Abstract
Objectives
To compare the pain scores between the two groups, breast milk (BM) and 24% sucrose, in preterm neonates undergoing automated heel lance for the blood draw.
Methods
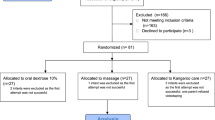
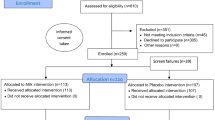
The study is designed as a randomized, single-blinded, non-inferiority trial. Infants born between 30 1/7weeks and 36 6/7 weeks of gestation were randomly assigned to receive either 24% sucrose or expressed BM. The Premature Infant Pain Profile—Revised (PIPP-R) was utilized to provide pain scores.
Results
No differences were noted in the baseline characteristics between the two groups. The quantile regression estimates for PIPP-R scores during the procedure were statistically non-significant at all percentile levels of distribution (50%ile coefficient 0, 95% CI −0.49 to 0.49).
Conclusion
We conclude that BM is not inferior to 24% sucrose in providing analgesia during heel lance in moderate and late preterm infants.
Trial registration
This trial was registered at www.clinicaltrials.gov (identifier NCT04898881)
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Slater R, Cantarella A, Gallella S, Worley A, Boyd S, Meek J, et al. Cortical pain responses in human infants. J Neurosci. 2006;26:3662–6.
Grunau RE, Whitfield MF, Petrie-Thomas J, Synnes AR, Cepeda IL, Keidar A, et al. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain. 2009;143:138–46.
Vinall J, Miller SP, Chau V, Brummelte S, Synnes AR, Grunau RE. Neonatal pain in relation to postnatal growth in infants born very preterm. Pain. 2012;153:1374–81.
Ranger M, Synnes AR, Vinall J, Grunau RE. Internalizing behaviours in school-age children born very preterm are predicted by neonatal pain and morphine exposure. Eur J Pain. 2014;18:844–52.
Grunau RE, Whitfield MF, Petrie J. Children’s judgements about pain at age 8–10 years: do extremely low birthweight (< or = 1000 g) children differ from full birthweight peers? J Child Psychol Psychiatry. 1998;39:587–94.
Taddio A, Shah V, Gilbert-MacLeod C, Katz J. Conditioning and hyperalgesia in newborns exposed to repeated heel lances. JAMA. 2002;288:857–61.
Hall RW, Shbarou RM. Drugs of choice for sedation and analgesia in the neonatal ICU. Clin Perinatol. 2009;36:215–26. vii
Bhalla T, Shepherd E, Tobias JD. Neonatal pain management. Saudi J Anaesth. 2014;8:S89–97.
Hall RW, Kronsberg SS, Barton BA, Kaiser JR, Anand KJ, Group NTI. Morphine, hypotension, and adverse outcomes among preterm neonates: who’s to blame? Secondary results from the NEOPAIN trial. Pediatrics. 2005;115:1351–9.
Hall RW, Anand KJ. Pain management in newborns. Clin Perinatol. 2014;41:895–924.
Committee On F, Newborn, Section On A, Pain M. Prevention and management of procedural pain in the neonate: an update. Pediatrics. 2016;137:e20154271.
Stevens B, Yamada J, Ohlsson A, Haliburton S, Shorkey A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2016;7:CD001069.
Stevens B, Yamada J, Campbell-Yeo M, Gibbins S, Harrison D, Dionne K, et al. The minimally effective dose of sucrose for procedural pain relief in neonates: a randomized controlled trial. BMC Pediatr. 2018;18:85.
Hatfield LA, Chang K, Bittle M, Deluca J, Polomano RC. The analgesic properties of intraoral sucrose: an integrative review. Adv Neonatal Care. 2011;11:83–92. quiz 93-84.
Johnston CC, Filion F, Snider L, Majnemer A, Limperopoulos C, Walker CD, et al. Routine sucrose analgesia during the first week of life in neonates younger than 31 weeks’ postconceptional age. Pediatrics. 2002;110:523–8.
Anseloni VC, Weng HR, Terayama R, Letizia D, Davis BJ, Ren K, et al. Age-dependency of analgesia elicited by intraoral sucrose in acute and persistent pain models. Pain. 2002;97:93–103.
