Abstract
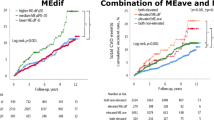
To investigate the effect of night-time BP-lowering drug treatment on the risk of major CVD and mortality, we systematically reviewed randomized controlled trials comparing night-time versus morning dosing. Two studies were found relevant to the clinical question (the MAPEC and Hygia trials). They were similar in study design and population and were conducted by the same study group. As the Hygia trial had more power with a significantly larger sample size, we did not perform a meta-analysis. Both studies reported a reduction of ~50% in major CVD events and all-cause mortality with night-time dosing and a reduction of 60% in CVD mortality. The results from these studies support the implementation of night-time BP-lowering drug treatment in the prevention of CVD and mortality. However there is an on-going discussion on the validity and methodology of MAPEC and Hygia trials, the interpretation of the results should be cautious. Stronger evidence is needed prior to changing clinical practice. Questions that remain to be answered relate to the generalisability of the results across different populations at different levels of BP related risk and the importance of morning versus evening timing of medication on CVD prevention as determined though a well-designed randomised controlled trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Williams B, Mancia G, Spiering W, Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Salles GF, Reboldi G, Fagard RH, Cardoso CRL, Pierdomenico SD, Verdecchia P, et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the ambulatory blood pressure collaboration in patients with hypertension (ABC-H) meta-analysis. Hypertension. 2016;67:693–700.
Grimaldi D, Provini F, Calandra-Buonaura G, Barletta G, Cecere A, Pierangeli G, et al. Cardiovascular-sleep interaction in drug-naive patients with essential grade I hypertension. Chronobiol Int. 2013;30:31–42.
Kario K, Shimada K. Risers and extreme‐dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens. 2004;26:177–89.
Brotman DJ, Davidson MB, Boumitri M, Vidt DG. Impaired diurnal blood pressure variation and all-cause mortality. Am J Hypertens. 2008;21:92–97.
Fagard R, Thijs L, Staessen JA, Clement D, De Buyzere M, De Bacquer D. Night–day blood pressure ratio and dipping pattern as predictors of death and cardiovascular events in hypertension. J Hum Hypertens. 2009;23:645–53.
Sobiczewski W, Wirtwein M, Gruchała M, Kocić I. Mortality in hypertensive patients with coronary heart disease depends on chronopharmacotherapy and dipping status. Pharm Rep. 2014;66:448–52.
Smolensky MH, Portaluppi F. Chronopharmacology and chronotherapy of cardiovascular medications: Relevance to prevention and treatment of coronary heart disease. Am Heart J. 1999;137:S14–S24.
Redfern, Peter H, Lemmer B, Andreotti F, Redfern PH & Lemmer B. Physiology and pharmacology of biological rhythms. Springer Berlin Heidelberg:Imprint: Springer. 1997.
Reinberg A, Smolensky M. Circadian changes of drug disposition in man. Clin Pharmacokinetics. 1982;7:401–20.
Zhao P, Xu P, Wan C, Wang Z. Evening versus morning dosing regimen drug therapy for hypertension. Cochrane Database of System Rev. 2011. https://doi.org/10.1002/14651858.CD004184.pub2. Accessed 22 December 2020.
Gupta R, Malik AH, Popli T, Ranchal P, Yandrapalli S, Aronow WS. Impact of bedtime dosing of antihypertensives compared to morning therapy: a meta-analysis of randomised controlled trials. Eur J Prevent Cardiol. 2020:2047487320903611. https://doi.org/10.1177/2047487320903611. [Epub ahead of print].
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350:757–64.
Liu L, Wang JG, Gong L, Liu G, Staessen JA. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. J Hypertens. 1998;16:1823–9.
Tatti P, Pahor M, Byington RP, Mauro PD, Guarisco R, Strollo G, et al. Outcome results of the Fosinopril Versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDM. Diabetes Care. 1998;21:597–603.
Black HR, Elliott WJ, Grandits G, Grambsch P, Lucente T, White WB, et al. principal results of the controlled onset verapamil investigation of cardiovascular end points (CONVINCE) trial. J Am Med Assoc. 2003;289:2073–82.
Black HR, Elliott WJ, Neaton JD, Grandits G, Grambsch P, Grimm RH, et al. Rationale and design for the Controlled ONset Verapamil INvestigation of Cardiovascular Endpoints (CONVINCE) Trial. Control Clin Trials. 1998;19:370–90.
Lefebvre C, Manheimer E, Glanville J. Chapter 6.4. 11.1 The cochrane highly sensitive search strategies for identifying randomized trials in MEDLINE. Cochrane handbook for systematic reviews of interventions version. 5.
Higgins JPT, Sterne JAC, Savović J, Page MJ, Hróbjartsson A, Boutron I et al. A revised tool for assessing risk of bias in randomized trials In: Chandler J, McKenzie J, Boutron I, Welch V (editors). Cochrane Methods. Cochrane Database of Systematic Reviews. 2016(10).
Ayala DE, Hermida R, Mojon A, Fernandez JR. Influence of class and treatment-time regimen of hypertension medications on the risk of developing chronic kidney disease. J Hypertens. 2015;1:e457.
Ayala DE, Hermida RC, Mojon A, Fernandez JR. Cardiovascular risk of resistant hypertension: dependence on treatment-time regimen of blood pressure-lowering medications. Chronobiol Int. 2013;30:340–52.
