Abstract
Background
There are no published guidelines regarding the diagnosis and treatment of ventilator-associated tracheitis (VAT) in the neonatal intensive care unit (NICU). VAT is likely over-diagnosed and over-treated, increasing antibiotic burden and cost.
Local problem
Diagnosis and treatment of VAT were entirely NICU provider dependent.
Methods
Retrospective pre- and post-intervention chart reviews were performed.
Interventions
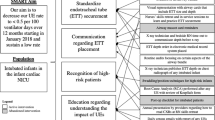
A VAT diagnosis and treatment algorithm was created for use in the care of intubated patients without tracheostomies. 3 plan-do-study-act (PDSA) cycles were used to implement change.
Results
Intubated patients treated for VAT with <25 PMNs on Gram stain decreased from 79% to 35% following the quality improvement (QI) initiative. Treatment of VAT with >7 days of antibiotic therapy decreased from 42% to 10%.
Conclusion
Implementing a QI initiative to improve the diagnosis and treatment of VAT in the NICU decreased the percent of patients treated inappropriately for VAT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
12 December 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41372-022-01574-4
References
Lee PL, Lee WT, Chen HL. Ventilator-Associated Pneumonia in Low Birth Weight Neonates at a Neonatal Intensive Care Unit: A Retrospective Observational Study. Pediatr Neonatol. 2017;58:16–21.
Foglia E, Meier MD, Elward A. Ventilator-associated pneumonia in neonatal and pediatric intensive care unit patients. Clin Microbiol Rev. 2007;20:409–25.
Tamma PD, Turnbull AE, Milstone AM, Lehmann CU, Sydnor ER, Cosgrove SE. Ventilator-associated tracheitis in children: does antibiotic duration matter? Clin Infect Dis. 2011;52:1324–31.
Yu Y, Zhu C, Liu C, Gao Y. How to remove the grey area between ventilator-associated pneumonia and ventilator-associated tracheobronchitis? Crit Care. 2017;21:165.
Network NHS. Pneumonia (Ventilator-associated [VAP] and nonventilator-associated Pneumonia [PNEU]) Event 2021 [Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/6pscvapcurrent.pdf.
Timsit JF, Esaied W, Neuville M, Bouadma L, Mourvllier B. Update on ventilator-associated pneumonia. F1000Res. 2017;6:2061.
Claassen CC, Keenan WJ. Challenging the “Culture” of the Tracheal Aspirate. Neoreviews. 2019;20:e145–e51.
Willson DF, Conaway M, Kelly R, Hendley JO. The lack of specificity of tracheal aspirates in the diagnosis of pulmonary infection in intubated children. Pediatr Crit Care Med. 2014;15:299–305.
Koulenti D, Arvaniti K, Judd M, Lalos N, Tjoeng I, Xu E, et al. Ventilator-Associated Tracheobronchitis: To Treat or Not to Treat? Antibiotics (Basel). 2020;9:51.
Cordero L, Sananes M, Dedhiya P, Ayers LW. Purulence and gram-negative bacilli in tracheal aspirates of mechanically ventilated very low birth weight infants. J Perinatol. 2001;21:376–81.
Slagle TA, Bifano EM, Wolf JW, Gross SJ. Routine endotracheal cultures for the prediction of sepsis in ventilated babies. Arch Dis Child. 1989;64:34–8.
Evans ME, Schaffner W, Federspiel CF, Cotton RB, McKee KT, Stratton CW. Sensitivity, specificity, and predictive value of body surface cultures in a neonatal intensive care unit. JAMA 1988;259:248–52.
Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med. 2000;162:505–11.
Ormsby J, Conrad P, Blumenthal J, Carpenter J, Jones S, Sandora TJ, et al. Practice Improvement for Standardized Evaluation and Management of Acute Tracheitis in Mechanically Ventilated Children. Pediatr Qual Saf. 2021;6:e368.
Langston SJ, Pithia N, Sim MS, Garg M, de St Maurice A, Chu A. Lack of utility of tracheal aspirates in the management of suspected pneumonia in intubated neonates. Infect Control Hosp Epidemiol. 2020;41:660–5.
Yalamanchi S, Saiman L, Zachariah P. Decision-Making Around Positive Tracheal Aspirate Cultures: The Role of Neutrophil Semiquantification in Antibiotic Prescribing. Pediatr Crit Care Med. 2019;20:e380–e5.
Cohen RI. Lean Methodology in Health Care. Chest 2018;154:1448–54.
GJ L, RD M, KM N, TW N, Norman, CL, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Second ed. San Francisco, CA: Jossey-Bass; 2009.
Willson DF, Kirby A, Kicker JS. Respiratory secretion analyses in the evaluation of ventilator-associated pneumonia: a survey of current practice in pediatric critical care. Pediatr Crit Care Med. 2014;15:715–9.
Network NHS. Pediatric Ventilator-Associated Event (PedVAE) 2021 [Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/pedvae-current-508.pdf.
Hickey MK, Miller NC, Haapala J, Demerath EW, Pfister KM, Georgieff MK, et al. Infants exposed to antibiotics after birth have altered recognition memory responses at one month of age. Pediatr Res. 2020;89:1500–07.
Esaiassen E, Fjalstad JW, Juvet LK, van den Anker JN, Klingenberg C. Antibiotic exposure in neonates and early adverse outcomes: a systematic review and meta-analysis. J Antimicrob Chemother. 2017;72:1858–70.
Dias M, Saleem J. Surface colonization and subsequent development of infections with multi drug resistant organisms in a neonatal intensive care unit. Ann Clin Microbiol Antimicrob. 2019;18:12.
Acknowledgements
We would like to thank Ali Anderson, RN for her contribution to improvement ideas, implementation of the QI interventions, and data collection. We would also like to thank our entire multidisciplinary NICU staff for participation in this QI initiative.
Author information
Authors and Affiliations
Contributions
ECI and JDG-V assisted with project design and improvement ideas, participated in the PDSA cycles, designed the data collection instruments, collected data, drafted the initial manuscript, and reviewed and revised the manuscript. JK assisted with project design and improvement ideas, collected data, and reviewed and revised the manuscript. JM and HMA assisted with project design and improvement ideas, collected data, carried out the initial analyses, and reviewed and revised the manuscript. AK and BS assisted with project design and improvement ideas, collected data, and reviewed and revised the manuscript. LN conceptualized and designed the study, supervised data collection, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Figure 1 has been corrected.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ingolfsland, E.C., Gonzalez-Villamizar, J.D., Moore, J. et al. Improving management of ventilator associated tracheitis in a level IV NICU. J Perinatol 42, 1260–1265 (2022). https://doi.org/10.1038/s41372-022-01399-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01399-1