Abstract
Objective
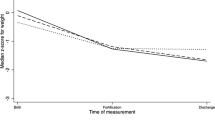
Compare the incidence of severe (grade III/IV) intraventricular hemorrhage (IVH) and/or periventricular leukomalacia (PVL) between two groups of ELBW infants based on diet until 34 weeks corrected gestational age (CGA): (1) Exclusive human milk (EHM)—mother’s own and/or pasteurized donor human milk, human milk-derived fortifier, and oral care with colostrum/human milk vs. (2) non-EHM—bovine formula or mother’s own milk with bovine-derived fortifier.
Study design
Retrospective observational study of two groups of ELBW infants based on diet until 34 weeks CGA.
Result
There were n = 306 infants, 127 EHM and 179 non-EHM. Demographics and morbidities were similar except higher antenatal steroids and NEC in EHM group. The rate of severe IVH/PVL was lower in EHM compared to non-EHM group (7 vs. 18%, p < 0.006).
Conclusion
EHM diet had an independent neuroprotective effect and was associated with decreased incidence of severe IVH/PVL, supporting the need of EHM in ELBW infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2019;7:CD002971. https://doi.org/10.1002/14651858.CD002971.pub5.
Hylander MA, Strobino DM, Pezzullo JC, Dhanireddy R. Association of human milk feedings with a reduction in retinopathy of prematurity among very low birth weight infants. J Perinatol. 2001;21:356–62. https://doi.org/10.1038/sj.jp.7210548.
Patel A, Johnson TJ, Robin B, Bigger HR, Buchanan A, Christian E, et al. Influence of own mother’s milk on bronchopulmonary dysplasia and costs. Arch Dis Child Fetal Neonatal Ed. 2017;102:F256–61. https://doi.org/10.1136/archdischild-2016-310898.
Lechner BE, Vohr BR. Neurodevelopmental outcomes of preterm infants fed human milk: a systematic review. Clin Perinatol. 2017;44:69–83. https://doi.org/10.1016/j.clp.2016.11.004.
Belfort MB. Human milk and preterm infant brain development. Breastfeed Med. 2018;13:S23–5. https://doi.org/10.1089/bfm.2018.29079.mbb.
Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Wright LL, Langer JC, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118:e115–23. https://doi.org/10.1542/peds.2005-2382.
Singhal A, Cole TJ, Lucas A. Early nutrition in preterm infants and later blood pressure: two cohorts after randomised trials. Lancet. 2001;357:413–9. https://doi.org/10.1016/S0140-6736(00)04004-6.
American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–41. https://doi.org/10.1542/peds.2011-3552.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34. https://doi.org/10.1016/s0022-3476(78)80282-0.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56. https://doi.org/10.1542/peds.2009-2959.
Mercier CE, Dunn MS, Ferrelli KR, Howard DB, Soll RF. Vermont Oxford Network ELBW Infant Follow-Up Study Group. neurodevelopmental outcome of extremely low birth weight infants for the Vermont Oxford Network: 1998-2003. Neonatology. 2010;97:329–38. https://doi.org/10.1159/000260136.
Vohr BR, Wright LL, Poole K, McDonald SA. Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks’ gestation between 1993 and 1998. Pediatrics. 2005;116:635–43. https://doi.org/10.1542/peds.2004-2247.
Schindler T, Koller-Smith L, Lui K, Bajuk B, Bolisetty S. Causes of death in very preterm infants cared for in neonatal intensive care units: a population-based retrospective cohort study. BMC Pediatr. 2017;17:59. https://doi.org/10.1186/s12887-017-0810-3.
Imamura T, Ariga H, Kaneko M, Watanabe M, Shibukawa Y, Fukuda Y, et al. Neurodevelopmental outcomes of children with periventricular leukomalacia. Pediatr Neonatol. 2013;54:367–72. https://doi.org/10.1016/j.pedneo.2013.04.006.
Blesa M, Sullivan G, Anblagan D, Telford EJ, Quigley AJ, Sparrow SA, et al. Early breast milk exposure modifies brain connectivity in preterm infants. Neuroimage. 2019;184:431–9. https://doi.org/10.1016/j.neuroimage.2018.09.045.
Ottolini KM, Andescavage N, Kapse K, Jacobs M, Limperopoulos C. Improved brain growth and microstructural development in breast milk-fed very low birth weight premature infants. Acta Paediatr. 2020;109:1580–7. https://doi.org/10.1111/apa.14156.
