Abstract
Background
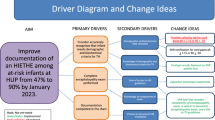
Neonatal encephalopathy (NE) continues to be a significant risk for death and disability. To address this risk, regional guidelines were developed with the support of a malpractice insurance patient safety organization. A NE registry was also established to include 14 centers representing around 50% of deliveries in the state of Massachusetts. The aim of this study was to identify areas of variation in practice that could benefit from quality improvement projects.
Methods
This manuscript reports on the establishment of the registry and the primary findings to date.
Results
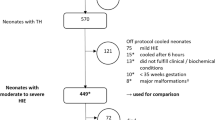
From 2018 to 2020, 502 newborns with NE were evaluated for Therapeutic Hypothermia (TH), of which 246 (49%) received TH, representing a mean of 2.91 per 1000 live births. The study reports on prenatal characteristics, delivery room resuscitation, TH eligibility screening, and post-natal management of newborns with NE who did and did not receive TH.
Conclusions
The registry has allowed for the identification of areas of variation in clinical practices, which have guided ongoing quality improvement projects. The authors advocate for the establishment of local and regional registries to standardize and improve NE patient care. They have made the registry data collection tools freely available for other centers to replicate this work.
Impact
-
Malpractice insurance companies can take an active role in supporting clinicians in establishing clinical practice guidelines and regional registries.
-
Establishing a collaborative regional neonatal encephalopathy (NE) registry is feasible.
-
Data Collection tools for a NE registry have been made publicly available to be adopted and replicated by other groups.
-
Establishing a regional NE registry allowed for the identification of gaps in knowledge, variations in practice, and the opportunity to advance care through quality improvement projects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Keohane, C. A. et al. Partnering with a medical malpractice insurer to improve patient safety and decrease risk. J. Perinat. Neonatal Nurs. 32, 66–71 (2018).
Harris, P. A. et al. Research electronic data capture (Redcap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
Harris, P. A. et al. The Redcap Consortium: building an international community of software platform partners. J. Biomed. Inf. 95, 103208 (2019).
Dwass, M. in Contributions to Probability and Statistics (eds Olkin, I., Ghurye, S. G., Hoeffding, W., Madow, W. G. & Mann, H. B.) 198–202 (Stanford University Press, 1960).
Douglas, C. E. & Michael, F. A. On distribution-free multiple comparisons in the one-way analysis of variance. Commun. Stat. Theory Methods 20, 127–139 (1991).
El-Dib, M. et al. Should therapeutic hypothermia be offered to babies with mild neonatal encephalopathy in the first 6 h after birth? Pediatr. Res. 85, 442–448 (2019).
Walsh, B. H. et al. Comparison of numerical and standard Sarnat grading using the Nichd and Siben methods. J. Perinatol. 42, 328–334 (2021).
Kurinczuk, J. J., White-Koning, M. & Badawi, N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum. Dev. 86, 329–338 (2010).
Hill, M. G., Reed, K. L. & Brown, R. N. Perinatal asphyxia from the obstetric standpoint. Semin. Fetal Neonatal Med. 26, 101259 (2021).
Harteman, J. C. et al. Placental pathology in full-term infants with hypoxic-ischemic neonatal encephalopathy and association with magnetic resonance imaging pattern of brain injury. J. Pediatr. 163, 968.e2–995.e2 (2013).
Mir, I. N. et al. Placental pathology is associated with severity of neonatal encephalopathy and adverse developmental outcomes following hypothermia. Am. J. Obstet. Gynecol. 213, 849.e841–847 (2015).
Penn, A. A. et al. Placental contribution to neonatal encephalopathy. Semin. Fetal Neonatal Med. 26, 101276 (2021).
Espinoza, M. L. et al. Placental pathology as a marker of brain injury in infants with hypoxic ischemic encephalopathy. Early Hum. Dev. 174, 105683 (2022).
Chalak, L. F., Adams-Huet, B. & Sant'Anna, G. A total Sarnat score in mild hypoxic-ischemic encephalopathy can detect infants at higher risk of disability. J. Pediatr. 214, 217.e1–221.e1 (2019).
Sakpichaisakul, K. et al. Blood gas measures as predictors for neonatal encephalopathy severity. J. Perinatol. 41, 2261–2269 (2021).
Chalak, L. et al. Bedside and laboratory neuromonitoring in neonatal encephalopathy. Semin. Fetal Neonatal Med. 26, 101273 (2021).
Lumba, R., Mally, P., Espiritu, M. & Wachtel, E. V. Therapeutic hypothermia during neonatal transport at regional perinatal centers: active vs. passive cooling. J. Perinat. Med. 47, 365–369 (2019).
Stafford, T. D., Hagan, J. L., Sitler, C. G., Fernandes, C. J. & Kaiser, J. R. Therapeutic hypothermia during neonatal transport: active cooling helps reach the target. Ther. Hypothermia Temp. Manag. 7, 88–94 (2017).
Chaudhary, R., Farrer, K., Broster, S., McRitchie, L. & Austin, T. Active versus passive cooling during neonatal transport. Pediatrics 132, 841–846 (2013).
