:186–94.
Heida FH, Loos MH, Stolwijk L, Te Kiefte BJ, van den Ende SJ, Onland W, et al. Risk factors associated with postnecrotizing enterocolitis strictures in infants. J Pediatr Surg. 2016;51:1126–30.
Ahmad I, Premkumar MH, Hair AB, Sullivan KM, Zaniletti I, Sharma J, et al. Variability in antibiotic duration for necrotizing enterocolitis and outcomes in a large multicenter cohort. J Perinatol. 2022;42:1458–64.
Patel EU, Wilson DA, Brennan EA, Lesher AP, Ryan RM. Earlier re-initiation of enteral feeding after necrotizing enterocolitis decreases recurrence or stricture: a systematic review and meta-analysis. J Perinatol. 2020;40:1679–87.
Niccum M, Khan MN, Middleton JP, Vergales BD, Syed S. Cholestasis affects enteral tolerance and prospective weight gain in the NICU. Clin Nutr ESPEN. 2019;30:119–25.
Teng J, Bohlin K, Nemeth A, Fischler B. Cholestasis after very preterm birth was associated with adverse neonatal outcomes but no significant long-term liver disease: a population-based study. Acta Paediatr. 2021;110:141–8.
Javid PJ, Oron AP, Duggan CP, Squires RH, Horslen SP. Pediatric Intestinal Failure C. The extent of intestinal failure-associated liver disease in patients referred for intestinal rehabilitation is associated with increased mortality: an analysis of the Pediatric Intestinal Failure Consortium database. J Pediatr Surg. 2018;53:1399–402.
Willis TC, Carter BA, Rogers SP, Hawthorne KM, Hicks PD, Abrams SA. High rates of mortality and morbidity occur in infants with parenteral nutrition-associated cholestasis. JPEN J Parenter Enteral Nutr. 2010;34:32–7.
Premkumar MH, Carter BA, Hawthorne KM, King K, Abrams SA. Fish oil-based lipid emulsions in the treatment of parenteral nutrition-associated liver disease: an ongoing positive experience. Adv Nutr. 2014;5:65–70.
Sjoberg Bexelius T, Ahle M, Elfvin A, Björling O, Ludvigsson JF, Andersson RE. Intestinal failure after necrotising enterocolitis: incidence and risk factors in a Swedish population-based longitudinal study. BMJ Paediatr Open. 2018;2:e000316.
Murthy K, Pallotto EK, Gien J, Brozanski BS, Porta NF, Zaniletti I, et al. Predicting death or extended length of stay in infants with congenital diaphragmatic hernia. J Perinatol. 2016;36:654–9.
Acknowledgements
Beverly Brozanski, Jacquelyn Evans, Theresa Grover, Karna Murthy, Michael Padula, Eugenia Pallotto, Anthony Piazza, Kristina Reber and Billie Short and ex-officio David Durand, Francine Dykes, Jeanette Asselin), are executive members of the Children’s Hospitals Neonatal Consortium, Inc., who developed and manage the CHND (thechnc.org). For more information, please contact: exec@thechnc.org. We are indebted to the following CHNC participating institutions that serve the infants and their families; these institutions (and their site sponsors) also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND): 1. Atlanta, Children’s Healthcare of Atlanta – Egleston (Anthony Piazza) 2. Atlanta, Children’s Healthcare of Atlanta - Scottish Rite (Gregory Sysyn) 3. Austin, Dell Children’s (Ashley Lucke, Molly Pont) 4. Birmingham, Children’s of Alabama (Allison Black, Carl Coghill) 5. Boston Children’s Hospital (Anne Hansen) 6. Charlotte, Levine Children’s Hospital (Eugenia Pallotto) 7. Chicago, Ann & Robert H. Lurie Children’s Hospital (Karna Murthy, Gustave Falciglia) 8. Cincinnati Children’s Hospital (Beth Haberman) 9. Cleveland Clinic (Tetyana Nesterenko) 10. Columbus, Nationwide Children’s