Abstract
Objective
The objective was to investigate maternal and pregnancy characteristics associated with neonatal encephalopathy (NE).
Study design
We queried an administrative birth cohort from California between 2011 and 2017 to determine the association between each factor and NE with and without hypothermia treatment.
Results
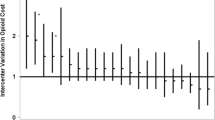
From 3 million infants born at 35 or more weeks of gestation, 6,857 cases of NE were identified (2.3 per 1000 births), 888 (13%) received therapeutic hypothermia. Risk factors for NE were stronger among cases receiving hypothermia therapy. Substance-related diagnosis, preexisting diabetes, preeclampsia, and any maternal infection were associated with a two-fold increase in risk. Maternal overweight/obesity, nulliparity, advanced maternal age, depression, gestational diabetes or hypertension, and short or long gestations also predicted NE. Young maternal age, Asian race and Hispanic ethnicity, and cannabis-related diagnosis lowered risk of NE.
Conclusions
By disseminating these results, we encourage further interrogation of these perinatal factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Neurologic Outcome. 2nd ed. American College of Obstetrics and Gynecologists: Washington, DC, 2019 https://doi.org/10.1097/01.AOG.0000445580.65983.d2.
Kurinczuk JJ, White-Koning M, Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev. 2010;86:329–38.
Badawi N, Kurinczuk JJ, Keogh JM, Alessandri LM, O’Sullivan F, Burton PR, et al. Intrapartum risk factors for newborn encephalopathy: The Western Australian case-control study. BMJ. 1998;317:1554–8.
Molloy EJ, Bearer C. Neonatal encephalopathy versus hypoxic-ischemic encephalopathy. Pediatr Res. 2018; 84: 574.
Aslam S, Strickland T, Molloy EJ. Neonatal encephalopathy: Need for recognition of multiple etiologies for optimal management. Front Pediatr. 2019;7:142.
Volpe JJ. Neonatal encephalopathy: An inadequate term for hypoxic-ischemic encephalopathy. Ann Neurol. 2012;72:156–66.
Martinello K, Hart AR, Yap S, Mitra S, Robertson NJ. Management and investigation of neonatal encephalopathy: 2017 update. Arch Dis Child Fetal Neonatal Ed. 2017;102:F346–F358.
Liljestrom L, Wikstrom AK, Agren J, Jonsson M. Antepartum risk factors for moderate to severe neonatal hypoxic ischemic encephalopathy: A Swedish national cohort study. Acta Obstet Gynecol Scand. 2018;97:615–23.
Blume HK, Li CI, Loch CM, Koepsell TD. Intrapartum fever and chorioamnionitis as risks for encephalopathy in term newborns: A case-control study. Dev Med Child Neurol. 2008;50:19–24.
Blume HK, Loch CM, Li CI. Neonatal encephalopathy and socioeconomic status: population-based case-control study. Arch Pediatr Adolesc Med. 2007;161:663–8.
Martinez-Biarge M, Diez-sebastian J, Wusthoff CJ, Cowan FM. Antepartum and intrapartum factors preceding neonatal hypoxic-ischemic encephalopathy. Pediatrics. 2013; 132. https://doi.org/10.1542/peds.2013-0511.
Tann CJ, Nakakeeto M, Willey BA, Sewegaba M, Webb EL, Oke I, et al. Perinatal risk factors for neonatal encephalopathy: an unmatched case-control study. Arch Dis Child Fetal Neonatal Ed. 2018;103:F250–F256.
Liljestrom L, Wikstrom A-K, Jonsson M. Obstetric emergencies as antecedents to neonatal hypoxic ischemic encephalopathy, does parity matter? Acta Obstet Gynecol Scand. 2018;97:1396–404.
Ellis M, de l Costello AM, Murphy DJ, Badawi N, Kurinczuk JJ, Stanley FJ, et al. Antepartum risk factors for newborn encephalopathy. BMJ 1999;318:1414.
