Abstract
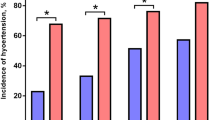
The purpose of this study was to examine the impact that the revised American College of Cardiology/American Heart Association (ACC/AHA) hypertension diagnostic criteria would have on the prevalence of metabolic syndrome (MBS) among college students. Students completed an objective health assessment between September 2015 and April 2018 that involved the assessment of abdominal girth, blood glucose, lipids, and blood pressure (BP). Data of 5681 students (60.1% Men; 21 ± 1 years) who had all MBS risk factors assessed were analyzed to compare differences between old and new diagnostic criteria and identify which component of BP best predicts metabolic risk factors. The prevalence of MBS increased by 40.6% and 104.5% with the change to ACC/AHA criteria from the AHA/National Heart Lung and Blood Institute and the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High BP criteria, respectively. The greatest relative increase in the prevalence of MBS was observed among women. Systolic BP and diastolic BP were significant predictors of abdominal obesity, and diastolic BP was a significant predictor of elevated triglycerides. Changes in hypertension diagnostic criteria had a significant impact on MBS prevalence. This is positive as it will allow earlier identification of young adults at risk of developing various noncommunicable diseases, but the ability of colleges to identify and then intervene to improve the health of at-risk students remains unclear. Furthermore, findings indicate that BP may hold utility as a cost-effective predictor of certain metabolic risk factors in the absence of efficient, accurate, and affordable alternatives.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
22 July 2020
This Article has been updated since publication in order to correct Table 4 and reformat the other Tables. We would like to apologise for these errors.
References
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20.
Alberti KGMM, Eckel Robert H, Grundy Scott M, Zimmet Paul Z, Cleeman James I, Donato Karen A, et al. Harmonizing the metabolic syndrome. Circulation. 2009;120:1640–5.
ACSM, Riebe D, Ehrman JK, Liguori G, Magal M. ACSM’s guidelines for exercise testing and prescription. 10th ed. Philadelphia, PA: Wolters Kluwer; 2018.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112:2735–52.
Morrell JS, Lofgren IE, Burke JD, Reilly RA. Metabolic syndrome, obesity, and related risk factors among college men and women. J Am Coll Health. 2012;60:82–9.
Morrell JS, Byrd-Bredbenner C, Quick V, Olfert M, Dent A, Carey GB. Metabolic syndrome: comparison of prevalence in young adults at 3 land-grant universities. J Am Coll Health. 2014;62:1–9.
Whelton PK, Carey RM, Aronow WS, Casey Jr DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115.
Kamara K, Wilson OWA, Papalia Z, Bopp M, Bopp CM. Comparison of college student hypertension prevalence between the JNC7 and ACC/AHA diagnostic criteria. Int J Exerc Sci. 2019;12:898–903.
Berenson GS, Wattigney WA, Tracy RE, Newman WP, Srinivasan SR, Webber LS, et al. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (the Bogalusa Heart Study). AM J Cardiol. 1992;70:851–8.
McGill Henry C, McMahan CA, Zieske Arthur W, Sloop Gregory D, Walcott Jamie V, Troxclair Dana A, et al. Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. Arterioscler Thromb Vasc Biol. 2000;20:1998–2004.
Stary HC. Evolution and progression of atherosclerotic lesions in coronary arteries of children and young adults. Arteriosclerosis. 1989;9(Suppl 1):I19–32.
Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med. 1998;338:1650–6.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–71.
Parikh P, Mochari H, Mosca L. Clinical utility of a fingerstick technology to identify individuals with abnormal blood lipids and high-sensitivity C-reactive protein levels. Am J Health Promot. 2009;23:279–82.
Wilson OWA, Kamara K, Papalia Z, Bopp M, Bopp CM. Changes in hypertension diagnostic criteria enhance early identification of at risk college students. Transl J Am Coll Sports Med. 2020;5:1–5.
Kuk JL, Ardern CI. Age and sex differences in the clustering of metabolic syndrome factors: association with mortality risk. Diabetes Care. 2010;33:2457–61.
Wilson OWA, Graupensperger S, Bopp M, Evans MB. The temporal association between physical activity and fruit and vegetable consumption: a longitudinal within- and between-person investigation. J Phys Act Health. 2019;16:274–80.
Moore JX, Chaudhry N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev Chronic Dis. 2017;14.
Wilson OWA, Zou ZH, Papalia Z, Bopp M, Bopp CM. Comparison of obesity classification methods among college students. Obes Res Clin Pr Title. 2019;14:430–4.
Acknowledgements
The authors would like to acknowledge the students who allowed the use of their data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wilson, O.W.A., Garra, S., Bopp, M. et al. Incorporating the American College of Cardiology/American Heart Association hypertension diagnostic criteria into metabolic syndrome criteria will significantly increase the prevalence of metabolic syndrome among college students. J Hum Hypertens 35, 517–523 (2021). https://doi.org/10.1038/s41371-020-0369-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0369-6