Abstract
Objectives
To characterize residual vancomycin concentrations (Cmin) and assess the relationships between Cmin, the risk of nephrotoxicity and persistent CoNS sepsis.
Methods
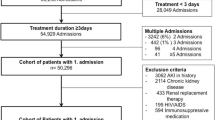
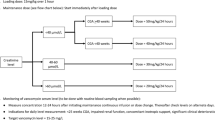
In this 5-year retrospective study among infants treated with vancomycin, the primary outcome was the proportion of those with a steady state Cmin between 10 and 20 mg/L. The secondary outcomes were nephrotoxicity and persistent CoNS sepsis.
Results
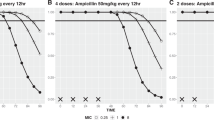
Of 120 infants included, the median first steady state Cmin was 12.4 mg/L and 77 (64%) had a Cmin between 10 and 20 mg/L. Six percent developed nephrotoxicity. This risk was not associated with Cmin. Of the 30 infants with CoNS sepsis, 17 (57%) had persistent bacteremia, and this risk did not correlate significantly with Cmin, CoNS minimal inhibitory concentration (MIC) for vancomycin, or Cmin/MIC.
Conclusions
The majority of infants achieved targeted levels of vancomycin, but persistent bacteremia was common. We did not identify a Cmin threshold associated with nephrotoxicity, nor with microbiological clearance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Clark RH, Bloom BT, Spitzer AlanR, Gerstman DR. Reported medication use in the neonatal intensive care unit: data from a large national data set. Pediatrics. 2006;117:1979–87.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD neonatal research network. Pediatrics. 2002;110:285–91.
Patel SJ, Oshodi A, Prasad P, Delamora P, Larson E, Zaoutis T, et al. Antibiotic use in neonatal intensive care units and adherence with centers for disease control and prevention 12 step campaign to prevent antimicrobial resistance. Pediatr Infect Dis J. 2009;28:1047–51.
Pauwels S, Allegaert K. Therapeutic drug monitoring in neonates. Arch Dis Child. 2016;101:377–81.
Jacqz-Aigrain E, Leroux S, Zhao W, Van Den Anker JN, Sharland M. How to use vancomycin optimally in neonates: remaining questions. Exp Rev Clin Pharm. 2015;8:635–48.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R, Craig W, Billeter M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Heal Pharm. 2009;66:82–98.
Pacifici GM, Allegaert K. Clinical pharmacokinetics of vancomycin in the neonate: a review. Clinics. 2012;67:831–7.
van den Anker JN. Getting the dose of vancomycin right in the neonate. Int J Clin Pharm Ther. 2011;49:247–50.
Moise-Broder PA, Forrest A, Birmingham MC, Schentag JJ. Pharmacodynamics of vancomycin and other antimicrobials in patients with Staphylococcus aureus lower respiratory tract infections. Clin Pharmacokinet. 2004;43:925–42.
Frymoyer A, Hersh AL, El-Komy MH, Gaskari S, Su F, Drover DR, et al. Association between vancomycin trough concentration and area under the concentration–time curve in neonates. Antimicrob Agents Chemother. 2014;58:6454–61.
Bhongsatiern J, Stockmann C, Roberts JK, Yu T, Korgenski KE, Spigarelli MG, et al. Evaluation of vancomycin use in late-onset neonatal sepsis using the area under the concentration-time curve to the minimum inhibitory concentration > 400 target. Ther Drug Monit. 2015;37:756–65.
Kim J, Walker S, Iaboni DC, Walker SE, Elligsen M, Dunn MS, et al. Determination of vancomycin pharmacokinetics in neonates to develop practical initial dosing recommendations. Antimicrob Agents Chemother. 2014;58:2830–40.
Mehrotra N, Tang L, Phelphs S, Meibohm B. Evaluation of vancomycin dosing regimens in preterm and term neonates using Monte Carlo simulations. Pharmacotherapy. 2012;32:408–19.
Ringenberg T, Robinson C, Meyers R, Degnan L, Shah P, Siu A, et al. Achievement of therapeutic vancomycin trough serum concentrations with empiric dosing in neonatal intensive care unit patients. Pediatr Infect Dis J. 2015;34:742–7.
