Abstract
Hypertension is a major risk factor for ischemic heart disease and stroke. We estimated prevalence, awareness, treatment, and control of hypertension along with its determinants in India. We used data from the National NCD Monitoring Survey-(NNMS-2017-2018) which studied one adult (18–69 years) from a representative sample of households across India and collected information on socio-demographic variables, risk factors for NCDs and treatment practices. Blood pressure was recorded digitally and hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg or currently on medications. Awareness was defined as being previously diagnosed with hypertension by a health professional; on treatment as taking a dose of medication once in the last 14 days and; control as SBP < 140 mmHg and DBP < 90 mmHg. Multivariate Logistic regression was performed to estimate determinants. Out of 10,593 adults with a blood pressure measurement (99.4%), 3017 (28.5%; 95% CI: 27.0–30.1) were found to have hypertension. Of these hypertensives, 840 (27.9%; 95% CI: 25.5–30.3) were aware, 438 (14.5%; 95% CI: 12.7–16.5) were under treatment and, 379 (12.6%; 95% CI: 11.0–14.3) were controlled. Significant determinants of awareness were being in the age group 50–69 years (aOR 2.45 95% CI: 1.63–3.69), women (1.63; 95% CI: 1.20–2.22) and from higher wealth quintiles. Those in the age group 50–69 (aOR 4.80; 95% CI: 1.74–13.27) were more likely to be under treatment. Hypertension control was poorer among urban participants (aOR 0.55; 95% CI: 0.33–0.90). Significant regional differences were noted, though without any clear trend. One-fifth of the patients were being managed at public facilities. The poor population-level hypertension control needs strengthening of hypertension services in the Universal Health Coverage package.
Similar content being viewed by others
Introduction
Hypertension is one of the most important risk factors for cardiovascular diseases (CVD), particularly ischemic heart disease and stroke [1, 2]. Currently, it is estimated that 28.1% of all deaths in India were due to CVD and, high systolic blood pressure (SBP) was the single largest contributor (8.5%) to disability-adjusted life years DALYs [3]. The World Health Organization target of a 25% relative reduction in the prevalence of high blood pressure (BP) among persons aged 18 years and older by 2025 can only be achieved by a combination of strategies that shift the population distribution of BP to the left and achieve good control of BP among those with hypertension [4, 5]. A good understanding of the cascade of hypertension of “awareness,” “treatment,” and “control” is useful to plan hypertension control strategy in a population as these have different implications [6,7,8].
Based on early experience in the United States, a rule of halves was postulated to hold with 50% of those with hypertension being aware of it, 50% of them being treated and 50% of those treated being controlled [9]. However, its universal applicability has been questioned [10]. A nationwide survey in India among 18–49 years in 2015–2016 showed that in those with high BP, 44.7% were aware of their diagnosis, 13.3% were being treated, and 7.9% had achieved control [11]. In a secondary data analysis of National Family Health Survey (NFHS 2015-16) data. the prevalence of hypertension among men aged 15–54 years was 16%. Of these hypertensive individuals, 63.2% had their BP measured earlier, 21.5% were aware of the diagnosis, 12.6% were treated and only 6.1% had controlled BP [12]. The estimated prevalence of hypertension for the Indian population aged 45 years and older, studied as a part of a longitudinal study on ageing, was 45.9%, with 55.7% of hypertension being already diagnosed, 38.9% were on antihypertensive medication and 31.7% had their BP under control [13]. A recent study in which these parameters were estimated 20 years apart in the National Capital Region of Delhi showed that there was little change in these parameters in an urban area while, the awareness, treatment and control had marginally improved in the rural population, though control of hypertension was still poorer than in urban area [14]. While these surveys provide useful information, they do not cover the age groups (18-69 years) needed for global and national monitoring efforts.
India recently strengthened its resolve to address hypertension at the population level by launching the population-based screening for hypertension (along with diabetes and the three common cancers) and strengthening primary and secondary health facilities [15, 16]. The National NCD Monitoring Survey (NNMS) in 2017–2018 was conducted to monitor the progress of the NCD monitoring indicators [17]. This paper presents the results related to hypertension cascade—prevalence, awareness, treatment and control.
