Abstract
Objective
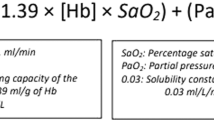
Ischemia followed by reperfusion plays a significant role in the pathogenesis of peri/intraventricular hemorrhage (P/IVH). Delayed cord clamping promotes placental transfusion to newborn and is associated with decreased P/IVH. We hypothesized that extremely low birth weight (ELBW) infants with higher initial hematocrit (Hct) after birth are less likely to develop P/IVH.
Study design
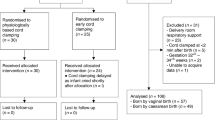
Pre- and postnatal data on inborn ELBW infants over 7 years were reviewed. We examined the relationship between P/IVH in the first week and initial Hct using logistic regression modeling.
Results
We studied 225 infants with a median gestational age (GA) 25.7 (22.4–31.7). Forty-one percent had grade I–IV P/IVH. In univariate analysis, cesarean section (CS) and higher GA, birth weight, 5-minute Apgar, and initial Hct were associated with decreased likelihood of P/IVH while higher maximum PCO2 in first 3 days and use of inotropes/vasopressors, postnatal steroid for hypotension, hypernatremia, transfusion, and use of insulin for hyperglycemia during the first week of life were associated with increased likelihood of P/IVH. In multiple regression analysis, only GA, CS, and initial Hct remained significantly associated with P/IVH. Adjusting for GA and CS, the odds of P/IVH was higher with Hct < 40% (OR 2.04, 95% CI [1.11, 3.76]) and Hct < 45% (2.38 [1.19, 4.76]).
Conclusion
Higher initial Hct is associated with decreased P/IVH. Initial Hct < 45% was associated with a 2-fold increase in P/IVH. We speculate that lower initial Hct represents a lower intravascular volume status and promotes cerebral hypoperfusion preceding P/IVH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Payne AH, Hintz SR, Hibbs AM, Walsh MC, Vohr BR, Bann CM, et al. Neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular–intraventricular hemorrhage. JAMA Pediatr. 2013;167:451–9.
Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M. Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics. 2005;115:997–1003.
Szpecht D, Nowak I, Kwiatkowska P, Szymankiewicz M, Gadzinowski J. Intraventricular hemorrhage in neonates born from 23 to 26 weeks of gestation: retrospective analysis of risk factors. Adv Clin Exp Med. 2017;26:89–94.
Bassan H. Intracranial hemorrhage in the preterm infant: understanding it, preventing it. Clin Perinatol. 2009;36:737–62.
Noori S, McCoy M, Anderson MP, Ramji F, Seri I. Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr. 2014;164:264–70.
Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2000;82:F188–94.
Noori S, Seri I. Hemodynamic antecedents of peri/intraventricular hemorrhage in very preterm neonates. Semin Fetal Neonatal Med. 2015;20:232–7.
Rabe H, Diaz-Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2012;CD003248:https://doi.org/10.1002/14651858.CD003248.pub3.
Tarnow-Mordi W, Morris J, Kirby A, Robledo K, Askie L, Brown R, et al. Delayed versus immediate cord clamping in preterm infants. N Engl J Med. 2017;377:2445–55.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Committee on Obstetric Practice. Committee Opinion No. 684: delayed umbilical cord clamping after birth. Obstet Gynecol. 2017;129:e5–10.
Al-Wassia H, Shah PS. Efficacy and safety of umbilical cord milking at birth: a systematic review and meta-analysis. JAMA Pediatr. 2015;169:18–25.
Linder N, Haskin O, Levit O, Klinger G, Prince T, Naor N, et al. Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case-control study. Pediatrics. 2003;111:e590–5.
Banerjee J, Asamoah FK, Singhvi D, Kwan AW, Morris JK, Aladangady N. Haemoglobin level at birth is associated with short term outcomes and mortality in preterm infants. BMC Med. 2015;13:16.
Hosono S, Mugishima H, Kitamura T, Inami I, Fujita H, Hosono A, et al. Effect of hemoglobin on transfusion and neonatal adaptation in extremely low-birthweight infants. Pediatr Int. 2008;50:306–11.
Koyano K, Kusaka T, Nakamura S, Nakamura M, Konishi Y, Miki T, et al. The effect of blood transfusion on cerebral hemodynamics in preterm infants. Transfusion. 2013;53:1459–67.
Dani C, Pezzati M, Martelli E, Prussi C, Bertini G, Rubaltelli FF. Effect of blood transfusions on cerebral haemodynamics in preterm infants. Acta Paediatr. 2002;91:938–41.
Baenziger O, Stolkin F, Keel M, von Siebenthal K, Fauchere JC, Das Kundu S, et al. The influence of the timing of cord clamping on postnatal cerebral oxygenation in preterm neonates: a randomized, controlled trial. Pediatrics. 2007;119:455–9.
Backes CH, Rivera BK, Haque U, Bridge JA, Smith CV, Hutchon DJ, et al. Placental transfusion strategies in very preterm neonates: a systematic review and meta-analysis. Obstet Gynecol. 2014;124:47–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Dekom, S., Vachhani, A., Patel, K. et al. Initial hematocrit values after birth and peri/intraventricular hemorrhage in extremely low birth weight infants. J Perinatol 38, 1471–1475 (2018). https://doi.org/10.1038/s41372-018-0224-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0224-6
This article is cited by
-
A predictive clinical model for moderate to severe intraventricular hemorrhage in very low birth weight infants
Journal of Perinatology (2022)
-
The impact of initial hematocrit values after birth on peri-/intraventricular hemorrhage in extremely low birth weight neonates
Child's Nervous System (2022)