Keller T, Körber F, Oberthuer A, Schafmeyer L, Mehler K, Kuhr K, et al. Intranasal breast milk for premature infants with severe intraventricular hemorrhage—an observation. Eur J Pediatr. 2019;178:199–206. https://doi.org/10.1007/s00431-018-3279-7.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:1–13. https://doi.org/10.1186/1471-2431-13-59.
Patel AL, Engstrom JL, Meier PP, Kimura RE. Calculating postnatal growth velocity in very low birth weight (VLBW) premature infants. J Perinatol. 2009;29:618–22. https://doi.org/10.1038/jp.2009.55.
Dohare P, Zia MT, Ahmed E, Ahmed A, Yadala V, Schober AL, et al. AMPA-kainate receptor inhibition promotes neurologic recovery in premature rabbits with intraventricular hemorrhage. J Neurosci. 2016;36:3363–77. https://doi.org/10.1523/JNEUROSCI.4329-15.2016.
Kim SE, Ko IG, Shin MS, Kim CJ, Ko YG, Cho H. Neuroprotective effects of bovine colostrum on intracerebral hemorrhage-induced apoptotic neuronal cell death in rats. Neural Reg Res. 2012;7:1715–21. https://doi.org/10.3969/j.issn.1673-5374.2012.22.006.
Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. 2013;60:49–74. https://doi.org/10.1016/j.pcl.2012.10.002.
Gila-Diaz A, Arribas SM, Algara A, Martín-Cabrejas MA, López de Pablo AL, SáenzdePipaón M, et al. A review of bioactive factors in human breastmilk: a focus on prematurity. Nutrients. 2019;11:1307. https://doi.org/10.3390/nu11061307.
Ballabh P, Braun A, Nedergaard M. The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis. 2004;16:1–13. https://doi.org/10.1016/j.nbd.2003.12.016.
Sweeney MD, Ayyadurai S, Zlokovic BV. Pericytes of the neurovascular unit: key functions and signaling pathways. Nat Neurosci. 2016;19:771–83. https://doi.org/10.1038/nn.4288.
Gale SM, Read LC, George-Nascimento C, Wallace JC, Ballard J. Is dietary epidermal growth factor absorbed by premature human infants? Biol Neonate. 1989;55:104–10. https://doi.org/10.1159/000242903.
Liu B, Neufeld AH. Activation of epidermal growth factor receptors in astrocytes: from development to neural injury. J Neurosci Res. 2007;85:3523–9. https://doi.org/10.1002/jnr.21364.
Ballabh P. Intraventricular hemorrhage in premature infants: Mechanism of disease. Pediatr Res. 2010;67:1–8. https://doi.org/10.1203/PDR.0b013e3181c1b176.
Kornblum HI, Hussain R, Wiesen J, Miettinen P, Zurcher SD, Chow K, et al. Abnormal astrocyte development and neuronal death in mice lacking the epidermal growth factor receptor. J Neurosci Res. 1998;53:697–717. 10.1002/(SICI)1097-4547(19980915)53:6<697::AID-JNR8>3.0.CO;2-0.
Vinukonda G, Hu F, Mehdizadeh R, Dohare P, Kidwai A, Juneja A, et al. Epidermal growth factor preserves myelin and promotes astrogliosis after intraventricular hemorrhage. Glia. 2016;64:1987–2004. https://doi.org/10.1002/glia.23037.
Zhou Q, Li M, Wang X, Li Q, Wang T, Zhu Q, et al. Immune-related microRNAs are abundant in breast milk exosomes. Int J Biol Sci 2012;8:118–23. https://doi.org/10.7150/ijbs.8.118.
Alsaweed M, Lai CT, Hartmann PE, Geddes DT, Kakulas F. Human milk miRNAs primarily originate from the mammary gland resulting in unique miRNA profiles of fractionated milk. Sci Rep. 2016;6:20680. https://doi.org/10.1038/srep20680.
Golan-Gerstl R, Elbaum Shiff Y, Moshayoff V, Schecter D, Leshkowitz D, Reif S. Characterization and biological function of milk-derived miRNAs. Mol Nutr Food Res. 2017;61. https://doi.org/10.1002/mnfr.201700009.
Qiu J, Zhou XY, Zhou XG, Cheng R, Liu HY, Li Y. Neuroprotective effects of microRNA-210 on hypoxic-ischemic encephalopathy. Biomed Res Int. 2013;2013:350419. https://doi.org/10.1155/2013/350419.
Xi T, Jin F, Zhu Y, Wang J, Tang L, Wang Y, et al. miR-27a-3p protects against blood-brain barrier disruption and brain injury after intracerebral hemorrhage by targeting endothelial aquaporin-11. J Biol Chem. 2018;293:20041–50. https://doi.org/10.1074/jbc.RA118.001858.
