Abstract
Objectives
To describe and evaluate trends in the etiology and mortality risk in neonates admitted for neonatal intensive care with hydrops fetalis.
Study design
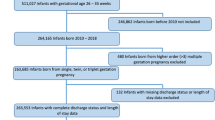
A retrospective review of de-identified patient data in the Pediatrix Clinical Data Warehouse from 1997 to 2018.
Results
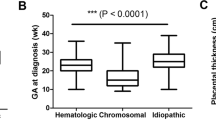
We identified 2144 infants diagnosed with hydrops fetalis. The most common diagnoses were congenital heart disease (n = 325, 15.2%), genetic diagnoses (n = 269, 12.5%) and cardiac arrhythmia (n = 176, 8.2%). Of 2144 neonates, 988 (46%) survived to hospital discharge and 775 (36%) died prior to discharge. Mortality rate was highly variable across diagnoses, ranging from 90% in infants with congenital diaphragmatic hernia to 0% in infants with atrial flutter. Over the study period, more infants were diagnosed with trisomies and fewer with twin-to-twin transfusion. Mortality decreased by 5% from 1997–2007 to 2008–2018.
Conclusions
The risk of death among neonates with hydrops fetalis is highly dependent on the underlying cause, with increasing risk of mortality at lower gestational ages.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Sparks TN, Lianoglou BR, Adami RR, Pluym ID, Holliman K, Duffy J, et al. Exome sequencing for prenatal diagnosis in nonimmune hydrops fetalis. N Engl J Med. 2020;383:1746–1756.
Huang HR, Tsay PK, Chiang MC, Lien R, Chou YH. Prognostic factors and clinical features in liveborn neonates with hydrops fetalis. Am J Perinatol. 2007;24:33–38.
Favre R, Dreux S, Dommergues M, Dumez Y, Luton D, Oury JF, et al. Nonimmune fetal ascites: a series of 79 cases. Am J Obstet Gynecol. 2004;190:407–412.
Bukowski R, Saade GR. Hydrops fetalis. Clin Perinatol. 2000;27:1007–1031.
Chen HY, Zheng JQ, Zhang HP. A case report of Turner syndrome associated with fetal nuchal cystic hygroma and bilateral syndactyly of the hands and feet. Ital J Pediatr. 2019;45:85.
Jomoui W, Tepakhan W, Karnpean R. Strong Linkage of the Single Nucleotide Polymorphism rs77308790 with an α0-Thalassemia (—SEA deletion) Allele and Application for Double-Check Diagnosis of Hb Bart’s Hydrops Fetalis Syndrome in Thailand. Hemoglobin. 2019;43:236–240. https://doi.org/10.1080/03630269.2019.1666720.
Kang Y, Ma Y, Jiang X, Lin X, Zhao F. Fetal giant right cervical cyst causing severe tracheal compression: a case report. Med (Baltim). 2019;98:e16670.
Makhamreh MM, Cottingham N, Ferreira CR, Berger S, Al-Kouatly HB. Nonimmune hydrops fetalis and congenital disorders of glycosylation: A systematic literature review. J Inherit Metab Dis. 2020;43:223–233. https://doi.org/10.1002/jimd.12162.
Mardy AH, Chetty SP, Norton ME, Sparks TN. A system-based approach to the genetic etiologies of non-immune hydrops fetalis. Prenat Diagn. 2019;39:732–750.
McPherson E. Hydrops fetalis in a cohort of 3,137 stillbirths and second trimester miscarriages. Am J Med Genet A. 2019;179:2338–2342. https://doi.org/10.1002/ajmg.a.61340.
Paladini D, Donarini G, Conti A, Constanza De AL, Witte MH, Genesio R, et al. Early fetal hydropic changes are associated with moderate dilatation of the brain ventricular system: a clue to a possible link between cervical lymphatic engorgement and ventricular dilatation? Lymphology. 2019;52:11–17.
Sparks TN, Thao K, Lianoglou BR, Boe NM, Bruce KG, Datkhaeva I, et al. Nonimmune hydrops fetalis: identifying the underlying genetic etiology. Genet Med. 2019;21:1339–1344.
Trainor B, Tubman R. The emerging pattern of hydrops fetalis—incidence, aetiology and management. Ulst Med J. 2006;75:185–186.
Burin MG, Scholz AP, Gus R, Sanseverino MT, Fritsh A, Magalhaes JA, et al. Investigation of lysosomal storage diseases in nonimmune hydrops fetalis. Prenat Diagn. 2004;24:653–657.
Deng Q, Fu F, Yu Q, Li R, Li F, Wang D, et al. Nonimmune hydrops fetalis: Genetic analysis and clinical outcome. Prenat Diagn. 2020;40:803–812.
Kilby MD. Nonimmune Hydrops Fetalis - More Than Meets the Eye? N Engl J Med. 2020;383:1785–1786. https://doi.org/10.1056/NEJMe2029914.
Bruwer Z, Al RN, Al DT, Al MF, Al SA, Al KA, et al. Inborn errors of metabolism in a cohort of pregnancies with non-immune hydrops fetalis: a single center experience. J Perinat Med. 2018;46:968–974.
Brock WW, Bradshaw WT. Congenital chylothorax: a unique presentation of nonimmune hydrops fetalis in a preterm infant. Adv Neonatal Care. 2016;16:114–123.
Calongos G, Hori M, Ogino M, Sawai H. A case of thanatophoric dysplasia type I with fetal hydrops in the first trimester. Case Rep Obstet Gynecol. 2016;2016:1821230.
Singla S, Kumar S, Roy KK, Sharma JB, Kachhawa G. Severe hydrops in the infant of a Rhesus D-positive mother due to anti-c antibodies diagnosed antenatally: a case report. J Med Case Rep. 2010;4:57.
Abrams ME, Meredith KS, Kinnard P, Clark RH. Hydrops fetalis: a retrospective review of cases reported to a large national database and identification of risk factors associated with death. Pediatrics. 2007120:84–9.
Has R. Non-immune hydrops fetalis in the first trimester: a review of 30 cases. Clin Exp Obstet Gynecol. 2001;28:187–190.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tolia, V.N., Hunter Clark, R., Perelmuter, B. et al. Hydrops fetalis—trends in associated diagnoses and mortality from 1997–2018. J Perinatol 41, 2537–2543 (2021). https://doi.org/10.1038/s41372-021-01179-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01179-3