Abstract
Objective
The objective is to document changes in the etiologic spectrum of hypertension in premature infants.
Study design
We reviewed all cases of systemic hypertension (HTN) in premature infants at two centers over 8 years. Infants were sorted into categorical groups as described in 2012 by Flynn. Analyses included frequency of diagnosis, timecourse of HTN, and diagnostics. Phthalate exposure via intravenous fluid and respiratory equipment was compared among groups and centers.
Results
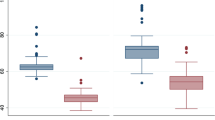
One hundred and twenty-nine infants having 130 episodes of HTN met the inclusion criteria. Sixty-five percent of cases were classified as pulmonary and 16% as miscellaneous. Plasma renin activity (PRA) was undetectable or <11 ng/mL/h in almost all hypertensive infants. Cases categorized as Pulmonary, medications/intoxications, and miscellaneous presented near 40 weeks postmenstrual age, with low PRA and large phthalate exposures.
Conclusions
High PRA HTN has been replaced by low PRA in most cases, and may be due to phthalate exposure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Adelman RD. Neonatal hypertension. Pediatr Clin N Am. 1978;25:99–110.
Neal WA, Reynolds JW, Jarvis CW, Williams HJ. Umbilical artery catheterization: demonstration of arterial thrombosis by aortography. Pediatrics. 1972;50:6–13.
Flynn JT. Neonatal hypertension: diagnosis and management. Pedia Nephrol. 2000;14:332–41.
Batisky DL. Neonatal hypertension. Clin Perinatol. 2014;41:529–42.
Kent AL, Chaudhari T. Determinants of neonatal blood pressure. Curr Hypertens Rep. 2013;15:426–32.
Flynn JT. Hypertension in the neonatal period. Curr Opin Pediatr. 2012;24:197–204.
Friedman AL, Hustead VA. Hypertension in babies following discharge from a neonatal intensive care unit. A 3-year follow-up. Pediatr Nephrol. 1987;1:30–34.
Sahu R, Pannu H, Yu R, Shete S, Bricker JT, Gupta-Malhotra M. Systemic hypertension requiring treatment in the neonatal intensive care unit. J Pediatr. 2013;163:84–88.
Sheftel DN, Hustead V, Friedman A. Hypertension screening in the follow-up of premature infants. Pediatrics. 1983;71:763–6.
Singh HP, Hurley RM, Myers TF. Neonatal hypertension. Incidence and risk factors. Am J Hypertens. 1992;5:51–55.
Jenkins RD, Aziz JK, Gievers LL, Mooers HM, Fino N, Rozansky DJ. Characteristics of hypertension in premature infants with and without chronic lung disease: a long-term multi-center study. Pediatr Nephrol. 2017;32:2115–24.
Jenkins R, Tackitt S, Gievers L, Iragorri S, Sage K, Cornwall T, et al. Phthalate-associated hypertension in premature infants: a prospective mechanistic cohort study. Pediatr Nephrol. 2019;34:1413–24.
Seliem WA, Falk MC, Shadbolt B, Kent AL. Antenatal and postnatal risk factors for neonatal hypertension and infant follow-up. Pediatr Nephrol. 2007;22:2081–7.
Abman SH, Warady BA, Lum GM, Koops BL. Systemic hypertension in infants with bronchopulmonary dysplasia. J Pediatr. 1984;104:928–31.
Alagappan A, Malloy MH. Systemic hypertension in very low-birth weight infants with bronchopulmonary dysplasia: incidence and risk factors. Am J Perinatol. 1998;15:3–8.
Milstein JM, Goetzman BW, Riemenschneider TA, Wennberg RP. Increased systemic vascular resistance in neonates with pulmonary hypertension. Am J Cardiol. 1979;44:1159–62.
Cohen G, Lagercrantz H, Katz-Salamon M. Abnormal circulatory stress responses of preterm graduates. Pediatr Res. 2007;61:329–34.
