Abstract
Objective
To elucidate the relationship between abnormal lung function (LF) at school age and neonatal respiratory support in very low birth weight children with bronchopulmonary dysplasia (BPD).
Study design
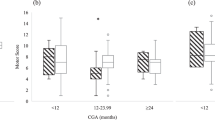
We retrospectively examined 78 BPD children whose LF was evaluated at 8–9 years. LF abnormalities were defined by reduced values of spirometric parameters. Adjusted odds ratios (aORs) for abnormal LF by the type and postmenstrual age (PMA) of respiratory support were calculated using logistic regression analysis after controlling perinatal factors.
Results
Overall, 24 (31%) patients had LF abnormalities. Antenatal steroid use was associated with a decreased risk of abnormal LF [aOR, 0.31; 95% CI, 0.09–0.92]. Requiring positive-pressure support at 37 weeks’ PMA correlated with abnormal LF [aOR, 4.58; 95% CI, 1.15–21.90]; whereas only low-flow oxygen at any PMA did not.
Conclusion
Requiring positive-pressure support at 37 weeks’ PMA could be an indicator of abnormal LF at school age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data relevant to the study are included in the article or supplied as supplementary information.
References
Lui K, Lee SK, Kusuda S, Adams M, Vento M, Reichman B, et al. Trends in outcomes for neonates born very preterm and very low birth weight in 11 high-income countries. J Pediatr. 2019;215:32–40.e14.
Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. JAMA. 2016;316:611–24.
Doyle LW, Andersson S, Bush A, Cheong JLY, Clemm H, Evensen KAI, et al. Expiratory airflow in late adolescence and early adulthood in individuals born very preterm or with very low birthweight compared with controls born at term or with normal birthweight: a meta-analysis of individual participant data. Lancet Respir Med. 2019;7:677–86.
Eves R, Mendonca M, Baumann N, Ni Y, Darlow BA, Horwood J, et al. Association of very preterm birth or very low birth weight with intelligence in adulthood: an individual participant data meta-analysis. JAMA Pediatr. 2021;175:e211058.
Keller RL, Feng R, DeMauro SB, Ferkol T, Hardie W, Rogers EE, et al. Bronchopulmonary dysplasia and perinatal characteristics predict 1-year respiratory outcomes in newborns born at extremely low gestational age: a prospective cohort study. J Pediatr. 2017;187:89–97.e3.
Hennessy EM, Bracewell MA, Wood N, Wolke D, Costeloe K, Gibson A, et al. Respiratory health in pre-school and school age children following extremely preterm birth. Arch Dis Child. 2008;93:1037–43.
Islam JY, Keller RL, Aschner JL, Hartert TV, Moore PE. Understanding the short- and long-term respiratory outcomes of prematurity and bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2015;192:134–56.
Um-Bergström P, Hallberg J, Thunqvist P, Berggren-Broström E, Anderson M, Adenfelt G, et al. Lung function development after preterm birth in relation to severity of Bronchopulmonary dysplasia. BMC Pulm Med. 2017;17:97.
Hirata K, Nishihara M, Shiraishi J, Hirano S, Matsunami K, Sumi K, et al. Perinatal factors associated with long-term respiratory sequelae in extremely low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2015;100:F314–9.
Doyle LW, Adams AM, Robertson C, Ranganathan S, Davis NM, Lee KJ, et al. Increasing airway obstruction from 8 to 18 years in extremely preterm/low-birthweight survivors born in the surfactant era. Thorax. 2017;72:712–9.
Bancalari E, Abdenour GE, Feller R, Gannon J. Bronchopulmonary dysplasia: clinical presentation. J Pediatr. 1979;95:819–23.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Stoecklin B, Simpson SJ, Pillow JJ. Bronchopulmonary dysplasia: rationale for a pathophysiological rather than treatment based approach to diagnosis. Paediatr Respir Rev. 2019;32:91–7.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Isayama T, Lee SK, Yang J, Lee D, Daspal S, Dunn M, et al. Revisiting the definition of bronchopulmonary dysplasia: effect of changing panoply of respiratory support for preterm neonates. JAMA Pediatr. 2017;171:271–9.
The Japan Neonatal Follow-up Study Group. Protocol for the multicenter follow-up study of VLBW infants (in Japanese). [cited 2022 Feb 11]. http://highrisk-followup.jp/schedule/.
Wechsler D. Wechsler Intelligence Scale for Children-third edition. Psychological Corporation: San Antonio, Texas, 1991.
Wechsler D. Weschsler Intelligence Scale for Children-fourth edition. Psychological Corporation: San Antonio, Texas, 2003.
Sugihara K, Sugihara T, Nakamura J, Okawa I, Nohara R, Serizawa N Tanaka Binet intelligence Scale V. Taken Shuppan: Tokyo, 2003.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68.
Blanc WA. Pathology of the placenta, membranes, and umbilical cord in bacterial, fungal, and viral infections in man. Monogr Pathol. 1981;22:67–132.