Materials and methods
The NNMS was conducted in 2017–2018 in covering a total of 300 rural (village) and 300 urban (ward) clusters, selected by multi-stage stratified random sample, and 20 households were selected in each of the clusters using systematic random sampling (Supplementary Fig. 1a). In each selected household, one adult member (18–69 years) was selected for the study. The details of the survey process including the selection of households and individuals and study tools have been published earlier [17]. The survey was implemented by ten regional partner institutions and followed standard operating procedures and training protocols. Automatic BP machines (OMRON HEM–7120, Omron Corporation, Kyoto, Japan) were used with regular calibration being done at the study sites.
Information collected were household-level data on socioeconomic status, fuel and cooking oil use, individual-level data on demographic details, socio-behavioral risk factors for NCDs; diagnosis and treatment-seeking for hypertension, diabetes and CVD. Anthropometric (height, weight, and waist circumference), BP and blood glucose measurements were also carried out on the participant selected for the survey. BP was recorded in the left arm in a seated position after resting the person for 5–10 min. Three readings were taken at least 5 min apart.
The definitions used for BP followed standard recommendations of the World Hypertension League Expert Committee [8]. The proportion of participants who reported their BP being checked at least once by a physician or a health worker in their lifetime were labeled as ever measured. High BP was defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg (based on the mean of the 2nd and 3rd measurements of BP based on the minimum percentage regression to mean (SBP: 5.8% and DBP: 9.9%) compared to other two measurement combination) or the participants who reported being currently on medications for raised BP or who reported having been diagnosed with hypertension by a health professional. The participants with high BP who reported having been diagnosed with hypertension by a health professional or who report taking medication for high BP were classified as being aware. The proportion of participants with hypertension who reported taking medication for high BP on any of the last 2 weeks before the survey day were considered to be on treatment. Hypertension control was defined as having an SBP < 140 mmHg and DBP < 90 mmHg. Presence of concomitant behavioral risk factors [current smoked or smokeless tobacco use, ever intake of alcohol and hazardous drinking (more than 6 standard drinks in a single drinking occasion in last 30 days), physical inactivity (less than 600 MET-minutes in a week), dietary salt restriction practices] co-morbidities (diabetes, hypercholesterolemia or, CVD), increased body mass index and increased waist circumference (≥90 cm in males and ≥80 cm in females), treatment-seeking practices, adherence to medication (number of days medication taken in last 14 days categorized into three groups 1–5 days, 6–10 days and 11 or more days) and source of drugs for hypertension (government/ others) were all explored as determinants of hypertension control and for estimation of crude and adjusted odds ratio and 95% CI.
The survey was done using an offline android-based application, Open Data Kit. The finalized forms, after review by the team leader for completion, were uploaded at the end of the day or the survey cluster. Data was cleaned in SPSS Version 22.0 and weighted for adjusting sample, population proportions and response rates to provide nationally representative prevalence estimates at the population level. The information on household possession of select assets was used to calculate the wealth index of all surveyed households and divided into quintiles. Final weighted data was analyzed in STATA 14.1 by complex survey analysis and the population estimates of hypertension treatment cascade are presented as proportion with 95% confidence intervals (CIs). These proportions and 95% CI were derived for different subgroups of age, sex, years of education, profession, wealth index quintiles, region, place of residence (urban or rural). Participants were categorized based on the regions of the country in which their state was present—Central (Uttar Pradesh, Chhattisgarh, Madhya Pradesh); East (Bihar, West Bengal, Jharkhand, Odisha); North (Jammu and Kashmir, Himachal Pradesh, Punjab, Chandigarh, Uttarakhand, Haryana, Delhi, Rajasthan); South (Andhra Pradesh, Karnataka, Kerala, Tamil Nadu); West (Gujarat, Maharashtra); and North-East (Sikkim, Nagaland, Manipur, Mizoram, Assam) [18].