Casey BJ, Duhoux S, Malter Cohen M. Adolescence: what do transmission, transition, and translation have to do with it? Neuron. 2010;67:749–60.
Greenough A, Emery EF, Gamsu HR. Dexamethasone and hypertension in preterm infants. Eur J Pediatr. 1992;151:134–5.
Al Awad E, Yusuf K, Soraisham A, Obaid H, Sundaram A, Samedi V, et al. Transient hyperaldosteronism and neonatal hypertension: case series and literature review. J Clin Neonatol. 2018;7:185–9.
Stroustrup A, Bragg JB, Busgang SA, Andra SS, Curtin P, Spear EA, et al. Sources of clinically significant neonatal intensive care unit phthalate exposure. J Expo Sci Environ Epidemiol. 2018. https://doi.org/10.1038/s41370-018-0069-2. [Epub ahead of print].
Mallow EB, Fox MA. Phthalates and critically ill neonates: device-related exposures and non-endocrine toxic risks. J Perinatol. 2014;34:892–7.
Loff S, Subotic U, Reinicke F, Wischmann H, Brade J. Extraction of di-ethylhexyl-phthalate from perfusion lines of various material, length and brand by lipid emulsions. J Pediatr Gastroenterol Nutr. 2004;39:341–5.
Weuve J, Sanchez BN, Calafat AM, Schettler T, Green RA, Hu H, et al. Exposure to phthalates in neonatal intensive care unit infants: urinary concentrations of monoesters and oxidative metabolites. Environ Health Perspect. 2006;114:1424–31.
Green R, Hauser R, Calafat AM, Weuve J, Schettler T, Ringer S, et al. Use of di(2-ethylhexyl) phthalate-containing medical products and urinary levels of mono(2-ethylhexyl) phthalate in neonatal intensive care unit infants. Environ Health Perspect. 2005;113:1222–5.
Zhao B, Chu Y, Huang Y, Hardy DO, Lin S, Ge RS. Structure-dependent inhibition of human and rat 11beta-hydroxysteroid dehydrogenase 2 activities by phthalates. Chem Biol Interact. 2010;183:79–84.
Walker BR, Edwards CR. Licorice-induced hypertension and syndromes of apparent mineralocorticoid excess. Endocrinol Metab Clin N Am. 1994;23:359–77.
Starr MC, Flynn JT. Neonatal hypertension: cases, causes, and clinical approach. Pediatr Nephrol. 2019;34:787–99.
Coleman MM, Spear ML, Finkelstein M, Leef KH, Pearlman SA, Chien C, et al. Short-term use of umbilical artery catheters may not be associated with increased risk for thrombosis. Pediatrics. 2004;113:770–4.
McAdams RM, Winter VT, McCurnin DC, Coalson JJ. Complications of umbilical artery catheterization in a model of extreme prematurity. J Perinatol. 2009;29:685–92.
Shahid S, Dutta S, Symington A, Shivananda S, McMaster University N. Standardizing umbilical catheter usage in preterm infants. Pediatrics. 2014;133:e1742–1752.
Chiellini F, Ferri M, Latini G. Physical-chemical assessment of di-(2-ethylhexyl)-phthalate leakage from poly(vinyl chloride) endotracheal tubes after application in high risk newborns. Int J Pharm. 2011;409:57–61.
Latini G, De Felice C, Del Vecchio A, Barducci A, Ferri M, Chiellini F. Di-(2-ethylhexyl)phthalate leakage and color changes in endotracheal tubes after application in high-risk newborns. Neonatology. 2009;95:317–23.
Acknowledgements
The authors acknowledge the assistance of Drs Douglas Leonard, Declan O’Riordan, Scott Snyder, and Robert Schelonka for their support of this research in their neonatal units. The authors also thank Andrew Stout for his editing and proofreading assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farnbach, K., Iragorri, S., Al-Uzri, A. et al. The changing spectrum of hypertension in premature infants. J Perinatol 39, 1528–1534 (2019). https://doi.org/10.1038/s41372-019-0457-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0457-z