Abstract
Objective
Identify factors associated with the need for pharmacologic therapy (PT) among opioid exposed newborn (OENs).
Study design
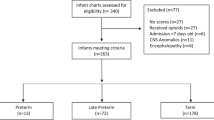
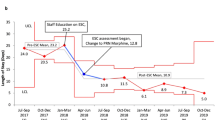
Retrospective analysis of a statewide database of OENs from 2017 through 2019. Multivariable mixed-effects logistic regression modeled the association of maternal characteristics, infant characteristics, and family engagement practices on the receipt of PT.
Results
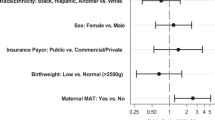
Of 2098 OENs, 44.8% required PT for NOWS. Higher odds of PT were associated with in-utero exposure to medication treatment for opioid use disorder (MOUD) and non-prescribed opioids in addition to MOUD; nicotine, benzodiazepines, SSRIs; male; out-born infants and mother’s ineligibility to provide breast-milk. Lower odds were associated with increasing birth year, skin-to-skin (STS) care, and rooming-in.
Conclusion
Male, out-born infants exposed to MOUD with additional non-prescribed opioids, nicotine, benzodiazepines and SSSRIs with mothers ineligible to provide breast-milk were more likely to require PT, while modifiable care practices including STS care, and rooming-in decreased the likelihood of PT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Prasad MR, Metz TD. Foreword: substance abuse in pregnancy. Clin Obstet Gynecol. 2019;62:110–1.
Rodriguez JJ, Smith VC. Epidemiology of perinatal substance use: exploring trends in maternal substance use. Semin Fetal Neonatal Med. 2019;24:86–9.
Bianchi DW, Gillman MW. Addressing the impact of opioids on women and children. Am J Obstet Gynecol. 2019;221:e1–123.e4.
Strahan AE, Guy GP, Bohm M, Frey M, Ko JY. Neonatal abstinence syndrome incidence and health care costs in the United States. 2016 JAMA Pediatr 2020;174:200–2.
MacMillan KD. Neonatal abstinence syndrome: review of epidemiology, care models, and current understanding of outcomes. Clin Perinatol. 2019;46:817–32.
Grossman M, Berkwitt A. Neonatal abstinence syndrome. Semin Perinatol. 2019;43:173–86.
Hartgrove MJ, Meschke LL, King TL, Saunders C. Treating infants with neonatal abstinence syndrome: an examination of three protocols. J Perinatol. 2019;39:1377–83.
Clemans-Cope L, Holla N, Lee HC, Cong AS, Castro R, Chyi L, et al. Neonatal abstinence syndrome management in California birth hospitals: results of a statewide survey. J Perinatol. 2020;40:463–72.
Mangat AK, Schmölzer GM, Kraft WK. Pharmacological and non-pharmacological treatments for the Neonatal Abstinence Syndrome (NAS). Semin Fetal Neonatal Med. 2019;24:133–41.
Whalen BL, Holmes AV, Blythe S. Models of care for neonatal abstinence syndrome: what works? Semin Fetal Neonatal Med. 2019;24:121–32.
Patrick SW, Barfield WD, Poindexter BB. Committee on fetus and newborn, committee on substance use and prevention. Neonatal Opioid Withdrawal Syndr Pediatrics 2020;146:e2020029074.
Oji-Mmuo CN, Schaefer EW, Liao L, Kaiser JR, Sekhar DL. The possibility of early discharge for newborns being monitored for neonatal abstinence syndrome based on modified finnegan score distributions. Clin Pediatr (Philos). 2019;58:641–6.
Henderson ZT, Ernst K, Simpson KR, Berns S, Suchdev DB, Main E, et al. The National Network of State Perinatal Quality Collaboratives: a growing movement to improve maternal and infant health. J Women’s Health. 2018;27:221–6.
Wachman EM, Houghton M, Melvin P, Isley BC, Murzycki J, Singh R, et al. A quality improvement initiative to implement the eat, sleep, console neonatal opioid withdrawal syndrome care tool in Massachusetts’ PNQIN collaborative. J Perinatol. 2020;40:1560–9.
Kilpatrick SJ, Papile LA, Macones GA. Organization of perinatal healthcare. In Guidelines for Perinatal Care. 8th ed. American Academy of Pediatrics and American College of Obstetrics and Gynecology; 2017. p. 1–36.
Dave CV, Goodin A, Zhu Y, Winterstein A, Wang X, Alrwisan A, et al. Prevalence of maternal‐risk factors related to neonatal abstinence syndrome in a commercial claims database: 2011–2015. Pharmacotherapy 2019;39:1005–11.
Yang JC, Roman-Urrestarazu A, Brayne C. Binge alcohol and substance use across birth cohorts and the global financial crisis in the United State. PLoS ONE. 2018;13:e0199741.