Abrams SA, Landers S, Noble LM, Poindexter BB, Daniels S, Corkins M, et al. Donor human milk for the high-risk infant: preparation, safety, and usage options in the United States. Pediatrics. 2017;139:e20163440. https://doi.org/10.1542/peds.2016-3440.
Ewaschuk JB, Unger S, O’Connor DL, Stone D, Harvey S, Clandinin MT, et al. Effect of pasteurization on selected immune components of donated human breast milk. J Perinatol. 2011;31:593–8. https://doi.org/10.1038/jp.2010.209.
Peila C, Moro GE, Bertino E, Cavallarin L, Giribaldi M, Giuliani F, et al. The effect of holder pasteurization on nutrients and biologically-active components in donor human milk: a review. Nutrients. 2016;8:pii: E477. https://doi.org/10.3390/nu8080477.
Groer M, Duffy A, Morse S, Kane B, Zaritt J, Roberts S, et al. Cytokines, chemokines, and growth factors in banked human donor milk for preterm infants. J Hum Lact. 2014;30:317–23. https://doi.org/10.1177/0890334414527795.
Wei JC, Catalano R, Profit J, Gould JB, Lee HC. Impact of antenatal steroids on intraventricular hemorrhage in very-low-birth-weight infants. J Perinatol. 2016;36:352–6. https://doi.org/10.1038/jp.2016.38.
Chawla S, Natarajan G, Shankaran S, Pappas A, Stoll BJ, Carlo WA, et al. Association of neurodevelopmental outcomes and neonatal morbidities of extremely premature infants with differential exposure to antenatal steroids. JAMA Pediatr. 2016;170:1164–72. https://doi.org/10.1001/jamapediatrics.2016.1936.
Horbar JD, Carpenter JH, Bader GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26. https://doi.org/10.1542/peds.2011-3028.
Garofalo NA, Caplan MS. Oropharyngeal mother’s milk: state of the science and influence on necrotizing enterocolitis. Clin Perinatol. 2019;46:77–88. https://doi.org/10.1016/j.clp.2018.09.005.
Keunen K, van Elburg RM, van Bel F, Benders MJ. Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatr Res. 2015;77:148–55. https://doi.org/10.1038/pr.2014.171.
American Academy of Pediatrics, Committee on Nutrition. Nutritional needs of low-birth-weight infants. Pediatrics. 1985;75:976–86.
Hair AB, Hawthorne KM, Chetta KE, Abrams SA. Human milk feeding supports adequate growth in infants ≤1250 grams birth weight. BMC Res Notes. 2013;13:459. https://doi.org/10.1186/1756-0500-6-459.
Colaizy TT, Carlson S, Saftlas AF, Morriss FH. Growth in VLBW infants fed predominantly fortified maternal and donor human milk diets: a retrospective cohort study. BMC Pediatr. 2012;12:124. https://doi.org/10.1186/1471-2431-12-124.
Brownell EA, Matson AP, Smith KC, Moore JE, Esposito PA, Lussier MM, et al. Dose-response relationship between donor human milk, mother’s own milk, preterm formula, and neonatal growth outcomes. J Pediatr Gastroenterol Nutr. 2018;67:90–6. https://doi.org/10.1097/MPG.0000000000001959.
Neubauer V, Griesmaier E, Pehböck-Walser N, Pupp-Peglow U, Kiechl-Kohlendorf U. Poor postnatal head growth in very preterm infants is associated with impaired neurodevelopment outcome. Acta Paediatr. 2013;102:883–8. https://doi.org/10.1111/apa.12319.
Harsha SS, Archana BR. SNAPPE-II (Score for Neonatal Acute Physiology With Perinatal Extension-II) in predicting mortality and morbidity in the NICU. J Clin Diagn Res. 2015;9:SC10–12. https://doi.org/10.7860/JCDR/2015/14848.6677.
Author information
Authors and Affiliations
Contributions
KC, AR, and BP contributed to the design of the experiment. KC and AR played a role in the acquisition of the data and KC, AR, and BP participated in the data analysis and interpretation. All coauthors played an active role in both the preparation and editing of this manuscript. All authors have read and agreed to the content of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carome, K., Rahman, A. & Parvez, B. Exclusive human milk diet reduces incidence of severe intraventricular hemorrhage in extremely low birth weight infants. J Perinatol 41, 535–543 (2021). https://doi.org/10.1038/s41372-020-00834-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00834-5