Multivariate logistic regression was performed to estimate adjusted odds ratios with their 95% CI with every measurement, prevalence, awareness, treatment and control of hypertension as dependent variables and the above variables as an independent. We also compared the management practices reported by the subjects with hypertension (source of treatment and medicines, receipt of advice on lifestyle management and level of adherence to medications) by place of residence.
Results
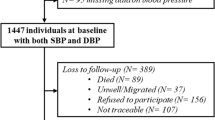
A total of 10,659 individuals provided complete information in the NNMS survey (96.3%), of which 10,593 had their BP measured (99.4%). Total males were 5490 (99.1%), 5103 were females (99.7%), urban adults were 3538 (99.1%) and 7055 rural adults (99.5%) (Supplementary Fig. 1b). Of the total adults, 3017 (28.5%; 95% CI: 27.0–30.1) were found to have high BP based on their BP measurement values and for reported history of being treated for hypertension. Of them, 840 (27.9%; 95% CI: 25.5–30.3) were aware of their hypertension status, 438 (14.5%; 95% CI: 12.7–16.5) were under treatment for hypertension and, 379 (12.6%; 95% CI: 11.0–14.3) had their BP under control. (Fig. 1).
Among the surveyed adults, 47.6% (95% CI: 45.2–50.0) reported having their BP measured ever in their lifetime (Table 1). This was significantly more among women as compared to men (aOR 1.92; 95% CI: 1.59–2.32), among those aged >30 years as compared to those between 18–30 years. The BP measurement showed a clear socioeconomic patterning with those educated beyond sixth class or those not working or professionals or people in higher wealth index being significantly more likely to have their BP measured. Adults living in southern India (aOR 2.41; 95% CI: 1.88–3.09) were more likely to have their BP measured, while the rural-urban differences ceased to be significant after adjustment.
Women were less likely to have high BP (aOR 0.82; 95% CI: 0.71–0.95) as were people in the lower age brackets (Table 1). Education and occupation were not found to be significant determinants of high BP. Those belonging to the highest wealth quintiles (Q5) had a significantly higher prevalence of high BP (aOR:1.35, 95% CI: 1.05–1.72). People in the northern (aOR 1.52; 95% CI: 1.20–1.93) and southern (aOR 1.35; 95% CI: 1.10–1.66) India were more likely to have high BP as compared to those in the central region. Urban residents were also found to have significantly high BP (aOR 1.29; 95% CI: 1.10–1.51) as compared to rural ones.
Table 2 presents the data on the awareness, treatment and control rates among those with hypertension and their determinants. Awareness of their high BP status was higher among those aged 50–69 years (aOR 2.45; 95% CI: 1.63–3.69); among women (aOR 1.63; 95% CI: 1.20–2.22), among those not working and professionals as compared to laborers, and those in the higher wealth index groups. Those living in the western region of India were less likely to be aware of their hypertension status (aOR 0.61; 95% CI: 0.40–0.94) whereas those in the northeast were more likely to be aware of their BP status (aOR 1.71; 95% CI: 1.02–2.85). There was no significant rural-urban differences on this parameter.
There were no significant differences in the proportion of hypertensives on treatment by sex, education, occupation, wealth index, or place of residence. People aged more than 50 years (aOR 4.80; 95% CI: 1.74–13.27) or living in east (aOR 2.65; 95% CI: 1.40–5.01) South (aOR 3.01; 95% CI: 1.69–5.36) or West (aOR 3.14; 95% CI: 1.54–6.40) India had significantly higher treatment rates. People living in urban areas were less likely to have their high BP controlled as compared to the rural areas (aOR 0.55; 95% CI: 0.33–0.90).
