Abstract
Objective
To compare sucrose 24% oral gel formulation to liquid formula and breastfeeding during a heel prick in neonates.
Study design
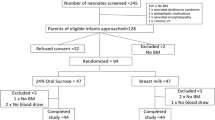
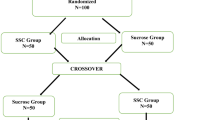
In this comparative effectiveness research 195 neonates >36 weeks’ gestation were randomised to three groups, receiving during heel stick: (i) breastfeeding, (ii) sucrose 24% liquid with non-nutritive sucking and (iii) sucrose 24% gel with non-nutritive sucking. The pain was assessed through the Neonatal Infant Pain Scale.
Results
All the methods analysed has shown to be effective in reducing pain. There was an increase in odds of pain following liquid sucrose compared to breastfeeding (OR = 1.60; 95% CI: 0.82–3.3; p = 0.17). A reduction of odds of pain was showed comparing sucrose to breastfeeding (OR = 0.78; 0.38–1.6; 0.48), and comparing sucrose gel to liquid formula (OR = 0.48; 0.23–0.96; p = 0.04).
Conclusion
Sucrose 24% gel with non-nutritive sucking seems to be a valid alternative when breastfeeding is not possible. Further research is needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Johnston CC, Fernandes AM, Campbell-Yeo M. Pain in neonates is different. Pain. 2011;152(3 Suppl):S65–73.
Vinall J, Grunau RE. Impact of repeated procedural pain-related stress in infants born very preterm. Pediatr Res. 2014;75:584–7.
Valeri BO, Holsti L, Linhares MB. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015;31:355–62.
Meaney MJ, Aitken DH. The effects of early postnatal handling on hippocampal glucocorticoid receptor concentrations: temporal parameters. Brain Res. 1985;354:301–4.
Hatfield LA. Neonatal pain: what’s age got to do with it? Surg Neurol Int. 2014;5(Suppl 13):S479–89.
Anand KJS, Eriksson M, Boyle EM, Avila-Alvarez A, Andersen RD, Sarafidis K, et al. Assessment of continuous pain in newborns admitted to NICUs in 18 European countries. Acta Paediatr. 2017;106:1248–59.
Balice-Bourgois C, Zumstein-Shaha M, Vanoni F, Jaques C, Newman CJ, Simonetti GD. A systematic review of Clinical Practice Guidelines for acute procedural pain on neonates. Clin J Pain. 2020;36:390–8.
Cignacco E, Hamers JP, Stoffel L, van Lingen RA, Gessler P, McDougall J, et al. The efficacy of non-pharmacological interventions in the management of procedural pain in preterm and term neonates. A systematic literature review. Eur J Pain. 2007;11:139–52.
Thakkar P, Arora K, Goyal K, Das RR, Javadekar B, Aiyer S, et al. To evaluate and compare the efficacy of combined sucrose and non-nutritive sucking for analgesia in newborns undergoing minor painful procedure: a randomised controlled trial. J Perinatol. 2016;36:67–70.
Harrison D, Larocque C, Bueno M, Stokes Y, Turner L, Hutton B, et al. Sweet solutions to reduce procedural pain in neonates: a meta-analysis. Pediatrics. 2017;139:e20160955.
Kirpalani H, Truog WE, D’Angio CT, Cotten M. Recent controversies on comparative effectiveness research investigations: challenges, opportunities, and pitfalls. Semin Perinatol. 2016;40:341–7.
Lago P, Garetti E, Pirelli A, Merazzi D, Savant Levet P, Bellieni CV, et al. Linee giuda per la prevenzione ed il trattamento del dolore nel neonato. Ed. Biomedia, pp. 98–102.
Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C. The development of a tool to assess neonatal pain. Neonatal Netw. 1993;12:59–66.
Leite AM, Linhares MB, Lander J, Castral TC, dos Santos CB, Silvan Scochi CG. Effects of breastfeeding on pain relief in full-term newborns. Clin J Pain. 2009;25:827–32.
Shah PS, Herbozo C, Aliwalas LL, Shah VS. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. 2012;12:CD004950.
Zurita-Cruz JN, Rivas-Ruiz R, Gordillo-Álvarez V, Villasis-Keever M. Breastfeeding for acute pain control on infants: a randomised controlled trial. Nutr Hosp. 2017;34:301–7.
Erkul M, Efe E. Efficacy of breastfeeding on babies’ pain during vaccinations. Breastfeed Med. 2017;12:110–5.
Simonse E, Mulder PG, van Beek RH. Analgesic effect of breast milk versus sucrose for analgesia during heel lance in late preterm infants. Pediatrics. 2012;129:657–63.
Baudesson de Chanville A, Brevaut-Malaty V, Garbi A, Tosello B, Baumstarck K, Gire C. Analgesic effect of maternal human milk odor on premature neonates: a randomized controlled trial. J Hum Lact. 2017;33:300–8.
Lima AH, Hermont AP, Friche AA. Analgesia in newborns: a case-control study of the efficacy of nutritive and non-nutritive sucking stimuli. Codas. 2013;25:365–8.
Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–9.
Blass EM, Ciaramitaro V. A new look at some old mechanisms in human newborns: taste and tactile determinants of state, affect, and action. Monogr Soc Res Child Dev. 1994;59:I–V. 1-81
Bellieni CV, Johnston CCAnalgesia. nil or placebo to babies, in trials that test new analgesic treatments for procedural pain. Acta Paediatr. 2016;105:129–36.
Leng HY, Zheng XL, Zhang XH, He HY, Tu GF, Fu Q, et al. Combined non-pharmacological interventions for newborn pain relief in two degrees of pain procedures: a randomised clinical trial. Eur J Pain. 2016;20:989–97.
Fruhstorfer H, Schmelzeisen-Redeker G, Weiss T. Capillary blood sampling: relation between lancet diameter, lancing pain and blood volume. Eur J Pain. 1999;3:283–6.
Acknowledgements
We thank all the members of our Neonatology Division who gave their contribution to this study. We thank Marco Chiera for his scientific help.
Funding
This study did not receive grant.
Author information
Authors and Affiliations
Contributions
IB conceived the study and wrote the initial manuscript. GV, FR, ID and GVZ reviewed and revised the manuscript. CF performed statistical analysis and reviewed the manuscript. VF and GL conceived the study and reviewed the manuscript. All the authors discussed the results, commented on the manuscript and approved it as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bresesti, I., Vanzù, G., Redaelli, F. et al. New perspective for pain control in neonates: a comparative effectiveness research. J Perinatol 41, 2298–2303 (2021). https://doi.org/10.1038/s41372-021-01025-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01025-6