Goel, N., Mohinuddin, S. M., Ratnavel, N., Kempley, S. & Sinha, A. Comparison of passive and servo-controlled active cooling for infants with hypoxic-ischemic encephalopathy during neonatal transfers. Am. J. Perinatol. 34, 19–25 (2017).
Thoresen, M. et al. Time is brain: starting therapeutic hypothermia within three hours after birth improves motor outcome in asphyxiated newborns. Neonatology 104, 228–233 (2013).
Rios, D. R. et al. Hemodynamic optimization for neonates with neonatal encephalopathy caused by a hypoxic ischemic event: physiological and therapeutic considerations. Semin. Fetal Neonatal Med. 26, 101277 (2021).
El-Dib, M., Szakmar, E., Chakkarapani, E. & Aly, H. Challenges in respiratory management during therapeutic hypothermia for neonatal encephalopathy. Semin. Fetal Neonatal Med. 26, 101263 (2021).
Rodd, C., Schwieger-Briel, A. & Hagmann, C. Subcutaneous fat necrosis associated with hypercalcemia in neonates with neonatal encephalopathy treated with therapeutic hypothermia. Semin. Fetal Neonatal Med. 26, 101269 (2021).
Verma, S., Bailey, S. M., Mally, P. V. & Wachtel, E. V. Subcutaneous fat necrosis and hypercalcemia after therapeutic hypothermia in patients with hypoxic-ischemic encephalopathy: a case series. Cureus 10, e3074 (2018).
Castle, V. et al. Frequency and mechanism of neonatal thrombocytopenia. J. Pediatr. 108, 749–755 (1986).
Boutaybi, N. et al. Neonatal thrombocytopenia after perinatal asphyxia treated with hypothermia: a retrospective case control study. Int. J. Pediatr. 2014, 760654 (2014).
Boutaybi, N. et al. Early-onset thrombocytopenia in near-term and term infants with perinatal asphyxia. Vox Sanguinis 106, 361–367 (2014).
Gluckman, P. D. et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 365, 663–670 (2005).
Shankaran, S. et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl. J. Med. 353, 1574–1584 (2005).
Azzopardi, D. V. et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med. 361, 1349–1358 (2009).
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst. Rev. 1, CD003311 (2013).
Del Vecchio, A., Franco, C., Petrillo, F. & D'Amato, G. Neonatal transfusion practice: when do neonates need red blood cells or platelets? Am. J. Perinatol. 33, 1079–1084 (2016).
Clark, S. L., Belfort, M. A., Dildy, G. A. & Meyers, J. A. Reducing obstetric litigation through alterations in practice patterns. Obstet. Gynecol. 112, 1279–1283 (2008).
Bonifacio, S. L. et al. Perinatal events and early magnetic resonance imaging in therapeutic hypothermia. J. Pediatr. 158, 360–365 (2011).
Andreasen, S., Backe, B. & Oian, P. Claims for compensation after alleged birth asphyxia: a nationwide study covering 15 years. Acta Obstet. Gynecol. Scand. 93, 152–158 (2014).
Fanaroff, J. M., Ross, M. G. & Donn, S. M. Medico-legal considerations in the context of neonatal encephalopathy and therapeutic hypothermia. Semin. Fetal Neonatal Med. 26, 101266 (2021).
Acknowledgements
The CRICO Neonatal Encephalopathy Registry included the following: Sara Bates, Mass General Hospital for Children; Ihor Bilyk, North Shore Medical Center; Jason Boulanger, CRICO; Kimberlee Chatson, Cambridge Health Alliance; Sara Cherkerzian, Brigham and Women’s Hospital; Ivana Culic Beverley Hospital; Mohamed El-Dib, Brigham and Women’s Hospital; Hoda El-Shibini; Brigham and Women’s Hospital; Andrew Farkas, Boston Medflight; John Fiascone, South Shore Hospital; Alan Fujii, Good Samaritans Medical Center; Munish Gupta, Beth Israel Medical Center; Anne Hansen, Boston Children’s Hospital; Emily Herzberg, Mass General Hospital for Children; Terrie Inder, Brigham and Women’s Hospital; Janet Lloyd, Mount Auburn Hospital; Marianna Parker, Holy Family Hospital; Silvia Patrizi; Newton Wellesley Hospital; Micheal Prenedergast, Boston Medflight; Janet Soul, Boston Children’s Hospital; Kyoung Young, Saint Elizabeth’s Medical Center.
Funding
This manuscript is supported by The Risk Management Foundation of the Harvard Medical Institutions Incorporated (CRICO).
Author information
Authors and Affiliations
Consortia
Contributions
Substantial contributions to conception and design, drafting the article or revising it critically for important intellectual content, and final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
M.E.-D. discloses he is the PI of an investigator-initiated research funded by Medtronic and served once on an advisory board for Radiometer. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
El-Dib, M., El-Shibiny, H., Walsh, B. et al. Establishing a regional registry for neonatal encephalopathy: impact on identification of gaps in practice. Pediatr Res 95, 213–222 (2024). https://doi.org/10.1038/s41390-023-02763-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02763-3