Abstract
Objective
To describe variation in mortality and morbidity effects of high-level, high-volume delivery hospital between racial/ethnic groups and insurance groups.
Study Design
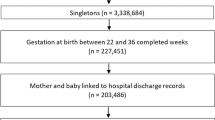
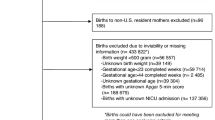
Retrospective cohort including infants born at 24–32 weeks gestation or birth weights ≤2500 g in California, Missouri, and Pennsylvania between 1995 and 2009 (n = 636,764). Multivariable logistic random-effects models determined differential effects of birth hospital level/volume on mortality and morbidity through an interaction term between delivery hospital level/volume and either maternal race or insurance status.
Result
Compared to non-Hispanic white neonates, odds of complications of prematurity were 14–25% lower for minority infants in all gestational age and birth weight cohorts delivering at high-level, high-volume centers (odds ratio (ORs) 0.75–0.86, p < 0.001–0.005). Effect size was greatest for Hispanic infants. No difference was noted by insurance status.
Conclusions
Neonates of minority racial/ethnic status derive greater morbidity benefits than non-Hispanic white neonates from delivery at hospitals with high-level, high-volume neonatal intensive care units.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1–54.
Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013;131:855–60. https://doi.org/10.1542/peds.2012-2471.
Institute of Medicine. Preterm birth: causes, consequences, and prevention. Washington, DC: The National Academic Press; 2007.
Yu VYH, Doyle LW. Regionalized long-term follow-up. Semin Neonatol. 2004;9:135–44. https://doi.org/10.1016/j.siny.2003.08.008.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–75. https://doi.org/10.1056/NEJMsa065029.
Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109:745–51.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010;304:992–1000. https://doi.org/10.1001/jama.2010.1226.
Chung JH, Phibbs CS, Boscardin WJ, Kominski GF, Ortega AN, Needleman J. The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care. 2010;48:635–44. https://doi.org/10.1097/MLR.0b013e3181dbe887.
Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8. https://doi.org/10.1542/peds.2011-2820.
Markus AR, Krohe S, Garro N, Gerstein M, Pellegrini C. Examining the association between Medicaid coverage and preterm births using 2010–2013 National Vital Statistics Birth Data. J Child Poverty. 2016;23:79–94. https://doi.org/10.1080/10796126.2016.1254601.
Durbin DR, Giardino AP, Shaw KN, Harris MC, Silber JH. The effect of insurance status on likelihood of neonatal interhospital transfer. Pediatrics. 1997;100:E8.
Howell EA, Janevic T, Herbert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172:269–77. https://doi.org/10.1001/jamapediatrics.2017.4402.
Horbar JD, Edwards EM, Greenberg LT, Profit J, Draper D, Helkey D, et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 2019. https://doi.org/10.1001/jamapediatrics.2019.0241.
Howell EA, Hebert PL, Zeitlin J. Racial segregation and inequality of care in neonatal intensive care units is unacceptable. JAMA Pediatr. 2019. https://doi.org/10.1001/jamapediatrics.2019.0240.
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97. https://doi.org/10.1542/peds.2012-199.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely pretern infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56. https://doi.org/10.1542/peds.2009-2959.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months. JAMA. 2003;289:1124–9. https://doi.org/10.1001/jama.289.9.1124.
Ananth C, Basso O. Impact of pregnancy-induced hypertension on stillbirth and neonatal mortality in first and higher order births: a population-based study. Epidemiology. 2010;21:118–23. https://doi.org/10.1097/EDE.0b013e3181c297af.
Perger L, Mukhopadhyay D, Komidar L, Wiggins-Dohlvik K, Uddin MN, Beeram M. Maternal pre-eclampsia as a risk factor for necrotizing enterocolitis. J Matern-Fetal Neonatal Med. 2016;29:2098–103. https://doi.org/10.3109/14767058.2015.1076386.
Leary P, Leary SE, Stout K, Schwartz S, Easterling TR. Maternal, perinatal, and postnatal outcomes in women with chronic heart disease in Washington State. Obstet Gynecol. 2012;120:1283–90. https://doi.org/10.1097/AOG.0b013e3182733d56.
Kendrick J, Sharma S, Holmen J, Palit S, Nuccio E, Chonchol M. Kidney disease and maternal and fetal outcomes in pregnancy. Am J Kidney Dis. 2015;66:55–59. https://doi.org/10.1053/j.ajkd.2014.11.019.
Nevis I, Reitsma, Dominic A, McDonald S, Thabane L, Aki E, et al. Pregnancy outcomes in women with chronic kidney disease: a systematic review. Clin J Am Soc Nephrol. 2011;6:2587–98. https://doi.org/10.2215/CJN.10841210.