Hospital (Thomas Bartman) 11. Dallas, Children’s Medical Center (Sushmita Yallapragada, Lina Chalak) 12. Denver, Children’s Hospital Colorado (Danielle Smith, Stephanie Bourque) 13. Detroit, Children’s Hospital Michigan (Girija Natarjan) 14. Ft. Worth, Cook Children’s Healthcare System (Annie Chi, Yvette Johnson) 15. Hartford, Connecticut Children’s (Annmarie Gotiolo) 16. Houston, Texas Children’s Hospital (Lakshmi Katarkan, Kristina Reber) 17. Indianapolis, Riley Children’s Health (Rebecca Rose) 18. Iowa City, University of Iowa Stead Family Children’s Hospital (Julie Lindower) 19. Kansas City, The Children’s Mercy Hospital (Julie Weiner) 20. Little Rock, Arkansas Children’s (Laura Carroll) 21. Los Angeles Children’s Hospital (Rachel Chapman) 22. Madison, American Family Children’s Hospital (Nina Menda) 23. Memphis, Le Bonheur Children’s Hospital (Mark Weems) 24. Minneapolis, Children’s Minnesota (Ann Downey) 25. Milwaukee, Wisconsin Children’s Hospital (Joanne Lagatta) 26. Oakland, UCSF Benioff Children’s Hospital (Priscilla Joe) 27. Oklahoma Children’s Hospital (Trent Tipple, Patricia Williams) 28. Omaha Children’s Hospital (Nicole Birge) 29. Orange County, Children’s Hospital of Orange County (Michel Mikhael) 30. Orlando, AdventHealth for Children (Narendra Dereddy, Rajan Wadhawan) 31. Orlando, Nemours Children’s Hospital (Aaron Weiss) 32. Philadelphia, Children’s Hospital of Philadelphia (Michael Padula) 33. Philadelphia, St. Christopher’s Hospital for Children (Vilarmis Quinones) 34. Phoenix Children’s Hospital (Pam Griffiths) 35. Pittsburgh Children’s Hospital (Toby Yanowitz) 36. Rochester, MN, Mayo Clinic Children’s (Ellen Bendel-Stenzel) 37. Salt Lake City, Primary Children’s Hospital (Con Yee Ling) 38. San Diego, Rady Children’s Hospital (Mark Speziale) 39. Seattle Children’s Hospital (Robert DiGeronimo, Elizabeth Jacobsen) 40. St. Louis Children’s Hospital (Beverly Brozanski, Rakesh Rao) 41. St Paul, Children’s Minnesota (Ann Downey) 42. St. Petersburg, All Children’s Hospital (Linda Van Marter) 43. Toronto, The Hospital for Sick Children (Kyong-Soon Lee) 44. Washington, Children’s National Hospital (Billie Lou Short) 45. Wilmington, Nemours/Alfred I. duPont Hospital for Children (Kevin Sullivan) 46. Winston-Salem, Brenner Children’s Hospital (Cherrie Welch).
Author information
Authors and Affiliations
Consortia
Contributions
SPN, KAH, MP, and TY contributed to the conception and design of the study. All authors contributed to the data acquisition and provided critical input during the Children’s Hospitals Neonatal Consortium NEC focus group meetings. IZ conducted data analysis. SPN and KAH contributed equally to drafting the manuscript. MP and TY helped to critically draft and revise the manuscript. All authors helped revise the manuscript and have approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Compliance with ethical standards
IRB approval was obtained at each participating site prior to entering data into CHND. For analysis of de-identified data the Stanley Manne Research Center (2011-14673) reviewed and approved this work. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nayak, S.P., Huff, K.A., Zaniletti, I. et al. Cholestasis is associated with a higher rate of complications in both medical and surgical necrotizing enterocolitis. J Perinatol 44, 100–107 (2024). https://doi.org/10.1038/s41372-023-01787-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01787-1