Hermida RC. Use of >= 1 antihypertensive drug at bedtime reduced CV events more than use of all drugs in the morning in CKD. Ann Intern Med. 2012;156:JC6–JC8.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of time of day of blood pressure–lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care. 2011;34:1270–6.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629–51.
Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. European Heart J. 2019. https://doi.org/10.1093/eurheartj/ehz754.
Hermida RC. Sleep-time ambulatory blood pressure as a prognostic marker of vascular and other risks and therapeutic target for prevention by hypertension chronotherapy: rationale and design of the Hygia Project. Chronobiol Int. 2016;33:906–36.
Luo Y, Ren L, Jiang M, Chu Y. Anti-hypertensive efficacy of amlodipine dosing during morning versus evening: a meta-analysis. Rev Cardiovasc Med. 2019;20:91–98.
Wang C, Ye Y, Liu C, Zhou Y, Lv L, Cheng C, et al. Evening versus morning dosing regimen drug therapy for chronic kidney disease patients with hypertension in blood pressure patterns: a systematic review and meta-analysis. Intern Med J. 2017;47:900–6.
Liu X, Huang W, Leo S, Li Y, Liu M, Yuan H. Evening-versus morning-dosing drug therapy for chronic kidney disease patients with hypertension: a systematic review. Kidney Blood Press Res. 2014;39:427–40.
Wing LM, Chowdhury EK, Reid C, Beilin LJ, Brown MA. Night-time ambulatory blood pressure is the best pretreatment blood pressure predictor of 11-year mortality in treated older hypertensives. Blood Press Monit. 2018;23:237–43.
Yano Y, Kario K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertension Res. 2012;35:695–701.
Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011;57:3–10.
Glasziou P, Doust J. In patients with hypertension, taking all BP-lowering drugs at bedtime vs in the morning reduced CV events. Ann Intern Med. 2020;172:JC29–JC29.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J hypertension. 2002;20:2183–9.
Palatini P, Verdecchia P, Beilin LJ, Eguchi K, Imai Y, Kario K, et al. Association of extreme nocturnal dipping with cardiovascular events strongly depends on age. Hypertension. 2020;119:14085. HYPERTENSIONAHA
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Carlberg B, Brunstrom M. Is Bedtime the best time of the day? ISH Hypertension News Web site. https://ish-world.com/data/uploads/2003-9.pdf. Published 2020. Accessed 2020.
Kreutz R, Kjeldsen SE, Burnier M, Narkiewicz K, Oparil S, Mancia G. Blood pressure medication should not be routinely dosed at bedtime. We must disregard the data from the HYGIA project. Blood Press. 2020;29:135–36.
Lemmer B, Middeke M. A commentary on the Spanish hypertension studies MAPEC and HYGIA. Chronobiol Int. 2020;37:728–30.
Hermida RC, Hermida RC. Ambulatory blood pressure monitoring in the prediction of cardiovascular events and effects of chronotherapy: rationale and design of the MAPEC study. Chronobiol Int. 2007;24:749–75.
Rorie DA, Rogers A, Mackenzie IS, Ford I, Webb DJ. Willams Bryan et al. Methods of a large prospective, randomised, open-label, blinded end-point study comparing morning versus evening dosing in hypertensive patients: the Treatment In Morning versus Evening (TIME) study. BMJ Open. 2016;6:e010313.
Carter BL, Chrischilles EA, Rosenthal G, Gryzlak BM, Eisenstein EL, Vander, et al. Efficacy and safety of nighttime dosing of antihypertensives: review of the literature and design of a pragmatic clinical trial. J Clin Hypertens (Greenwich). 2014;16:115–21.
Pierdomenico SD, Bucci A, Costantini F, Lapenna D, Cuccurullo F, Mezzetti A. Circadian blood pressure changes and myocardial ischemia in hypertensive patients with coronary artery disease. J Am Coll Cardiol. 1998;31:1627–34.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7.
Suzuki Y, Kuwajima I, Aono T, Kanemaru A, Nishinaga M, Shibata H, et al. Prognostic value of nighttime blood pressure in the elderly: a prospective study of 24-hour blood pressure. Hypertension Res. 2000;23:323–30.
Pierdomenico SD, Pierdomenico AM, Coccina F, Lapenna D, Porreca E. Circadian blood pressure changes and cardiovascular risk in elderly-treated hypertensive patients. Hypertension Res. 2016;39:805–11.
Acknowledgements
The researchers gratefully acknowledge NHMRC Centre of Research Excellence in Cardiovascular Outcomes Improvement for their support of this project. CMR is supported by a NHMRC Principal Research Fellowship (1136372). We thank Prof Hermida for his kind support on the enquiries related to MAPEC and Hygia trial. We thank Dr Jun Chih (Biostatisticician, School of Public Health, Curtin University) for her advise on statistical issues.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ho, C.L.B., Chowdhury, E.K., Doust, J. et al. The effect of taking blood pressure lowering medication at night on cardiovascular disease risk. A systematic review. J Hum Hypertens 35, 308–314 (2021). https://doi.org/10.1038/s41371-020-00469-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-00469-1
This article is cited by
-
Non-Dipping Blood Pressure or Nocturnal Hypertension: Does One Matter More?
Current Hypertension Reports (2024)
-
Arterial Hypertension—clinical trials update 2023
Hypertension Research (2023)
-
Advances in Clinical Cardiology 2022: A Summary of Key Clinical Trials
Advances in Therapy (2023)