Novak CM, Eke AC, Ozen M, Burd I, Graham EM. Risk Factors for Neonatal Hypoxic-Ischemic Encephalopathy in the Absence of Sentinel Events. Am J Perinatol. 2018;36:27–33.
Parker SJ, Kuzniewicz M, Niki H, Wu YW. Antenatal and intrapartum risk factors for hypoxic-ischemic encephalopathy in a US birth cohort. J Pediatr. 2018;203:163–9.
Lundgren C, Brudin L, Wanby AS, Blomberg M. Ante- and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy. J Matern Neonatal Med. 2018;31:1595–601.
Baer RJ, Rogers EE, Partridge JC, Anderson JG, Morris M, Kuppermann M, et al. Population-based risks of mortality and preterm morbidity by gestational age and birth weight. J Perinatol. 2016;36:1008–13.
Vance GA, Niederhauser A, Chauhan SP, Magann EF, Dahlke JD, Muraskas JK, et al. Does the international classification of disease (ICD-9) code accurately identify neonates who clinically have hypoxic-ischemic encephalopathy? Gynecol Obstet Invest. 2011;71:202–6.
Cnattingius S, Lindam A, Persson M. Risks of asphyxia-related neonatal complications in offspring of mothers with type 1 or type 2 diabetes: the impact of maternal overweight and obesity. Diabetologia. 2017;60:1244–51.
Martinez-Biarge M, Cheong JLY, Diez-Sebastian J, Mercuri E, Dubowitz LMS, Cowan FM. Risk factors for neonatal arterial ischemic stroke: The importance of the intrapartum period. J Pediatr. 2016;173:62–68.e1.
Sells CM, Feske SK. Stroke in pregnancy. Semin Neurol. 2017;37:669–78.
Bandoli G, Palmsten K, Chambers CD, Jelliffe-pawlowski LL, Baer RJ, Thompson CA. Revisiting the Table 2 fallacy: A motivating example examining preeclampsia and preterm birth. Paediatr Perinat Epidemiol. 2018;32:390–7.
Kracer B, Hintz SR, Van Meurs KP, Lee HC. Hypothermia therapy for neonatal hypoxic ischemic encephalopathy in the state of California. J Pediatr. 2014;165:267–73.
Bruun TUJ, Desroches CL, Wilson D, Chau V, Nakagawa T, Yamasaki M, et al. Prospective cohort study for identification of underlying genetic causes in neonatal encephalopathy using whole-exome sequencing. Genet Med. 2018;20:486–94.
Harteman JC, Groenendaal F, Benders MJ, Huisman A, Blom HJ, De Vries LS. Role of thrombophilic factors in full-term infants with neonatal encephalopathy. Pediatr Res. 2013;73:80–86.
Acknowledgements
The authors wish to thank Joe Gleeson, MD for his valuable comments on the project. This analysis was funded by the San Diego Study of Mothers and Infants at the University of California San Diego and the Rady Children’s Institute for Genomic Medicine. Gretchen Bandoli is funded by a NIH award (1 K01 AA027811-01). No funders/sponsors participated in this work.
Author information
Authors and Affiliations
Contributions
Bandoli conceptualized the design and analysis for the study, performed the analysis, drafted and revised the paper. Suttner and Chambers conceptualized the design and analysis for the study, drafted and revised the paper. Kiernan coordinated the literature review, contributed to the drafting and revision of the paper. Baer managed the database for the study, cleaned and prepared data for the analysis, and contributed to the drafting and revision of the paper. Jelliffe-Pawlowski assisted in conceptualizing the parent study, and critically reviewed and revised the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bandoli, G., Suttner, D., Kiernan, E. et al. Risk factors for neonatal encephalopathy in late preterm and term singleton births in a large California birth cohort. J Perinatol 42, 341–347 (2022). https://doi.org/10.1038/s41372-021-01242-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01242-z