Only one-fifth of the subjects with hypertension were being managed at (21.9%; 95% CI: 17.1–27.7) or getting their medicines (18.1%; 95% CI: 13.6–23.8) from a public health facility with no significant rural-urban differences (Table 3). There was very little utilization of the AYUSH (Ayurveda, Yoga, Unani, Siddha, and Homeopathy) system alone in the treatment of hypertension. Good adherence was measured by the reported intake of pills taken in last 2 weeks on at least 80% days (≥11 days’ intake of medicine in last 2 weeks) based on the definition given by Haynes et al. [15]. Good adherence was (70.6%; 95% CI: 63.6–76.7) being significantly higher in urban (83.2%) as compared to rural areas (59.2%). Advice by health care providers regarding behavioral modification was uniformly poor in urban and rural areas. Dietary advice (49.7%) and reducing salt intake (41.6%) were the advice most often given and quitting alcohol (9%) was the least likely advice. Tobacco cessation (13.3%) and increasing physical activity (32.5) were other advice reported.
Among the hypertensives currently on treatment, those being in the age group 50–69 years (aOR 0.47; 95% CI: 0.26–0.84) and current smokeless tobacco users (aOR 0.31; 95% CI: 0.15–0.64) were less likely to have their BP controlled. Whereas those in the rural areas (aOR 2.19; 95% CI: 1.25–3.83) and those underweight (aOR 4.87; 95% CI: 1.52–15.65) were more likely to have their BP controlled (Table 4).
Sub-group analysis based on gender (male and female) and area of residence (rural and urban) was carried out for ever measured BP, prevalence of high BP, its awareness, treatment and control status was presented as Supplementary Tables 1a–d and 2a–d. In addition, determinants for control status among those who are under treatment for high BP was depicted in Supplementary Table 4a–d. Age group, level of education and wealth index was found to be significant determinants for prevalence, awareness and treatment of high BP.
Discussion
This nationally representative study from India found low levels of awareness, treatment, and control of hypertension among adults. In the hypertension cascade, the biggest drops were seen at the awareness and treatment stage. Only 28% of those with high BP were aware of it and 52% of those aware were on treatment. Most of the patients with hypertension on treatment had good adherence and were under control. Key differentials by rural-urban, wealth index and geographical regions were noted.
Women were more likely to have their BP measured (perhaps owing to ante-natal care services) as compared to men. However, the probability of treatment and control did not vary by gender. Mohanty et al., based on an analysis of the NFHS 2015-16, reported that women above 45 years had higher levels of awareness, treatment, and control of hypertension than their male counterparts [19]. Other surveys have also confirmed this [11, 13]. While not statistically significant, our study reported higher treatment rates among women and lower control rates, maybe due to the lower age profile of the participants.
The study highlighted the socioeconomic patterning of the disease. The gap between the lowest and highest wealth quintile was larger for awareness (17.3% vs. 41.8%) and narrower for control (9.4% vs. 16.6%). However, neither treatment nor control of hypertension was determined by the wealth index. Other studies have confirmed the pro-rich inequalities in hypertension awareness, treatment and control [11, 13, 19]. In pooled data from nationally representative studies in low-income and middle-income countries (LMICs), being a woman, older, more educated, wealthier, and not being a current smoker were all positively associated with attaining each of the four steps of the care cascade [20].
The regional and rural-urban differences have been reported from many previous studies [6, 11, 13]. These reflect the differences in the prevalence of different behavioral, risk factors like tobacco use and diet, urbanization levels, socioeconomic differences as well as the organization of health services. Regional differences in the international context have also been reported globally with Latin American and Caribbean countries doing better than sub-Saharan Africa and Asia [20]. These reviews show that improvements in the detection, treatment and control of hypertension have varied substantially across countries, with some middle-income countries now outperforming most high-income nations [20, 21].
