Abstract
Objective
To compare rural obstetric patient and neonate characteristics and outcomes by birth location.
Methods
Retrospective observational cohort study of rural residents’ hospital births from California, Pennsylvania, and South Carolina. Hospitals in rural counties were rural-located, those in metropolitan counties with ≥10% of obstetric patients from rural communities were rural-serving, metropolitan-located, others were non-rural-serving, metropolitan-located. Any adverse obstetric patient or neonatal outcomes were assessed with logistic regression accounting for patient characteristics, state, year, and hospital.
Results
Of 466,896 rural patient births, 64.3% occurred in rural-located, 22.5% in rural-serving, metropolitan-located, and 13.1% in non-rural-serving, metropolitan-located hospitals. The odds of any adverse outcome increased in rural-serving (aOR 1.27, 95% CI 1.10–1.46) and non-rural-serving (aOR 1.35, 95% CI 1.18–1.55) metropolitan-located hospitals.
Conclusion
One-third of rural obstetric patients received care in metropolitan-located hospitals. These patients have higher comorbidity rates and higher odds of adverse outcomes likely reflecting referral for higher baseline illness severity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data generated and analyzed during the current study are not publicly available due to data use agreements, but may be available from the senior author on reasonable request.
References
Ratcliffe M, Burd C, Holder K, Fields A. Defining Rural at the U.S. Census Bureau. 2016. http://www2.census.gov. Accessed 5 April 2021.
National Advisory Committee on Rural Health and Human Services. Maternal and obstetric care challenges in rural America: policy brief and recommendations to the secretary. 2020. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2020-maternal-obstetric-care-challenges.pdf. Accessed 14 July 2021.
Maron D. Maternal health care is disappearing in Rural America. Sci Am. 2016. https://www.scientificamerican.com/article/maternal-health-care-is-disappearing-in-rural-america/#. Accessed 29 Mar 2022.
Ely DM, Hoyert DL. Differences between rural and urban areas in mortality rates for the leading causes of infant death: United States, 2013–2015. NCHS Data Brief. 2018;300:1–8.
Womack LS, Rossen LM, Hirai AH. Urban-rural infant mortality disparities by race and ethnicity and cause of death. Am J Prev Med. 2020;58:254–60.
Ehrenthal DB, Daphne Kuo HH, Kirby RS. Infant mortality in rural and nonrural counties in the United States. Pediatrics. 2020;146:e20200464.
Grünebaum A, McCullough LB, Orosz B, Chervenak FA. Neonatal mortality in the United States is related to location of birth (hospital versus home) rather than the type of birth attendant. Am J Obstet Gynecol. 2020;223:254.e1–254.e8.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–75.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304:992–1000.
Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8.
Kozhimannil KB, Interrante JD, Tuttle MKS, Henning-Smith C. Changes in hospital-based obstetric services in rural US counties, 2014-2018. JAMA. 2020;324:197.
Handley SC, Passarella M, Herrick HM, Interrante JD, Lorch SA, Kozhimannil KB, et al. Birth volume and geographic distribution of US hospitals with obstetric services from 2010 to 2018. JAMA Netw Open. 2021;4:1–12.
Kaufman BG, Thomas SR, Randolph RK, Perry JR, Thompson KW, Holmes GM, et al. The rising rate of rural hospital closures. J Rural Health. 2016;32:35–43.
Lorch SA, Srinivas SK, Ahlberg C, Small DS. The impact of obstetric unit closures on maternal and infant pregnancy outcomes. Health Serv Res. 2013;48:455–75. 2 PART1
Kozhimannil KB, Hung P, Henning-Smith C, Casey MM, Prasad S. Association between loss of hospital-based obstetric services and birth outcomes in rural counties in the United States. JAMA. 2018;319:1239–47.
Aubrey-Bassler F, Cullen R, Simms A, Asghari S, Crane J, Wang PP, et al. Population-based cohort study of hospital delivery volume, geogrpahic accessibility, and obstetric outcomes. Int J Gynecol Obstet. 2019;146:95–102.
Burris HH, Passarella M, Handley SC, Srinivas SK, Lorch SA. Black-White disparities in maternal in-hospital mortality according to teaching and Black-serving hospital status. Am J Obstet Gynecol. 2021;225:e1–9.
Kozhimannil KB, Casey MM, Hung P, Prasad S, Moscovice IS. Location of childbirth for rural women: implications for maternal levels of care. Am J Obstet Gynecol. 2016;214:661.e1–661.e10.
Ryan GM. Toward improving the outcome of pregnancy recommendations for the regional development of perinatal health services. Obstet Gynecol. 1975;46:375–84.
Okoroh EM, Kroelinger CD, Lasswell SM, Goodman DA, Williams AM, Barfield WD. United States and territory policies supporting maternal and neonatal transfer: review of transport and reimbursement. J Perinatol. 2016;36:30–34.