Frymoyer A, Stockmann C, Hersh AL, Goswami S, Keizer RJ. Individualized empiric vancomycin dosing in neonates using a model-based approach. J Pediatr Infect Dis Soc. 2017;00(January):1–8.
Kato H, Hagihara M, Nishiyama N, Koizumi Y, Mikamo H, Matsuura K, et al. Assessment of optimal initial dosing regimen with vancomycin pharmacokinetics model in very low birth weight neonates. J Infect Chemother. 2017;23:154–60.
McNeil JC, Kok EY, Forbes AR, Lamberth L, Hulten KG, Vallejo JG, et al. Healthcare-associated Staphylococcus aureus bacteremia in children evidence for reverse vancomycin creep and impact of vancomycin trough values on outcome. Pediatr Infect Dis J. 2016;35:263–8.
National Healthcare Safety Network (NHSN). Central Line-Associated Bloodstream Infection and non-central line-associated Bloodstream Infection. 2019.
Furuichi M, Miyairi I. Risk factors for persistent bacteremia in infants with catheter-related bloodstream infection due to coagulase-negative Staphylococcus in the neonatal intensive care unit. J Infect Chemother. 2016;22:785–9.
Abbott Laboratories. Architect iVancomycin. 2008;1–7.
Tseng S, Lim CP, Chen Q, Tang CC, Kong ST, Ho PC. Evaluating the relationship between vancomycin trough concentration and 24-hour area under the concentration- time curve in neonates. Antimicrob Agents Chemother. 2018;62:1–11.
De Hoog M, Mouton JW, Van Den Anker JN. Vancomycin: pharmacokinetics and administration regimens in neonates. Clin Pharmacokinet. 2004;43:417–40.
Linder N, Edwards R, MeClead R, Mortensen ME, Walson PKG. Safety of vancomycin with or without gentamicin in neonates. Neonatal Netw. 1993;12:27–30.
Yoo RN, Kim SH, Lee J. Impact of initial vancomycin trough concentration on clinical and microbiological outcomes of methicillin-resistant Staphylococcus aureus bacteremia in children. J Korean Med Sci. 2017;32:22–8.
Wang JL, Lai CH, Lin HH, Chen WF, Shih YC, Hung CH. High vancomycin minimum inhibitory concentrations with heteroresistant vancomycin-intermediate Staphylococcus aureus in meticillin-resistant S. aureus bacteraemia patients. Int J Antimicrob Agents. 2013;42:390–4.
Blanchard AC, Fortin E, Laferrière C, Goyer I, Moussa A, Autmizguine J, et al. Comparative effectiveness of linezolid versus vancomycin as definitive antibiotic therapy for heterogeneously resistant vancomycinintermediate coagulase-negative staphylococcal central-lineassociated bloodstream infections in a neonatal intensive care uni. J Antimicrob Chemother. 2017;72:1812–7.
Le J, Bradley JS, Murray W, Romanowski GL, Tran TT, Nguyen N, et al. Improved vancomycin dosing in children using area under the curve exposure. Pediatr Infect Dis J. 2013;32:e155–63.
Stockmann C, Hersh AL, Roberts JK, Bhongsatiern J, Korgenski EK, Spigarelli MG, et al. Predictive performance of a vancomycin population pharmacokinetic model in neonates. Infect Dis Ther. 2015;4:187–98.
Acknowledgements
We would like to thank sincerely Nadia Desmarais, Dr Caroline Quach, and Dr Nicole Le Saux for their support throughout this project.
Author information
Authors and Affiliations
Contributions
All of the listed authors (IV-T, FT-D, BM, JB, AM, JA) have participated to the conception of this review. IV-T drafted the initial version. Subsequently, all of the co-authors revised the manuscript. All six authors approved the final version of the review. IV-T is the corresponding author and as such, has full access to the data and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Viel-Thériault, I., Martin, B., Thompson-Desormeaux, F. et al. Vancomycin drug monitoring in infants with CoNS sepsis-target attainment, microbiological response and nephrotoxicity. J Perinatol 40, 97–104 (2020). https://doi.org/10.1038/s41372-019-0519-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0519-2
This article is cited by
-
Role of fluid status markers as risk factors for suboptimal vancomycin concentration during continuous infusion in neonates: an observational study
European Journal of Pediatrics (2022)