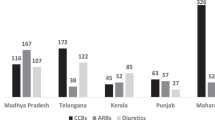
Control of BP is influenced both by the population and patient-level factors as well as limitations within the healthcare system [22]. Weak health systems have been identified as major bottlenecks in effectively responding to the rising burden of chronic conditions in LMIC, including India [23]. India has a mixed health care system, with a predominant share by the private sector which is largely unregulated and poorly coordinated, which have posed significant challenges in addressing chronic NCDs adequately [24, 25]. Health facility component of the current study (NNMS)) has well-documented significant gaps in both private and public primary care facilities and public secondary facilities in the availability of essential medicines, technologies, training of available manpower and counseling services of the health system response to NCDs in India. Our efforts have focused on strengthening primary and secondary public health facilities by improving the availability of key medicines for hypertension [26]. The India Hypertension Control Initiative [27], has demonstrated a substantial improvement of BP controls through five intervention strategies of protocol-based approach, ensuring drug availability of a small list of drugs, patient-centric care provision and cohort monitoring enabled by the use of technology of the HEARTS technical package [28]. Currently, this initiative does not include the private sector and an exploratory study involving private practitioners as a part of IHCI in Bhopal (Central part of India) showed that there were major constraints in terms of limited availability of single component hypertension drugs, preferences for fixed-dose combinations, and fear of losing patients to others. In addition, none of the interviewed doctors had resources to provide patient-centered care and use a digital health information system [29] It will be important to address these challenges if we want to achieve better population control of hypertension.
This study provides valuable insight for strategizing for the same and a good template to monitor progress in this regard. Strengths and limitations: The strengths of the study are its national scope, focus on NCD risk factors, good quality assurance, use of standard definitions, large sample size, weighted proportions, high response rates as well as coverage of age group used for global monitoring and linkage to national efforts. Limitations were a single day measurement of BP and adherence to treatment being based on reported medication intake and not on any standard tool or pill counting methods. Other limitations of the survey were challenges in arriving at State-based estimates, since the study sample was nationally representative in line with the specific objectives for generating baseline evidence on risk factors and health-seeking behaviors as per the National NCD Monitoring Framework for India.
Summary table
What is already known
-
Population-level hypertension control is poor in many developed as well as developing countries.
-
Urban-rural, gender, poor-rich differentials exist in hypertension control cascade.
What this study adds to existing knowledge
-
Poor control of Hypertension in India is mainly due to poor awareness of hypertension and inadequate treatment-seeking.
-
There exists gender, economic and regional differentials in awareness, treatment and control of hypertension.
-
Only 1 in 5 persons with hypertension seeks treatment in the public sector.
-
The study identifies population-based screening and health system strengthening including involvement of the private sector as key interventions to improve population-level control of hypertension.
Data availability
All the data are available within the manuscript. The National Noncommunicable Disease Monitoring Survey (NNMS) report is available at https://www.ncdirindia.org/nnms/.
Change history
02 August 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41371-022-00727-4
References
Gupta R, Xavier D. Hypertension: the most important non communicable disease risk factor in India. Indian Heart J. 2018;70:565–72. https://doi.org/10.1016/j.ihj.2018.02.003.
Prabhakaran D, Jeemon P, Sharma M, Roth GA, Johnson C, Harikrishnan S, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health. 2018;6:e1339–51. https://doi.org/10.1016/S2214-109X(18)30407-8.
Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, et al. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390:2437–60. https://doi.org/10.1016/S0140-6736(17)32804-0.
World Health Organization. 2013–2020 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Geneva, Switzerland; 2013. https://www.who.int/nmh/global_monitoring_framework/en/.
Gupta R, Gaur K, S Ram CV. Emerging trends in hypertension epidemiology in India. J Hum Hypertens. 2019;33:575–87. https://doi.org/10.1038/s41371-018-0117-3.
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7. https://doi.org/10.1097/HJH.0000000000000146.
Wozniak G, Khan T, Gillespie C, Sifuentes L, Hasan O, Ritchey M, et al. Hypertension control cascade: a framework to improve hypertension awareness, treatment, and control. J Clin Hypertens. 2016;18:232–9. https://doi.org/10.1111/jch.12654.
Gee ME, Campbell N, Sarrafzadegan N, Jafar T, Khalsa TK, Mangat B, et al. Standards for the uniform reporting of hypertension in adults using population survey data: recommendations from the World Hypertension League Expert Committee. J Clin Hypertens. 2014;16:773–81. https://doi.org/10.1111/jch.12387.
Wilber JA. The problem of undetected and untreated hypertension in the community. Bull N Y Acad Med. 1973;49:510–20.
