Abstract
Objective
To determine the rates of high-risk infant follow-up (HRIF) attendance and the characteristics associated with follow-up among infants with hypoxic–ischemic encephalopathy (HIE) in California.
Study design
Using population-based datasets, 1314 infants with HIE born in 2010–2016 were evaluated. The characteristics associated with follow-up were identified through multivariable logistic regression.
Results
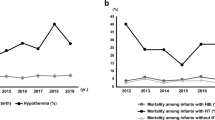
73.9% of infants attended HRIF by age 1. Follow-up rates increased and variation in follow-up by clinic decreased over time. Female infants; those born to African-American, single, less than college-educated, or publicly insured caregivers; and those referred to high-volume or regional programs had lower follow-up rates. In multivariable analysis, Asian and Pacific Islander race/ethnicity had lower odds of follow-up; infants with college- or graduate school-educated caregivers or referred to mid-volume HRIF programs had greater odds.
Conclusion
Sociodemographic and program-level characteristics were associated with lack of follow-up among HIE infants. Understanding these characteristics may improve the post-discharge care of HIE infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013:CD003311. https://doi.org/10.1002/14651858.CD003311.pub3.
Kurinczuk JJ, White-Koning M, Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev. 2010;86:329–38.
Perez A, Ritter S, Brotschi B, Werner H, Caflisch J, Martin E, et al. Long-term neurodevelopmental outcome with hypoxic-ischemic encephalopathy. J Pediatr. 2013;163:454–9.
Pappas A, Shankaran S, McDonald SA, Vohr BR, Hintz SR, Ehrenkranz RA, et al. Cognitive outcomes after neonatal encephalopathy. Pediatrics. 2015;135:e624–34.
Vannucci RC. Current and potentially new management strategies for perinatal hypoxic-ischemic encephalopathy. Pediatrics. 1990;85:961–8.
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009;361:1349–58.
Newborn AAoPCoFa. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Vohr B, Wright LL, Hack M, Aylward G. Follow-up care of high-risk infants. Pediatrics. 2004;114:1377–97.
Ballantyne M, Stevens B, Guttmann A, Willan AR, Rosenbaum P. Maternal and infant predictors of attendance at Neonatal Follow-Up programmes. Child Care Health Dev. 2014;40:250–8.
Harmon SL, Conaway M, Sinkin RA, Blackman JA. Factors associated with neonatal intensive care follow-up appointment compliance. Clin Pediatr (Philos). 2013;52:389–96.
Perenyi A, Katz J, Flom P, Regensberg S, Sklar T. Analysis of compliance, morbidities and outcome in neurodevelopmental follow-up visits in urban African-American infants at environmental risk. J Dev Orig Health Dis. 2010;1:396–402.
Wolke D, Söhne B, Ohrt B, Riegel K. Follow-up of preterm children: important to document dropouts. Lancet. 1995;345:447.
Brady JM, Pouppirt N, Bernbaum J, D’Agostino JA, Gerdes M, Hoffman C, et al. Why do children with severe bronchopulmonary dysplasia not attend neonatal follow-up care? Parental views of barriers. Acta Paediatr. 2018;107:996–1002.
Ballantyne M, Benzies K, Rosenbaum P, Lodha A. Mothers’ and health care providers’ perspectives of the barriers and facilitators to attendance at Canadian neonatal follow-up programs. Child Care Health Dev. 2015;41:722–33.
Hintz SR, Gould JB, Bennett MV, Lu T, Gray EE, Jocson MAL, et al. Factors associated with successful first high-risk infant clinic visit for very low birth weight infants in California. J Pediatr. 2019;210:91–8.e91.
Tin W, Fritz S, Wariyar U, Hey E. Outcome of very preterm birth: children reviewed with ease at 2 years differ from those followed up with difficulty. Arch Dis Child Fetal Neonatal Ed. 1998;79:F83–7.
Callanan C, Doyle L, Rickards A, Kelly E, Ford G, Davis N. Children followed with difficulty: how do they differ? J Paediatr Child Health. 2001;37:152–6.
Mazaubrun C DU, Garel M, Ancel PY, Supernant K, Blondel B, Paris-Petite-Couronne GE. Difficulties with the follow-up of a cohort of very preterm infants: the EPIPAGE Paris-Petite-Couronne population. Arch Pediatr. 2006;13:1202–8.
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet. 2005;365:663–70.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353:1574–84.
Zhou WH, Cheng GQ, Shao XM, Liu XZ, Shan RB, Zhuang DY, et al. Selective head cooling with mild systemic hypothermia after neonatal hypoxic-ischemic encephalopathy: a multicenter randomized controlled trial in China. J Pediatr. 2010;157:367–72.
Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, et al. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:692–700.
Simbruner G, Mittal RA, Rohlmann F, Muche R, Participants nnnT. Systemic hypothermia after neonatal encephalopathy: outcomes of neo.nEURO.network RCT. Pediatrics. 2010;126:e771–8.
Papile LA, Baley JE, Benitz W, Cummings J, Carlo WA, Eichenwald E, et al. Hypothermia and neonatal encephalopathy. Pediatrics. 2014;133:1146–50.
Akula VP, Gould JB, Kan P, Bollman L, Profit J, Lee HC. Characteristics of neonatal transports in California. J Perinatol. 2016;36:1122–7.
Pai VV, Kan P, Bennett M, Carmichael SL, Lee HC, Hintz SR. Improved referral of very low birthweight infants to high-risk infant follow-up in California. J Pediatr. 2019;216:101–8.
Tang BG, Lee HC, Gray EE, Gould JB, Hintz SR. Programmatic and administrative barriers to high-risk infant follow-up care. Am J Perinatol. 2018;35:940–5.
Van Meurs KP, Yan ES, Randall KS, Chock VY, Davis AS, Glennon CS, et al. Development of a NeuroNICU with a broader focus on all newborns at risk of brain injury: the first 2 years. Am J Perinatol. 2018;35:1197–205.
Nehra V, Pici M, Visintainer P, Kase JS. Indicators of compliance for developmental follow-up of infants discharged from a regional NICU. J Perinat Med. 2009;37:677–81.
Funding
This study was supported by grant number F32 HD096778-01 from the National Institutes of Health, awarded to VVP. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
VVP contributed to the conceptualization and design of the study, interpreted the data, and drafted and reviewed the manuscript. PK and TL contributed to the design of the study, analyzed and interpreted the data, and reviewed the manuscript. EEG and MB contributed to the design of the study and reviewed the manuscript. MALJ contributed to the conceptualization of the study and reviewed the manuscript. HCL, SLC, and SRH contributed to the conceptualization and design of the study, analyzed the data, and reviewed and revised the manuscript. All authors approved the final version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pai, V.V., Kan, P., Lu, T. et al. Factors associated with follow-up of infants with hypoxic–ischemic encephalopathy in a high-risk infant clinic in California. J Perinatol 41, 1347–1354 (2021). https://doi.org/10.1038/s41372-020-00898-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00898-3