Persson M, Shah PS, Rusconi F, Reichman B, Modi N, Kusuda S, et al. Association of maternal diabetes with neonatal outcomes of very preterm and very low-birth-weight infants: an International Cohort Study. JAMA Pediatr. 2018;172:867–75. https://doi.org/10.1001/jamapediatrics.2018.1811.
Grandi C, Tapia JL, Cardoso VC. Impact of maternal diabetes mellitus on mortality and morbidity of very low birth weight infants: a multicenter Latin America study. J Pediatr. 2015;91:234–41. https://doi.org/10.1016/j.jped.2014.08.007.
Shapiro-Mendoza C, Tomashek K, Kotelchuck M, Barfield W, Nannini JW, Declercq E. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics. 2008;121:e223–32. https://doi.org/10.1542/peds.2006-3629.
Yee W, Soraisham A, Shah V, Aziz K, Yoon W, Lee SK. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–304. https://doi.org/10.1542/peds.2011-2022.
Samuels N, van de Graaf R, de Jonge R, Reiss IK, Vermeulen M. Risk factors for necrotizing enterocolitis in neonates: a systematic review of prognostic studies. BMC Pediatr. 2017;17:105 https://doi.org/10.1186/s12887-017-0847-3.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sanchez PJ, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66. https://doi.org/10.1542/peds.2007-3423.
Fang JL, Sorita A, Carey WA, Colby CE, Murad MH, Alahdab F, et al. Interventions to prevent retinopathy of prematurity: a meta-analysis. Pediatrics. 2016;137 https://doi.org/10.1542/peds.2015-3387.
Trembath A, Laughon M. Predictors of bronchopulmonary dysplasia. Clin Perinatol. 2012;39:585–601. https://doi.org/10.1016/j.clp.2012.06.014.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3. https://doi.org/10.1002/14651858.CD004454.pub2.
Linder N, Haskin O, Levit O, Klinger G, Prince T, Naor N, et al. Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case–control study. Pediatrics. 2003;111(5 Part 1):e590–5.
Chevallier M, Debillon T, Pierrat V, Delorme P, Kayem G, Durox M, et al. Leading causes of preterm delivery as risk factors for intraventricular hemorrhage in very preterm infants: results of the EPIPAGE 2 cohort study. Am J Obstet Gynecol. 2017;216:518.el–518.e12. https://doi.org/10.1016/j.ajog.2017.01.002.
Handley SC, Passarella M, Lee HC, Lorch SA. Incidence trends and risk factor variation in severe intraventricular hemorrhage across a population based cohort. J Pediatr. 2018;200:24–29.e3. https://doi.org/10.1016/j.jpeds.2018.04.020.
Profit J, Gould J, Bennett M, Goldstein BA, Draper D, Phibbs C, et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics. 2017;140. https://doi.org/10.1542/peds.2017-0918.
Jha AK, Orav EJ, Epstein AM. Low-quality, high-cost hospitals, mainly in South, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Aff. 2011;30:1904–11. https://doi.org/10.1377/hlthaff.2011.0027.
Comstock R, Castillo E, Lindsay S. Four-year review of the use of race and ethnicity in epidemiologic and public health research. Am J Epidemiol. 2004;159:611–9.
Burchard EG, Ziv E, Coyle N, Gomez SL, Tang H, Karter AJ. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348:1170–5. https://doi.org/10.1056/NEJMsb025007.
Baker LC, Afendulis CC, McConville S, Phibbs CS, Fuentes-Afflick E. Differences in neonatal motality among whites and Asian American subgroups: evidence from California. Arch Pediatr Adolesc Med. 2007;161:69–76. https://doi.org/10.1001/archpedi.161.1.69.
Rice WS, Goldfarb SS, Brisendine AE, Burrows S, Wingate MS. Disparities in infant mortality by race among Hispanic and non-Hispanic infants. Matern Child Health J. 2017;21:1581–8. https://doi.org/10.1007/s10995-017-2290-3.
Funding
This work was supported by a grant R01 HD084819.
Author information
Authors and Affiliations
Contributions
SL obtained data for the project. GY and SL both contributed to idea development, project design, data analysis, and manuscript writing and editing. MP prepared data and assisted with data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yannekis, G., Passarella, M. & Lorch, S. Differential effects of delivery hospital on mortality and morbidity in minority premature and low birth weight neonates. J Perinatol 40, 404–411 (2020). https://doi.org/10.1038/s41372-019-0423-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0423-9
This article is cited by
-
The impact of volume and neonatal level of care on outcomes of moderate and late preterm infants
Journal of Perinatology (2024)