Abstract
Background
Growing evidence suggests that continuous infusion of vancomycin (CIV) is superior to intermittent infusion of vancomycin (IIV) in neonates. This quality improvement (QI) project aimed to transition from IIV to CIV with earlier and improved attainment of therapeutic vancomycin levels.
Methods
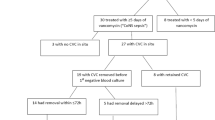
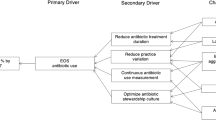
The Model for Improvement framework with Plan Do Study Act cycles was used. Prospective data were collected during three phases: IIV, CIV-1 and CIV-2.
Interventions
A QI team developed a CIV drug monograph and a multidisciplinary education package.
Results
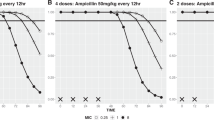
Using IIV, 36% (9/25) of first vancomycin levels were within target range. CIV achieved therapeutic levels twice as quickly as IIV (p < 0.05) with improved first vancomycin target levels (IIV 36%, 9/25; CIV-1 55%, 16/29; CIV-2 61%, 14/23) and total therapeutic levels (IIV 44%, 37/84; CIV-1 56%, 55/98; CIV-2 69%, 79/114).
Conclusions
This QI project demonstrated a successful transition from IIV to CIV with reduced time to achieve target vancomycin and an increased proportion of therapeutic levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Cailes B, Kortsalioudaki C, Buttery J, Pattnayak S, Greenough A, Matthes J, et al. Epidemiology of UK neonatal infections: the neonIN infection surveillance network. Arch Dis Child Fetal Neonatal Ed. 2018;103:F547-F553.
NICE. Neonatal infection (early onset): antibiotics for prevention and treatment. 2012. https://www.nice.org.uk/guidance/CG149.
Dong Y, Speer CP. Late-onset neonatal sepsis: recent developments. Arch Dis Child Fetal Neonatal Ed. 2015;100:F257-63.
De Hoog M, Mouton JW, Van Den Anker JN. Vancomycin: Pharmacokinetics and administration regimens in neonates. Clin Pharmacokinet. 2004;43:417–40.
Moise-Broder PA, Forrest A, Birmingham MC, Schentag JJ. Pharmacodynamics of vancomycin and other antimicrobials in patients with Staphylococcus aureus lower respiratory tract infections. Clin Pharmacokinet. 2004;43:925–42.
British National Formulary for Children. Vancomycin. 2020. https://bnfc.nice.org.uk/drug/vancomycin.html.
Wysocki M, Delatour F, Faurisson F, Rauss A, Pean Y, Misset B, et al. Continuous versus intermittent infusion of vancomycin in severe staphylococcal infections: Prospective multicenter randomized study. Antimicrob Agents Chemother. 2001;45:2460–7.
Cataldo MA, Tacconelli E, Grilli E, Pea F, Petrosillo N. Continuous versus intermittent infusion of vancomycin for the treatment of gram-positive infections: systematic review and meta-analysis. J Antimicrob Chemother. 2012;67:17–24.
Patel AD, Anand D, Lucas C, Thomson AH. Continuous infusion of vancomycin in neonates. Arch Dis Child. 2013;98:478–9.
Gwee A, Cranswick N, McMullan B, Perkins E, Bolisetty S, Gardiner K, et al. Continuous versus intermittent vancomycin infusions in infants: a randomized controlled trial. Pediatrics. 2019;143:e20182179.
Kim J, Walker SAN, Iaboni DC, Walker SE, Elligsen M, Dunn MS, et al. Determination of vancomycin pharmacokinetics in neonates to develop practical initial dosing recommendations. Antimicrob Agents Chemother. 2014;58:2830–40.
Gwee A, Cranswick N, Metz D, Coghlan B, Daley AJ, Bryant PA, et al. Neonatal vancomycin continuous infusion: still a confusion? Pediatr Infect Dis J. 2014;33:600–5.
Ward RM, Allegaert K, De Groot R, Van Den Anker JN. Commentary: continuous infusion of vancomycin in neonates: to use or not to use remains the question. Pediatr Infect Dis J. 2014;33:606–7.
Zhao W, Lopez E, Biran V, Durrmeyer X, Fakhoury M, Jacqz-Aigrain E. Vancomycin continuous infusion in neonates: dosing optimisation and therapeutic drug monitoring. Arch Dis Child. 2013;98:449–53.
Mahieu LM, De Dooy JJ, Lenaerts AE, Ieven MM, De Muynck AO. Catheter manipulations and the risk of catheter-associated bloodstream infection in Neonatal Intensive Care Unit patients. J Hosp Infect. 2001;48:20–6.
Pacifici GM, Allegaert K. Clinical pharmacokinetics of vancomycin in the neonate: a review. Clinics. 2012;67:831–7.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R, Craig W, Billeter M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009;66:82–98.
Rasigade JP, Raulin O, Picaud JC, Tellini C, Bes M, Grando J, et al. Methicillin-resistant Staphylococcus capitis with reduced vancomycin susceptibility causes late-onset sepsis in intensive care neonates. PLoS ONE. 2012;7:e31548.
Butin M, Martins-Simões P, Picaud JC, Kearns A, Claris O, Vandenesch F, et al. Adaptation to vancomycin pressure of multiresistant Staphylococcus capitis NRCS—a involved in neonatal sepsis. J Antimicrob Chemother. 2015;70:3027–31.
Butin M, Martins-Simões P, Rasigade JP, Picaud JC, Laurent F. Worldwide endemicity of a multidrug-resistant Staphylococcus capitis clone involved in neonatal sepsis. Emerg Infect Dis. 2017;23:538–9.
Frymoyer A, Hersh AL, El-Komy MH, Gaskari S, Su F, Drover DR, et al. Association between vancomycin trough concentration and area under the concentration-time curve in neonates. Antimicrob Agents Chemother. 2014;58:6454–61.
University Hospitals of Leicester NHS Trust. The Leicester neonatal service. https://www.leicestershospitals.nhs.uk/aboutus/departments-services/neonatal-service/ (2020).
Acknowledgements
We would like to thank the Clinical Audit Department of University Hospitals of Leicester NHS Trust in their support of this work.
Author information
Authors and Affiliations
Contributions
KFN and SM contributed to the conception of the project. All listed authors contributed to the acquisition of data. AR initially drafted the paper, with KFN subsequently editing. All authors were then involved in revising and final approval of the paper. All authors agree to be accountable for all aspects of the work and its integrity.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This quality improvement project was approved by the UHL Clinical Audit Department. Audit registration number was 10080.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Round, A., Clifton, E., Stachow, L. et al. Continuous infusion of vancomycin improved therapeutic levels in term and preterm infants. J Perinatol 41, 1459–1466 (2021). https://doi.org/10.1038/s41372-020-00909-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00909-3
This article is cited by
-
Optimization of Vancomycin Initial Dose in Term and Preterm Neonates by Machine Learning
Pharmaceutical Research (2022)