Abstract
Objectives
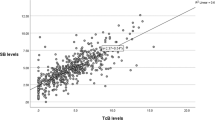
Transcutaneous bilirubin measurements (TcBs) provide a noninvasive method for screening infants for hyperbilirubinemia and have been used extensively in term and late preterm newborns in well baby nurseries, offices, and outpatient clinics. Several studies have also demonstrated the utility of TcBs as a screening tool for infants > 28 weeks’ gestation and their ability to reduce the need for blood sampling. The objectives of this study are to identify how often TcBs are used among California Newborn Intensive Care Units (NICUs) in preterm, late preterm and term infants, and other aspects of jaundice management.
Methods
We conducted a survey on TcB use and practices relating to jaundice management in 150 California NICUs between April and October 2016.
Results
TcB screening is routinely used in 28% (42/150) of NICUs. Only 7% (11/150) of NICUs use TcB in preterm infants < 28 weeks. Practice varied similarly across NICU levels of care. Among the subset of NICUs that responded to questions related to phototherapy and screening practices, prophylactic phototherapy was used in 38% (23/59) and 90% (55/61) screened for glucose-6-phosphate dehydrogenase deficiency based on race, ethnicity, and/or family history.
Conclusion(s)
Despite studies validating the accuracy of TcB in preterm infants > 28 weeks, only 28% of California NICUs routinely use TcB devices. TcB screening in infants < 28 weeks gestation is not widely used and no recommendation can be made in this regard until there is more experience with its application using a standardized protocol in these infants and on a large scale.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Engle WD, Jackson GL, Engle NG. Transcutaneous bilirubinometry. Semin Perinatol. 2014;38:438–51.
Wickremasinghe AC, Karon BS, Saenger AK, Cook WJ. Effect of universal neonatal transcutaneous bilirubin screening on blood draws for bilirubin analysis and phototherapy usage. J Perinatol. 2012;32:851–5.
Quist FK, Bapat R, Kuch-Kunich HK, Ezeanoule K, Keeni S, Thomas R, et al. Clinical utility of transcutaneous bilirubinometer (TcB) in very low birth weight (VLBW) infants. J Perinat Med. 2016;44:933–9.
Wainer S, Parmar SM, Allegro D, Rabi Y, Lyon ME. Impact of a transcutaneous bilirubinometry program on resource utilization and severe hyperbilirubinemia. Pediatrics. 2012;129:77–86.
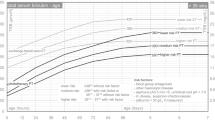
American Academy of Pediatrics Subcommittee on H. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Stark AR, Watchko JF. Hyperbilirubinemia in the newborn infant > or = 35 weeks’ gestation: an update with clarifications. Pediatrics. 2009;124:1193–8.
Maisels MJ, Watchko JF, Bhutani VK, Stevenson DK. An approach to the management of hyperbilirubinemia in the preterm infant less than 35 weeks of gestation. J Perinatol. 2012;32:660–4.
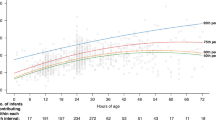
Bhutani VK, Gourley GR, Adler S, Kreamer B, Dalin C, Johnson LH. Noninvasive measurement of total serum bilirubin in a multiracial predischarge newborn population to assess the risk of severe hyperbilirubinemia. Pediatrics. 2000;106:E17.
Rubaltelli FF, Gourley GR, Loskamp N, Modi N, Roth-Kleiner M, Sender A, et al. Transcutaneous bilirubin measurement: a multicenter evaluation of a new device. Pediatrics. 2001;107:1264–71.
Nagar G, Vandermeer B, Campbell S, Kumar M. Reliability of transcutaneous bilirubin devices in preterm infants: a systematic review. Pediatrics. 2013;132:871–81.
Chawla D, Jain S, Kaur G, Sinhmar V, Guglani V. Accuracy of transcutaneous bilirubin measurement in preterm low-birth-weight neonates. Eur J Pediatr. 2014;173:173–9.
Murli L, Thukral A, Sankar MJ, Vishnubhatia S, Deorari AK, Paul VK, et al. Reliability of transcutaneous bilirubinometry from shielded skin in neonates receiving phototherapy: a prospective cohort study. J Perinatol. 2017;37:182–7.
Nagar G, Vandermeer B, Campbell S, Kumar M. Effect of phototherapy on the reliability of transcutaneous bilirubin devices in term and near-term infants: a systematic review and meta-analysis. Neonatology. 2016;109:203–12.
American Academy of Pediatrics Committee on F, Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97.
Maisels MJ, Coffey MP, Kring E. Transcutaneous bilirubin levels in newborns < 35 weeks’ gestation. J Perinatol. 2015;35:739–44.
Rubio A, Epiard C, Gebus M, Deiber M, Samperiz S, Genty C, et al. Diagnosis accuracy of transcutaneous bilirubinometry in very preterm newborns. Neonatology. 2017;111:1–7.
Schmidt ET, Wheeler CA, Jackson GL, Engle WD. Evaluation of transcutaneous bilirubinometry in preterm neonates. J Perinatol. 2009;29:564–9.
Maisels MJ. Transcutaneous bilirubin measurement: does it work in the real world? Pediatrics. 2015;135:364–6.
Acknowledgements
We want to thank all 150 NICU Directors of California for their support. We want to thank CAN (California Association of Neonatologists) for their support in completing the survey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Jeffrey Maisels is a consultant to Draeger Inc (Telford, PA), the supplier of the JM-103 and JM-105 transcutaneous bilirubinometers. The remaining authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Bhatt, D.R., Kristensen-Cabrera, A.I., Lee, H.C. et al. Transcutaneous bilirubinometer use and practices surrounding jaundice in 150 California newborn intensive care units. J Perinatol 38, 1532–1535 (2018). https://doi.org/10.1038/s41372-018-0154-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0154-3
This article is cited by
-
Transcutaneous bilirubin levels in extremely preterm infants less than 30 weeks gestation
Journal of Perinatology (2023)
-
Reliability of transcutaneous bilirubin determination based on skin color determined by a neonatal skin color scale of our own
European Journal of Pediatrics (2021)
-
TcB, FFR, phototherapy and the persistent occurrence of kernicterus spectrum disorder
Journal of Perinatology (2020)
-
How skin anatomy influences transcutaneous bilirubin determinations: an in vitro evaluation
Pediatric Research (2019)