McQueen KA, Murphy-Oikonen J, Desaulniers L. Maternal substance use and neonatal abstinence syndrome: a descriptive study. Matern Child Health J. 2015;19:1756–65.
Bhavsar R, Kushnir A, Kemble N. Incidence and severity of neonatal abstinence syndrome in infants with prenatal exposure to methadone versus buprenorphine. Pediatrics 2018;142:145–5.
Jansson LM, DiPietro JA, Elko A, Williams EL, Milio L, Velez M. Pregnancies exposed to methadone, methadone and other illicit substances, and poly-drugs without methadone: A comparison of fetal neurobehaviours and infant outcomes. Drug Alcohol Depend. 2012;122:213–9.
Opioid use and Opioid use disorder in pregnancy. Committee Opinion No.711. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2017;130:e81–94.
Shen Y, Lo-Ciganic WH, Segal R, Goodin AJ. Prevalence of substance use disorder and psychiatric comorbidity burden among pregnant women with opioid use disorder in a large administrative database, 2009–2014. J Psychosom Obstet Gynaecol. 2020;Feb:1–7.
Nellhaus EM, Nieuwenhuizen L, Egleton R, Hansen Z, Chaffin D, Loudin S, et al. History of postpartum depression as a contributor to the severity of NAS. Addict Behav. 2019;89:78–84.
Mesches GA, Wisner KL, Betcher HK. A Common clinical conundrum: antidepressant treatment of depression in pregnant women. Semin Perinatol. 2020;44:151229.
Hamułka J, Zielińska MA, Chądzyńska K. The combined effects of alcohol and nicotine use during pregnancy on birth outcomes. Rocz Panstw Zakl Hig. 2018;69:45–54.
Parikh A, Gopalakrishnan M, Azeem A, Booth A, El-Metwally D. Racial association and pharmacotherapy in neonatal opioid withdrawal syndrome. J Perinatol. 2019;39:1370–6.
Ramphul K, Mejias SG, Joynauth J. An Update on the burden of neonatal abstinence syndrome in the United States. Hosp Pediatr. 2020;10:181–4.
Howard MB, Schiff DM, Penwill N, Si W, Rai A, Wolfgang T, et al. Impact of parental presence at infants’ bedside on neonatal abstinence syndrome. Hosp Pediatr. 2017;7:63–9.
Singh R, Rothstein R, Ricci K, Visintainer P, Shenberger J, Attwood E, et al. Partnering with parents to improve outcomes for substance exposed newborns—a pilot program. J Perinatol. 2020;40:1041–9.
O’Connor AB, O’Brien L, Alto WA. Are there gender related differences in neonatal abstinence syndrome following exposure to buprenorphine during pregnancy? J Perinat Med. 2013;41:621–3.
Charles MK, Cooper WO, Jansson LM, Dudley J, Slaughter JC, Patrick SW. Male sex associated with increased risk of neonatal abstinence syndrome. Hosp Pediatr. 2017;7:328–34.
Acknowledgements
The authors gratefully acknowledge the contributions of their subjects, and their subjects’ families, as well as those of their colleagues.
Funding
This work has been supported by programmatic funding from Health Policy Commission of Massachusetts.
PNQIN Perinatal Opioid Project Collaborating Hospitals’:
Baystate Medical Center, Springfield, MA, USA; Baystate Franklin Medical Center, Greenfield, MA, USA; Berkshire Medical Center, Pittsfield, MA, USA; Beth Israel Deaconess Medical Center, Boston, MA, USA; Beverly Hospital, Beverly, MA, USA; Boston Medical Center, Boston, MA, USA; Brockton Hospital, Brockton, MA, USA; Cape Cod Hospital, Hyannis, MA, USA; Cooley-Dickenson Hospital, Northampton, MA, USA; Lowell General Hospital, Lowell, MA, USA; Massachusetts General Hospital, Boston, MA, USA; Melrose-Wakefield Hospital, Melrose MA, USA; Mercy Medical Center, Springfield, MA, USA; Southcoast Health, Wareham, MA, USA; South Shore Hospital, South Weymouth, MA, USA; Tufts Medical Center, Boston, MA, USA; UMass Memorial Medical Center, Worcester, MA, USA.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, R., Houghton, M., Melvin, P. et al. Predictors of pharmacologic therapy for neonatal opioid withdrawal syndrome: a retrospective analysis of a statewide database. J Perinatol 41, 1381–1388 (2021). https://doi.org/10.1038/s41372-021-00969-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00969-z
This article is cited by
-
Short term outcomes of neonatal opioid withdrawal syndrome: a comparison of two approaches
Journal of Perinatology (2024)
-
Polygenic risk scores and the need for pharmacotherapy in neonatal abstinence syndrome
Pediatric Research (2023)
-
Association between pharmacologic treatment and hospital utilization at birth among neonatal opioid withdrawal syndrome mother-infant dyads
Journal of Perinatology (2023)