Chida S, Fujiwara T, Konishi M, Takahashi H, Sasaki M. Stable microbubble test for predicting the risk of respiratory distress syndrome: II. Prospective evaluation of the test on amniotic fluid and gastric aspirate. Eur J Pediatr. 1993;152:152–6.
Kawai M. Late-onset circulatory collapse of prematurity. Pediatr Int. 2017;59:391–6.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Benaron DA, Benitz WE. Maximizing the stability of oxygen delivered via nasal cannula. Arch Pediatr Adolesc Med. 1994;148:294–300.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A. Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol. 2003;23:451–6.
Takase M, Sakata H, Shikada M, Tatara K, Fukushima T, Miyakawa T. Development of reference equations for spirometry in Japanese children aged 6-18 years. Pediatr Pulmonol. 2013;48:35–44.
Ronkainen E, Dunder T, Kaukola T, Marttila R, Hallman M. Intrauterine growth restriction predicts lower lung function at school age in children born very preterm. Arch Dis Child Fetal Neonatal Ed. 2016;101:F412–7.
Silveyra P, Fuentes N, Rodriguez Bauza DE. Sex and gender differences in lung disease. Adv Exp Med Biol. 2021;1304:227–58.
McGoldrick E, Stewart F, Parker R, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12:CD004454.
Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N. Engl J Med. 2000;342:1500–7.
Jackson WM, O’Shea TM, Allred EN, Laughon MM, Gower WA, Leviton A. Risk factors for chronic lung disease and asthma differ among children born extremely preterm. Pediatr Pulmonol. 2018;53:1533–40.
Lo DK, Beardsmore CS, Roland D, Richardson M, Yang Y, Danvers L, et al. Lung function and asthma control in school-age children managed in UK primary care: a cohort study. Thorax. 2020;75:101–7.
Vyas-Read S, Logan JW, Cuna AC, Machry J, Leeman KT, Rose RS, et al. A comparison of newer classifications of bronchopulmonary dysplasia: findings from the Children’s Hospitals Neonatal Consortium Severe BPD Group. J Perinatol. 2022;42:58–64.
Saengrat P, Limrungsikul A. Predictive ability of the new bronchopulmonary dysplasia definition on pulmonary outcomes at 20 to 24 months’ corrected age of preterm infants. Am J Perinatol 2021; https://doi.org/10.1055/s-0041-1735219.
Hines D, Modi N, Lee SK, Isayama T, Sjörs G, Gagliardi L, et al. Scoping review shows wide variation in the definitions of bronchopulmonary dysplasia in preterm infants and calls for a consensus. Acta Paediatr. 2017;106:366–74.
Crowther CA, Anderson PJ, McKinlay CJ, Harding JE, Ashwood PJ, Haslam RR, et al. Mid-Childhood outcomes of repeat antenatal corticosteroids: A randomized controlled trial. Pediatrics. 2016;138:e20160947 https://doi.org/10.1542/peds.2016-0947.
Doyle LW, Irving L, Haikerwal A, Lee K, Ranganathan S, Cheong J. Airway obstruction in young adults born extremely preterm or extremely low birth weight in the postsurfactant era. Thorax. 2019;74:1147–53.
Cools F, Offringa M, Askie LM Elective high-frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2015:CD000104. https://doi.org/10.1002/14651858.CD000104.epub4.
Fawke J, Lum S, Kirkby J, Hennessy E, Marlow N, Rowell V, et al. Lung function and respiratory symptoms at 11 years in children born extremely preterm: the EPICure study. Am J Respir Crit Care Med. 2010;182:237–45.
Stern DA, Morgan WJ, Wright AL, Guerra S, Martinez FD. Poor airway function in early infancy and lung function by age 22 years: a non-selective longitudinal cohort study. Lancet. 2007;370:758–64.
van Meel ER, den Dekker HT, Elbert NJ, Jansen PW, Moll HA, Reiss IK, et al. A population-based prospective cohort study examining the influence of early-life respiratory tract infections on school-age lung function and asthma. Thorax. 2018;73:167–73.
Belgrave DCM, Granell R, Turner SW, Curtin JA, Buchan IE, Le Souëf PN, et al. Lung function trajectories from pre-school age to adulthood and their associations with early life factors: a retrospective analysis of three population-based birth cohort studies. Lancet Respir Med. 2018;6:526–34.
Acknowledgements
The authors are grateful to clinical laboratory technicians at Jichi Medical University Hospital for conducting LF testing. No funding was secured for this study.
Author information
Authors and Affiliations
Contributions
YS contributed to the study design, methodology, investigation, data curation, and formal analysis as well as drafted the initial manuscript. YK contributed to the study design and methodology, provided supervision and resources, and drafted and revised the manuscript. YY provided supervision and revised the manuscript. HS, MM, SK, and MS contributed to data curation and revised the manuscript. TY provided supervision and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suzuki, Y., Kono, Y., Yada, Y. et al. Neonatal respiratory support related to lung function abnormalities in school-age children with bronchopulmonary dysplasia. J Perinatol 43, 337–344 (2023). https://doi.org/10.1038/s41372-023-01609-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01609-4