Abstract
Objective
We aimed to evaluate abnormal magnetic resonance imaging (MRI) findings in neonates with mild hypoxic-ischemic encephalopathy (HIE).
Study design
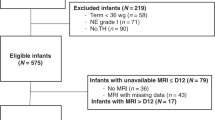
This was a single-center, retrospective study of mild HIE conducted from 2011 to 2020. Almost all neonates with mild HIE received management targeted to a temperature of 36 ± 0.5°C for 72 h and underwent MRI (135 of 145). We evaluated medical records and assessed amplitude-integrated electroencephalography (aEEG).
Result
All participants survived until discharge. Abnormal MRI findings were present in 23/135 (17%) neonates. The normal versus abnormal MRI-finding groups had similar characteristics, except discontinuous aEEG patterns (p = 0.002) and inotropic drugs (p = 0.035). Regression analyses showed discontinuous aEEG patterns (odds ratio = 19.3, 95% confidence interval=1.88–197, p = 0.013) being associated with higher odds of abnormal MRI findings.
Conclusion
Our study suggests that a discontinuous aEEG pattern is associated with abnormal MRI findings and can be used to discuss the definition of mild HIE.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author, T. I., upon reasonable request.
References
Robertson C, Finer N. Term infants with hypoxic-ischemic encephalopathy: outcome at 3.5 years. Dev Med Child Neurol. 1985;27:473–84. https://doi.org/10.1111/j.1469-8749.1985.tb04571.x
Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976;33:696–705. https://doi.org/10.1001/archneur.1976.00500100030012
van de Riet JE, Vandenbussche FP, Le Cessie S, Keirse MJ. Newborn assessment and long-term adverse outcome: a systematic review. Am J Obstet Gynecol. 1999;180:1024–9. https://doi.org/10.1016/s0002-9378(99)70676-9
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013;1:CD003311 https://doi.org/10.1002/14651858.CD003311.pub3
Tagin MA, Woolcott CG, Vincer MJ, Whyte RK, Stinson DA. Hypothermia for neonatal hypoxic ischemic encephalopathy: an updated systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2012;166:558–66. https://doi.org/10.1001/archpediatrics.2011.1772
Shah PS. Hypothermia: a systematic review and meta-analysis of clinical trials. Semin Fetal Neonatal Med. 2010;15:238–46. https://doi.org/10.1016/j.siny.2010.02.003
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl J Med. 2005;353:1574–84. https://doi.org/10.1056/NEJMcps050929
Finer NN, Robertson CM, Peters KL, Coward JH. Factors affecting outcome in hypoxic-ischemic encephalopathy in term infants. Am J Dis Child. 1983;137:21–25. https://doi.org/10.1001/archpedi.1983.02140270017006
Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, et al. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:692–700. https://doi.org/10.1001/archpediatrics.2011.43
Zhou WH, Cheng GQ, Shao XM, Liu XZ, Shan RB, Zhuang DY, et al. Selective head cooling with mild systemic hypothermia after neonatal hypoxic-ischemic encephalopathy: a multicenter randomized controlled trial in China. J Pediatr. 2010;157:367–72. 372.e1–372.e3 https://doi.org/10.1016/j.jpeds.2010.03.030.
Lally PJ, Price DL, Pauliah SS, Bainbridge A, Kurien J, Sivasamy N, et al. Neonatal encephalopathic cerebral injury in South India assessed by perinatal magnetic resonance biomarkers and early childhood neurodevelopmental outcome. PLOS ONE. 2014;9:e87874 https://doi.org/10.1371/journal.pone.0087874. Erratum in: PLoS One; 9: e87874. (Pan-Massachusetts Challenge, ID, 2014) p 24505327
Murray DM, O’Connor CM, Ryan CA, Korotchikova I, Boylan GB. Early EEG grade and outcome at 5 years After mild neonatal hypoxic ischemic encephalopathy. Pediatrics. 2016;138:e20160659 https://doi.org/10.1542/peds.2016-0659
Lodygensky GA, Battin MR, Gunn AJ. Mild Neonatal Encephalopathy-How, When, and How Much to Treat? JAMA Pediatr. 2018;172:3–4. https://doi.org/10.1001/jamapediatrics.2017.3044. PMID: 29114743
Reiss J, Sinha M, Gold J, Bykowski J, Lawrence SM. Outcomes of infants with mild hypoxic ischemic encephalopathy who did not receive therapeutic hypothermia. Biomed Hub. 2019;4:1–9. https://doi.org/10.1159/000502936
Chalak LF, Nguyen KA, Prempunpong C, Heyne R, Thayyil S, Shankaran S, et al. Prospective research in infants with mild encephalopathy identified in the first six hours of life: neurodevelopmental outcomes at 18–22 months. Pediatr Res. 2018;84:861–8. https://doi.org/10.1038/s41390-018-0174-x