Marques-Vidal P, Tuomilehto J. Hypertension awareness, treatment and control in the community: is the ‘rule of halves’ still valid? J Hum Hypertens. 1997;11:213–20. https://doi.org/10.1038/sj.jhh.1000426.
Prenissl J, Manne-Goehler J, Jaacks LM, Prabhakaran D, Awasthi A, Bischops AC, et al. Hypertension screening, awareness, treatment, and control in India: a nationally representative cross-sectional study among individuals aged 15 to 49 years. PLoS Med. 2019;16:e1002801. https://doi.org/10.1371/journal.pmed.1002801.
Kothavale A, Puri P, Yadav S. The burden of hypertension and unmet need for hypertension care among men aged 15-54 years: a population-based cross-sectional study in India. J Biosoc Sci. 2021:1–22. https://doi.org/10.1017/S0021932021000481.
Lee J, Wilkens J, Meijer E, Sekher TV, Bloom DE, Hu P. Hypertension awareness, treatment, and control and their association with healthcare access in the middle-aged and older Indian population: a nationwide cohort study. PLoS Med. 2022;19:e1003855. https://doi.org/10.1371/journal.pmed.1003855.
Roy A, Praveen PA, Amarchand R, Ramakrishnan L, Gupta R, Kondal D, et al. Changes in hypertension prevalence, awareness, treatment and control rates over 20 years in National Capital Region of India: results from a repeat cross-sectional study. BMJ Open. 2017;7:e015639. https://doi.org/10.1136/bmjopen-2016-015639.
National Programs. National Programme for Prevention and Control of Cancer Diabetes Cardiovascular diseases and Stroke (NPCDCS). Ministry of Health and Family Welfare. Government of India; 2021. https://main.mohfw.gov.in/Major-Programmes/non-communicable-diseases-injury-trauma/Non-Communicable-Disease-II/National-Programme-for-Prevention-and-Control-of-Cancer-Diabetes-Cardiovascular-diseases-and-Stroke-NPCDCS.
Government of India. Population based screening. 2021. https://dghs.gov.in/content/1363_3_NationalProgrammePreventionControl.aspx.
Mathur P, Kulothungan V, Leburu S, Krishnan A, Chaturvedi HK, Salve HR, et al. National Noncommunicable Disease Monitoring Survey (NNMS) in India: estimating risk factor prevalence in adult population. PLoS ONE. 2021;16:e0246712. https://doi.org/10.1371/journal.pone.0246712.
International Institute for Population Sciences (IIPS) and ICF. 2017. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai: IIPS; 2021. https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf.
Mohanty SK, Pedgaonkar SP, Upadhyay AK, Kämpfen F, Shekhar P, Mishra RS, et al. Awareness, treatment, and control of hypertension in adults aged 45 years and over and their spouses in India: a nationally representative cross-sectional study. PLoS Med. 2021;18:e1003740. https://doi.org/10.1371/journal.pmed.1003740.
Geldsetzer P, Manne-Goehler MJ, Marcus ME, Ebert C, Zhumadilov Z, Wesseh CS, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet. 2019;394:652–62. https://doi.org/10.1016/S0140-6736(19)30955-9.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80. https://doi.org/10.1016/S0140-6736(21)01330-1.
Frieden TR, Varghese CV, Kishore SP, Campbell NR, Moran AE, Padwal R, et al. Scaling up effective treatment of hypertension—a pathfinder for universal health coverage. J Clin Hypertens. 2019;21:1442–9. https://doi.org/10.1111/jch.13655.
Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, et al. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376:1785–97. https://doi.org/10.1016/S0140-6736(10)61353-0.
Bhojani U, Devedasan N, Mishra A, De Henauw S, Kolsteren P, Criel B. Health system challenges in organizing quality diabetes care for urban poor in South India. PLoS ONE. 2014;9:e106522. https://doi.org/10.1371/journal.pone.0106522.
Lall D, Engel N, Devadasan N, Horstman K, Criel B. Challenges in primary care for diabetes and hypertension: an observational study of the Kolar district in rural India. BMC Health Serv Res 2019;19:44. https://doi.org/10.1186/s12913-019-3876-9.