USDA ERS—Urban Influence Codes. https://www.ers.usda.gov/data-products/urban-influence-codes/. Accessed 15 Feb 2021.
Interrante J, Carroll C, Handley S, Kozhimannil K. An enhanced method for identifying hospital-based obstetric unit status. 2021. https://3pea7g1qp8f3t9ooe3z3npx1-wpengine.netdna-ssl.com/wp-content/uploads/2022/01/UMN-OB-Unit-Identification-Methods_7.pdf.
How does CDC identify severe maternal morbidity? | CDC. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm. Accessed 7 Sept 2021.
California Maternal Quality Care Collaborative. NQF # 716: Unexpected newborn complications update (aka Healthy Term Newborn) summary of measure updates. March 2013.
Interrante JD, Tuttle MS, Basile Ibrahim B, Admon LK, Kozhimannil KB. Policy brief: state and regional differences in access to hospital-based obstetric services for rural residents, 2018. https://3pea7g1qp8f3t9ooe3z3npx1-wpengine.netdna-ssl.com/wp-content/uploads/2021/09/UMN-State-Regional-Differences-in-OB_Policy-Brief_8.16.21_508.pdf. Accessed August 2021.
Handley SC, Passarella M, Srinivas SK, Lorch SA. Identifying individual hospital levels of maternal care using administrative data. BMC Health Serv Res. 2021;21:1–11.
Srinivas SK, Kozhimannil K, Hung P, Attanasio L, Jou J, Grobman WA. Do hospitals with a higher level of maternal care designation have better maternal outcomes? Am J Perinatol. 2019;36:653–8.
Vanderlaan J, Rochat R, Williams B, Dunlop A, Shapiro SE. Maternal health associations between hospital maternal service level and delivery outcomes. Women’s Heal Issues. 2019;29:252–8.
Declercq ER, Sakala C, Corry MP, Applebaum S, Herrlich A. Major survey findings of listening to mothers III: pregnancy and birth. J Perinat Educ. 2014;23:9.
Hansen AC, Slavova S, O’Brien JM. Rural residency as a risk factor for severe maternal morbidity. J Rural Health. 2022;38:161–70.
Cameron NA, Molsberry R, Pierce JB, Perak AM, Grobman WA, Allen NB, et al. Pre-pregnancy hypertension among women in rural and urban areas of the United States. J Am Coll Cardiol. 2020;76:2611–9.
Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK. Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health Aff. 2019;38:2077–85.
Saint Onge JM, Smith S. Demographics in rural populations. Surg Clin N. Am. 2020;100:823–33.
Probst J, Eberth JM, Crouch E. Structural urbanism contributes to poorer health outcomes for rural America. Health Aff. 2019;38:1976–84.
Clapp MA, Srinivas SK, Kozhimannil KB, Grobman WA, Kaimal AJ. Comparison of maternal and neonatal subspecialty care provision by hospital. Am J Perinatol. 2021. https://doi.org/10.1055/s-0041-1727223
Kozhimannil KB, Henning-Smith C. Improving health among rural residents in the US. JAMA 2021;325:1033–4.
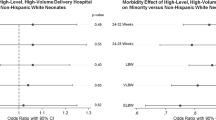
Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and hispanic very preterm infants among New York City Hospitals. JAMA Pediatr. 2018;172:269–77.
Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID multinational cohort study. JAMA Pediatr. 2021;175:817–26.
Handley SC, Srinivas SK, Lorch SA. Regionalization of care and the maternal-infant dyad disconnect. JAMA. 2019;322:503–4.
Brantley MD, Davis NL, Goodman DA, Callaghan WM, Barfield WD. Perinatal regionalization: a geospatial view of perinatal critical care, United States, 2010-2013. Am J Obstet Gynecol. 2017;216:185.e1–185.e10.
DeSisto CL, Okoroh EM, Kroelinger CD, Barfield WD. Summary of neonatal and maternal transport and reimbursement policies—a 5-year update. J Perinatol. 2022. https://doi.org/10.1038/s41372-022-01389-3.
Author information
Authors and Affiliations
Contributions
SCH conceptualized and designed the study, interpreted the data, and drafted the manuscript. MP completed the data analysis, interpreted the data, and critically revised the manuscript. JDI interpreted the data and critically revised the manuscript. KBK participated in the design of the study, interpretation of the data, and critically revised the manuscript. SAL contributed to study conceptualization, interpretation of the data, and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Handley, S.C., Passarella, M., Interrante, J.D. et al. Perinatal outcomes for rural obstetric patients and neonates in rural-located and metropolitan-located hospitals. J Perinatol 42, 1600–1606 (2022). https://doi.org/10.1038/s41372-022-01490-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01490-7