Montaldo P, Lally PJ, Oliveira V, Swamy R, Mendoza J, Atreja G, et al. Therapeutic hypothermia initiated within 6 h of birth is associated with reduced brain injury on MR biomarkers in mild hypoxic-ischaemic encephalopathy: a non-randomised cohort study. Arch Dis Child Fetal Neonatal Ed. 2019;104:F515–F520. https://doi.org/10.1136/archdischild-2018-316040
Rao R, Trivedi S, Distler A, Liao S, Vesoulis Z, Smyser C, et al. Neurodevelopmental outcomes in neonates with mild hypoxic ischemic encephalopathy treated with therapeutic hypothermia. Am J Perinatol. 2019;36:1337–43. https://doi.org/10.1055/s-0038-1676973
Saw CL, Rakshasbhuvankar A, Rao S, Bulsara M, Patole S. Current practice of therapeutic hypothermia for mild hypoxic ischemic encephalopathy. J Child Neurol. 2019;34:402–9. https://doi.org/10.1177/0883073819828625
Takenouchi T, Iwata O, Nabetani M, Tamura M. Therapeutic hypothermia for neonatal encephalopathy: JSPNM & MHLW Japan Working Group Practice Guidelines Consensus Statement from the Working Group on Therapeutic Hypothermia for Neonatal encephalopathy, Ministry of Health, Labor and Welfare (MHLW), Japan, and Japan Society for Perinatal and Neonatal Medicine (JSPNM). Brain Dev. 2012;34:165–70. https://doi.org/10.1016/j.braindev.2011.06.009
Hellström-Westas L, Rosén I LS, de Vries LS, Greisen G. Amplitude-integrated EEG classification and interpretation in preterm and term infants. NeoReviews. 2006;7:e76–e87. https://doi.org/10.1542/neo.7-2-e76
Barkovich AJ, Hajnal BL, Vigneron D, Sola A, Partridge JC, Allen F, et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR Am J Neuroradiol. 1998;19:143–9.
Rutherford M, Ramenghi LA, Edwards AD, Brocklehurst P, Halliday H, Levene M, et al. Assessment of brain tissue injury after moderate hypothermia in neonates with hypoxic-ischaemic encephalopathy: a nested substudy of a randomised controlled trial. Lancet Neurol. 2010;9:39–45. https://doi.org/10.1016/S1474-4422(09)70295-9
Shankaran S, Barnes PD, Hintz SR, Laptook AR, Zaterka-Baxter KM, McDonald SA, et al. Brain injury following trial of hypothermia for neonatal hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 2012;97:F398–F404. https://doi.org/10.1136/archdischild-2011-301524. Erratum in: Dis Child A. 23080477, PMC 3722585. Fetal Neonatal; 99 PMID (ed.). (Pan-Massachusetts Challenge, ID, 2014): 301
Swarte R, Lequin M, Cherian P, Zecic A, van Goudoever J, Govaert P. Imaging patterns of brain injury in term-birth asphyxia. Acta Paediatr. 2009;98:586–92. https://doi.org/10.1111/j.1651-2227.2008.01156.x
Society for the Kyoto Scale of Psychological Development Test Shinpan KS (Eds). Kensahou H (Nakanishiya Shuppan, Kyoto, Japan, 2008) p 2001 nenban [the Kyoto Scale of psychological development test 2001].
Wechsler D WPPSI-III- Administration and Scoring Manual. (The Psychological Corporation, Tokyo, Japan, 2003).
Wechsler D WISC-IV- Administration and Scoring Manual. (The Psychological Corporation, Tokyo, Japan, 2003).
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244. Epub 2012 Dec 3
Mercuri E, Ricci D, Cowan FM, Lessing D, Frisone MF, Haataja L, et al. Head growth in infants with hypoxic-ischemic encephalopathy: correlation with neonatal magnetic resonance imaging. Pediatrics. 2000;106:235–43. https://doi.org/10.1542/peds.106.2.235
van Kooij BJ, van Handel M, Nievelstein RA, Groenendaal F, Jongmans MJ, de Vries LS. Serial MRI and neurodevelopmental outcome in 9- to 10-year-old children with neonatal encephalopathy. J Pediatr. 2010;157:221–227.e2. https://doi.org/10.1016/j.jpeds.2010.02.016
DuPont TL, Chalak LF, Morriss MC, Burchfield PJ, Christie L, Sánchez PJ. Short-term outcomes of newborns with perinatal acidemia who are not eligible for systemic hypothermia therapy. J Pediatr. 2013;162:35–41. https://doi.org/10.1016/j.jpeds.2012.06.042
Prempunpong C, Chalak LF, Garfinkle J, Shah B, Kalra V, Rollins N, et al. Prospective research on infants with mild encephalopathy: the PRIME study. J Perinatol. 2018;38:80–85. https://doi.org/10.1038/jp.2017.164. Epub 2017 Nov 2
Walsh BH, Inder TE. MRI as a biomarker for mild neonatal encephalopathy. Early Hum Dev. 2018;120:75–79. https://doi.org/10.1016/j.earlhumdev.2018.02.006
Miller SP, Ramaswamy V, Michelson D, Barkovich AJ, Holshouser B, Wycliffe N. et al. Patterns of brain injury in term neonatalencephalopathy. J Pediatr.2005;146:453–60. https://doi.org/10.1016/j.jpeds.2004.12.026.].