Krishnan A, Mathur P, Kulothungan V, Salve HR, Leburu S, Amarchand R, et al. Preparedness of primary and secondary health facilities in India to address major noncommunicable diseases: results of a National Noncommunicable Disease Monitoring Survey (NNMS). BMC Health Serv Res. 2021;21:1–12. https://doi.org/10.1186/s12913-021-06530-0.
Kaur P, Kunwar A, Sharma M, Mitra J, Das C, Swasticharan L, et al. India Hypertension Control Initiative—hypertension treatment and blood pressure control in a cohort in 24 sentinel site clinics. J Clin Hypertens. 2021;23:720–9. https://doi.org/10.1111/jch.14141.
World Health Organization. Hearts: technical package for cardiovascular disease management in primary health care. Geneva; 2016. https://www.who.int/cardiovascular_diseases/hearts/Hearts_package.pdf.
Krishna A, Pathni AK, Sharma B, Shivashankar R, Shrivastava S, Hering D. A perspective of private health care providers in the state of Madhya Pradesh on adopting key strategies of the India hypertension control initiative. J Clin Hypertens. 2020;22:1321–7. https://doi.org/10.1111/jch.13944.
Acknowledgements
We acknowledge the support and facilitation provided by the Ministry of Health and Family Welfare, the Government of India, the Indian Council of Medical Research and the World Health Organization (India office). We also thankful the NNMS–National Technical Working Group experts for their valuable suggestions and scientific input and all the ICMR-NNMS investigators and collaborators.
Funding
This study was funded by the Ministry of Health and Family Welfare (MoHFW), Govt of India (Dy.No.C-707, dated 06 July 2015). The funders only provided the funds and had no role in the study planning implementation and preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
AK, PM, RA and VK contributed to the concept and design of the paper. RA and AK developed the analysis plan. VK and PM reviewed and finalized the analysis plan. VK was involved in data management and statistical analyses. RA drafted the manuscript with expert review and inputs from AK, PM and VK. RA, AK, VK and PM were involved in the revision of the manuscript and approved the final version of the manuscript. RA and AK were one of the study site investigators and PM and VK were part of the central coordinating unit primarily involved in the investigation. PM received funding for the study and was the central principal investigator. All the authors were part of the expert core group of the central coordinating unit.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Institutional Ethics Committee of ICMR—National Centre for Disease Informatics and Research, Bengaluru which was the coordinating center as well as one of the survey’s implementing agencies (approval no: NCDIR/IEC/2017/4 dated 03 February 2017). Every implementing agency obtained its ethics approval from its own Institutional Ethics Committee before starting the survey. All selected study participants were informed about the visit and purpose of the survey. Following their voluntary acceptance to participate, written informed consent was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Due to an error in the text.
Supplementary information
41371_2022_692_MOESM1_ESM.docx
Supplementary files: Figure 1a, Figure 1b, Table 1a, Table 1b, Table 1c, Table 1d, Table 2a, Table 2b, Table 2c, Table 2d, Table 4a, Table 4b, Table 4c, Table 4d
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amarchand, R., Kulothungan, V., Krishnan, A. et al. Hypertension treatment cascade in India: results from National Noncommunicable Disease Monitoring Survey. J Hum Hypertens 37, 394–404 (2023). https://doi.org/10.1038/s41371-022-00692-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00692-y
This article is cited by
-
Recent studies on hypertension prevalence and control in India 2023
Hypertension Research (2024)
-
Predictors of Control Status of Hypertension in India: A Systematic Review and Meta-analysis
Journal of Prevention (2024)
-
Sociodemographic and geographic inequalities in diagnosis and treatment of older adults’ chronic conditions in India: a nationally representative population-based study
BMC Health Services Research (2023)
-
Hypertension care cascade in an urban resettlement colony and slum in Delhi, India: a cross-sectional survey
BMC Public Health (2023)
-
Trends in hypertension prevalence, awareness, treatment, and control: an 8-year follow-up study from rural North India
Scientific Reports (2023)