Baudesson de Chanville A, Brevaut-Malaty V, Garbi A, Tosello B, Baumstarck K, Gire C. Analgesic effect of maternal human milk odor on premature neonates: a randomized controlled trial. J Hum Lact. 2017;33:300–8.
Badiee Z, Asghari M, Mohammadizadeh M. The calming effect of maternal breast milk odor on premature infants. Pediatr Neonatol. 2013;54:322–5.
Heine WE. The significance of tryptophan in infant nutrition. Adv Exp Med Biol. 1999;467:705–10.
Barrett T, Kent S, Voudouris N. Does melatonin modulate beta-endorphin, corticosterone, and pain threshold? Life Sci. 2000;66:467–76.
Stevens BJ, Gibbins S, Yamada J, Dionne K, Lee G, Johnston C, et al. The premature infant pain profile-revised (PIPP-R): initial validation and feasibility. Clin J Pain. 2014;30:238–43.
Chen M, Shi X, Chen Y, Cao Z, Cheng R, Xu Y, et al. A prospective study of pain experience in a neonatal intensive care unit of China. Clin J Pain. 2012;28:700–4.
Banga S, Datta V, Rehan HS, Bhakhri BK. Effect of sucrose analgesia, for repeated painful procedures, on short-term neurobehavioral outcome of preterm neonates: a randomized controlled trial. J Trop Pediatr. 2016;62:101–6.
Simonse E, Mulder PG, van Beek RH. Analgesic effect of breast milk versus sucrose for analgesia during heel lance in late preterm infants. Pediatrics. 2012;129:657–63.
Sener Taplak A, Erdem E. A comparison of breast milk and sucrose in reducing neonatal pain during eye exam for retinopathy of prematurity. Breastfeed Med. 2017;12:305–10.
Angeles DM, Boskovic DS, Tan JC, Shih W, Hoch E, Forde D, et al. Oral dextrose reduced procedural pain without altering cellular ATP metabolism in preterm neonates: a prospective randomized trial. J Perinatol. 2020;40:888–95.
Slater R, Cornelissen L, Fabrizi L, Patten D, Yoxen J, Worley A, et al. Oral sucrose as an analgesic drug for procedural pain in newborn infants: a randomised controlled trial. Lancet. 2010;376:1225–32.
Shah PS, Herbozo C, Aliwalas LL, Shah VS. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. 2012;12:CD004950.
Codipietro L, Ceccarelli M, Ponzone A. Breastfeeding or oral sucrose solution in term neonates receiving heel lance: a randomized, controlled trial. Pediatrics. 2008;122:e716–721.
Asmerom Y, Slater L, Boskovic DS, Bahjri K, Holden MS, Phillips R, et al. Oral sucrose for heel lance increases adenosine triphosphate use and oxidative stress in preterm neonates. J Pediatr. 2013;163:29–35 e21.
Angeles DM, Asmerom Y, Boskovic DS, Slater L, Bacot-Carter S, Bahjri K, et al. Oral sucrose for heel lance enhances adenosine triphosphate use in preterm neonates with respiratory distress. SAGE Open Med. 2015;3:2050312115611431.
Tremblay S, Ranger M, Chau CMY, Ellegood J, Lerch JP, Holsti L, et al. Repeated exposure to sucrose for procedural pain in mouse pups leads to long-term widespread brain alterations. Pain. 2017;158:1586–98.
Funding
This work was supported by an institutional grant from Sarnaik Endowment Grant, Detroit Medical Center.
Author information
Authors and Affiliations
Contributions
Concept and Design: PV, MB, CT, FE, MLB, GN, and SJ; Acquisition, analysis, and interpretation of data: PV, FE, CT, SJ, and MB Randomization and treatment allocation: MLB; Statistical analysis: MB, and AF; Drafting of manuscript: PV; Critical revision of manuscript for important intellectual content: FE, CT, SJ, GN, and MB; Obtaining funding: PV and MB; Supervision: MB. PV and MB had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Velumula, P.K., Elbakoush, F., Tabb, C. et al. Breast milk vs 24% sucrose for procedural pain relief in preterm neonates: a non-inferiority randomized controlled trial. J Perinatol 42, 914–919 (2022). https://doi.org/10.1038/s41372-022-01352-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01352-2