Machie M, Weeke L, de Vries LS, Rollins N, Brown L, Chalak L. MRI score ability to detect abnormalities in mild hypoxic-ischemic encephalopathy. Pediatr Neurol. 2021;116:32–38. https://doi.org/10.1016/j.pediatrneurol.2020.11.015. Epub 2020 Nov 28
Goswami IR, Whyte H, Wintermark P, Mohammad K, Shivananda S, Louis D, et al. Characteristics and short-term outcomes of neonates with mild hypoxic-ischemic encephalopathy treated with hypothermia. J Perinatol. 2020;40:275–83. https://doi.org/10.1038/s41372-019-0551-2
Massaro AN, Murthy K, Zaniletti I, Cook N, DiGeronimo R, Dizon M, et al. Short-term outcomes after perinatal hypoxic ischemic encephalopathy: a report from the Children’s Hospitals Neonatal Consortium HIE focus group. J Perinatol. 2015;35:290–6. https://doi.org/10.1038/jp.2014.190
Gagne-Loranger M, Sheppard M, Ali N, Saint-Martin C, Wintermark P. Newborns referred for therapeutic hypothermia: association between initial degree of encephalopathy and severity of brain injury (what About the newborns with mild encephalopathy on admission?). Am J Perinatol. 2016;33:195–202. https://doi.org/10.1055/s-0035-1563712
Lally PJ, Montaldo P, Oliveira V, Swamy RS, Soe A, Shankaran S, et al. Residual brain injury after early discontinuation of cooling therapy in mild neonatal encephalopathy. Arch Dis Child Fetal Neonatal Ed. 2018;103:F383–F387. https://doi.org/10.1136/archdischild-2017-313321
Walsh BH, Neil J, Morey J, Yang E, Silvera MV, Inder TE, et al. The frequency and severity of magnetic resonance imaging abnormalities in infants with mild neonatal encephalopathy. J Pediatr. 2017;187:26–33.e1. https://doi.org/10.1016/j.jpeds.2017.03.065. Epub 2017 May 4
Rao R, Mietzsch U, DiGeronimo R, Hamrick SE, Dizon MLV, Lee KS, et al. Utilization of therapeutic hypothermia and neurological injury in neonates with mild hypoxic-ischemic encephalopathy: A report from Children’s Hospital neonatal Consortium. Am J Perinatol. 2022;39:319–28. https://doi.org/10.1055/s-0040-1716341
Johnson NJ, Danielson KR, Counts CR, Ruark K, Scruggs S, Hough CL, et al. Targeted temperature management at 33 Versus 36 degrees: A retrospective cohort study. Crit Care Med. 2020;48:362–9. https://doi.org/10.1097/CCM.0000000000004159
Hellström-Westas L, Rosén I, Svenningsen NW. Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch Dis Child Fetal Neonatal Ed. 1995;72:F34–F38. https://doi.org/10.1136/fn.72.1.f34
Toet MC, Hellström-Westas L, Groenendaal F, Eken P, de Vries LS. Amplitude integrated EEG 3 and 6 h after birth in full term neonates with hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 1999;81:F19–F23. https://doi.org/10.1136/fn.81.1.f19
Selvanathan T, Miller SP. Early EEG in neonates with mild hypoxic-ischemic encephalopathy: more than meets the eye. Pediatr Res. 2021;90:18–19. https://doi.org/10.1038/s41390-021-01514-6
Conway JM, Walsh BH, Boylan GB, Murray DM. Mild hypoxic ischaemic encephalopathy and long term neurodevelopmental outcome-A systematic review. Early Hum Dev. 2018;120:80–87. https://doi.org/10.1016/j.earlhumdev.2018.02.007
Finder M, Boylan GB, Twomey D, Ahearne C, Murray DM, Hallberg B. Two-year neurodevelopmental outcomes After mild hypoxic ischemic encephalopathy in the era of therapeutic hypothermia. JAMA Pediatr. 2020;174:48–55. https://doi.org/10.1001/jamapediatrics.2019.4011. Erratum in: JAMA Pediatr. (Pan-Massachusetts Challenge, ID, 2020) p 31710357
Chalak LF, Adams-Huet B, Sant’Anna G. A total Sarnat score in mild hypoxic-ischemic encephalopathy can detect infants at higher risk of disability. J Pediatr. 2019;214:217–221.e1. https://doi.org/10.1016/j.jpeds.2019.06.026. Erratum in: J Pediatr 2020; 218: e2
Author information
Authors and Affiliations
Contributions
TI conceptualized the study, and MS and MK devised the methodology. KK provided feedback to refine the methodology and analysis. TI, WS, CK, and MK collected the clinical data. TI drafted the manuscript, and MS reviewed the manuscript and provided critical feedback.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Research Ethics Board of Saitama Children’s Medical Center (approval number: 2021-03-024). Parental consent was not required because of the retrospective nature of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Imanishi, T., Shimizu, M., Sumiya, W. et al. Brain injury following mild hypoxic-ischemic encephalopathy in neonates–Ten-year experience in a tertiary perinatal center. J Perinatol 42, 1630–1636 (2022). https://doi.org/10.1038/s41372-022-01486-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01486-3